Henoch-Schönlein purpura
Dr. med. Mira Seidel is a freelance writer for the medical team.
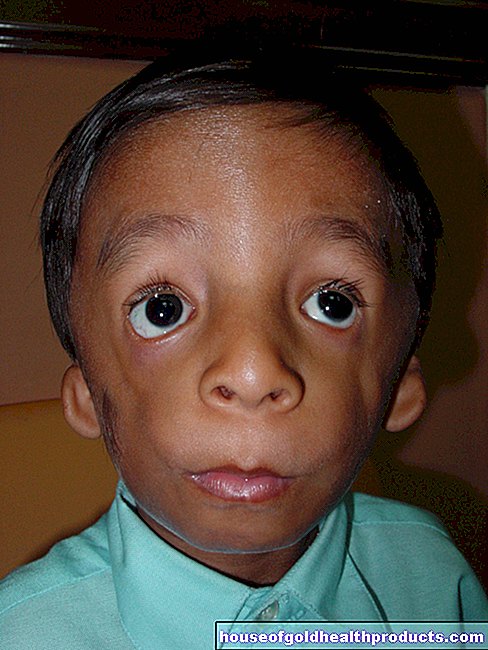
More about the experts All content is checked by medical journalists.Henoch-Schönlein purpura (purpura anaphylactoides, vasculitis allergica) is an immunologically induced inflammation of the small blood vessels. Typical symptoms are punctiform hemorrhages in the skin (petechiae), cramp-like abdominal pain and joint pain. Henoch-Schönlein purpura occurs in young children and school children and is usually triggered by a previous infection or medication. Here you can read everything you need to know about Henoch-Schönlein purpura.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D69
Henoch-Schönlein purpura: description
Henoch-Schönlein purpura (anaphylactoid purpura, vasculitits allergica) is an inflammation of the small blood vessels and capillaries triggered by the immune system. In technical jargon, such inflammation is called vasculitis. Henoch-Schönlein purpura is the most common form of vasculitis in young children and school children and affects children under ten years of age in 90 percent of cases. Infants and adolescents are rarely affected.
In Henoch-Schönlein purpura, the small vessels of the skin, the joints, the gastrointestinal tract and the kidneys are particularly affected. The disease often occurs after a previous upper respiratory tract infection or other triggers such as medication. The blood vessels become more permeable over time due to the inflammation, which leads to punctiform bleeding (petechiae) in the skin. In addition, there is usually swelling on the back of the feet, hands and joints. Suddenly, children with Henoch-Schönlein purpura no longer want to walk. The children also often suffer from abdominal pain, vomiting and diarrhea. In some cases, Henoch-Schönlein purpura develops kidney inflammation (glomerulonephritis).
The disease begins acutely and progresses in phases. As a rule, it heals without serious consequences.
The Purpura Schönlein-Henoch was named after the German doctors Johann Lukas Schönlein and Eduard Heinrich Henoch.
Henoch-Schönlein purpura: symptoms
In the case of Henoch-Schönlein purpura, small skin bleeding is in the foreground. However, the internal organs can also be affected, usually accompanied by a slight fever. The onset is usually sudden. The children complain of symptoms such as headaches, loss of appetite, and cramping abdominal pain. The symptoms appear in bursts.
The main symptoms of Henoch-Schönlein purpura affect different parts of the body:
Henoch-Schönlein purpura: skin
The skin is always involved in Henoch-Schönlein purpura and shows punctiform, sometimes extensive, intertwining skin bleeding. The skin bleeding can be felt, but not pushed away. They mostly occur on the extensor sides of the lower legs and on the buttocks. They are also rarely found on the lower abdomen, on the extensor surfaces of the upper extremities and in boys in the testicular area. The skin lesions can be different. Often times, Henoch-Schönlein purpura begins as individual skin hemorrhages with a diameter of one to three millimeters, which then flow together and appear as an extensive hemorrhage. Most of the skin bleeding occurs symmetrically and does not itch.
In children under two years of age, another variant of Henoch-Schönlein purpura can appear. It is referred to as "acute infantile hemorrhagic edema" or 2Seidlmayer corkard purple ". The typical skin bleeding can be found here both in the area of the arms and legs as well as the skin of the face.
