Thyroid surgery
All content is checked by medical journalists.Thyroid surgery is usually understood to mean the partial or total removal of the thyroid gland (thyroidectomy). This is necessary, for example, in the case of cancer or an enlarged thyroid. Read everything about the course of thyroid surgery, when it is used and what risks it entails.

What is thyroid surgery?
Doctors also refer to thyroid surgery as a thyroidectomy or thyroidectomy. Depending on the underlying disease of the patient, a distinction is made between various thyroid surgery procedures:
- Removal of a lump (enucleation)
- Removal of most of the thyroid gland (subtotal thyroid surgery)
- Removal of a thyroid lobe (hemithyroidectomy)
- Complete removal of the thyroid gland (thyroidectomy)
In addition to these surgical techniques, there are also minimally invasive thyroid operations, in which the thyroid gland is removed using a probe and only the smallest incisions are necessary. Minimally invasive thyroid operations at specialized centers currently account for around ten percent.
When do you have a thyroid operation?
The most common reason for a thyroid removal is malignant neoplasms. Even if a lump in the thyroid gland is discovered, about the benignness or malignancy of which no reliable statement can be made, an operation must be carried out. Other reasons for thyroid surgery are:
- Enlargement of the thyroid gland, possibly with narrowing of the surrounding organs (goiter)
- Uncontrolled production of thyroid hormones
- Severe course of Graves' disease (autoimmune hypothyroidism)
- Massive metabolic imbalance in hyperthyroidism (thyrotoxic crisis)
What do you do during thyroid surgery?
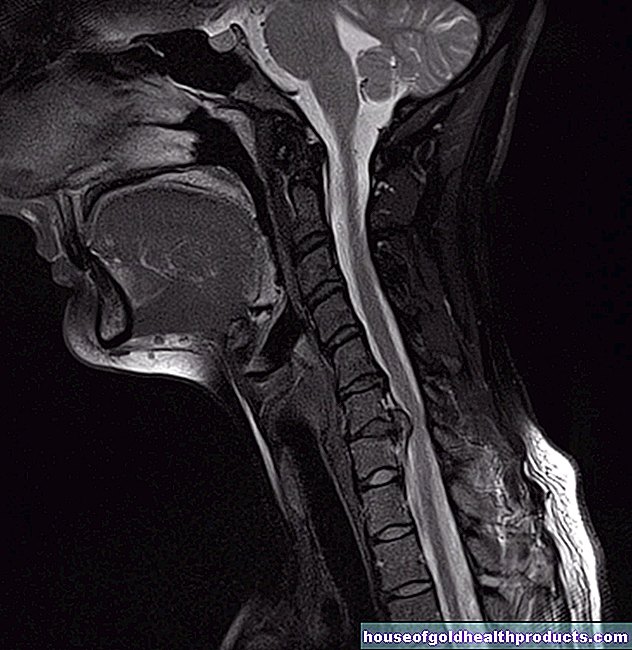
The thyroid is located on the neck below the larynx. It consists of two flaps that are connected by a tissue bridge (isthmus). It is enclosed by a connective tissue capsule. A healthy thyroid weighs around 15 to 20 grams.
Before thyroid surgery
The patient is given general anesthesia so that he or she spends the procedure asleep and pain-free. The doctor generously disinfects the surgical field and covers the patient with sterile cloths, leaving out the anterior neck region. Then the surgeon can begin the actual thyroid removal. If necessary, he monitors the surrounding nerves with the help of a so-called neuromonitoring system - if he touches a nerve with the surgical instrument, a warning signal sounds.
Total thyroidectomy
Total thyroidectomy is used, for example, to remove goiter (goiter surgery, strumectomy, goiter resection) and to remove large cancerous ulcers. The surgeon usually makes an incision four to five centimeters long. If possible, he looks for a skin fold to achieve a better cosmetic result. The doctor then cuts through the fatty tissue layer with electric scissors, which immediately stop any bleeding. If the thyroid is exposed, the surgeon will separate it from the surrounding tissue.
The doctor can now remove the entire thyroid gland, leaving the parathyroid glands if they can be found. The parathyroid glands are only about the size of a grain of rice and can be located in different places in the throat. If the surgeon finds the parathyroid glands only when examining the removed thyroid, he will replant them into an artificially created pocket in the neck muscles. There the parathyroid can start working again.
Hemithyroidectomy
In a hemithyroidectomy, only one of the two thyroid lobes is removed. It is also used for goiter surgery, but also for unilateral cancerous ulcers. Access is the same as for a total thyroidectomy. If the doctor has a good view of the exposed thyroid lobe, he cuts the connective tissue bridge that connects the two lobes.
Enucleation
Enucleation is used to remove small, benign nodules. The surgeon makes a small incision through which he carefully gains access to the knot. He then removes it with ultrasonic scissors or an electric knife.
Subtotal thyroid surgery
The subtotal thyroid resection is a rather rare procedure and is usually only used when independently hormone-producing cells are distributed throughout the thyroid. The surgeon removes large parts of the thyroid, but spares the healthy thyroid tissue.
After thyroid surgery
After the thyroid has been removed, the doctor first sutures the muscle and fat layers with self-dissolving sutures, then also sutures the skin incision as tension-free as possible in order to prevent unsightly scarring. The wound is bandaged with sterile plasters. The patient is then taken to the recovery room, where he can recover from the anesthesia.
What are the risks of thyroid surgery?
Thyroid surgery is a routine surgical procedure. However, as with any operation, complications can arise. Possible consequences of the operation can be:
- Secondary bleeding, possibly with surgical removal of the bruise
- Wound healing disorder
- Infection of the operating area
- Cosmetically unsatisfactory result with clear scarring
Injury to nerves
Thyroid removal can damage important nerves that run near the thyroid. If the so-called recurrent nerve is injured on one side of the neck, it can lead to a slight hoarseness. The rare bilateral severing of the nerve leads to shortness of breath, and the patient may have to be artificially ventilated.
Damage or accidental removal of the parathyroid glands
The parathyroid glands release a hormone and thus control the calcium balance. Calcium is important for the functioning of nerves and muscles and it stabilizes the bones. The stress of thyroid surgery can impair the function of the parathyroid glands and reduce calcium levels. Usually the parathyroid glands recover and the calcium balance normalizes. If this does not happen, the body must be supplied with the missing calcium in tablet form.
What do I have to consider after a thyroid operation?
As with any surgery, wound pain can occur in the first few days after the procedure. If necessary, your doctor will prescribe pain reliever medication. In order to protect the wound, you should wash yourself only with the exception of the neck region or with a special shower plaster.
Hormone replacement therapy after thyroid surgery
When the thyroid is removed, the body lacks the hormones triiodothyronine and thyroxine it produces. These must be supplied permanently after the complete thyroid operation. Your doctor will prescribe tablets for you to take every day. After four to six weeks, he checks the hormone level in the blood and adjusts the dose to your individual needs. If only part of the thyroid gland is removed during your thyroid surgery, hormone intake is usually not necessary.
Tags: prevention palliative medicine pregnancy birth