Henoch-Schönlein purpura: joints
About 65 percent of children with Henoch-Schönlein purpura show a sudden onset of painful swellings and restricted mobility, especially in the ankle and knee joints (rheumatic purpura). Usually both sides of the body are affected. Parents then notice that their child “suddenly can no longer walk”.
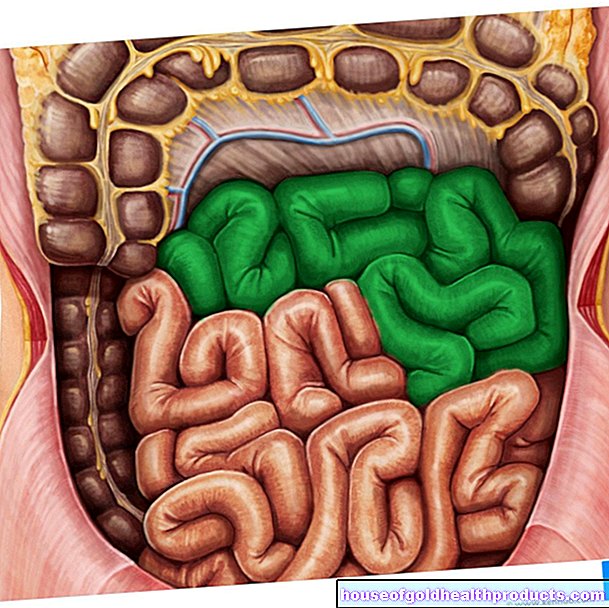
Henoch-Schönlein purpura: gastrointestinal tract
Colic abdominal pain, but also bloody stool (purpura abdominalis) and diarrhea can be caused by the inflammation of the small intestinal vessels. The gastrointestinal tract is affected in half of children with Henoch-Schönlein purpura. Vomiting and bloody stools can indicate an invagination of the intestinal loops (intussusception).
Henoch-Schönlein purpura: kidney
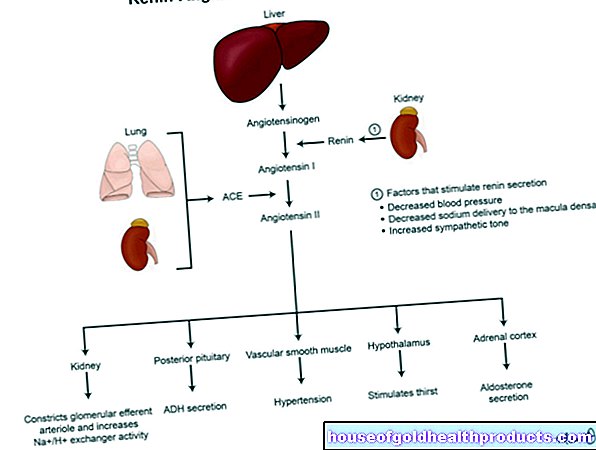
After one to two weeks there may be visible or invisible blood in the urine (macro- or microhematuria). This affects at least 30 percent of children with Henoch-Schönlein purpura. Excretion of protein in the urine (proteinuria), increased blood pressure and impaired kidney function are also possible. Such kidney involvement is called Henoch-Schönlein nephritis.
Henoch-Schönlein purpura: Central nervous system
The cerebral vessels are very rarely affected in Henoch-Schönlein purpura. Headaches, behavior disorders, seizures, paralysis and impaired consciousness can then occur.
Henoch-Schönlein purpura: testicles
In Henoch-Schönlein purpura there is rarely inflammation of the testicles (orchitis): the testicles are painful and swollen. It is important to rule out testicular torsion (rotation of the testicle and spermatic cord around the longitudinal axis), as this can lead to infertility if left untreated.
Henoch-Schönlein purpura: complications
Complications with Henoch-Schönlein purpura are very rare and only occur sporadically. In a so-called fulminant form, symmetrical, flat skin bleeding suddenly occurs. Most of these bleeding blisters develop, which eventually become necrotic (tissue destruction). With this variant of Henoch-Schönlein purpura, the child can suffer a life-threatening shock.
Another complication that can occur with Henoch-Schönlein purpura is the invagination of the intestine.
In the case of Henoch-Schönlein nephritis, the kidneys can later develop again. Kidney function deteriorates in the process.
Women who have already suffered from Henoch-Schönlein purpura are more prone to kidney problems during pregnancy.
Henoch-Schönlein purpura: causes and risk factors
The exact cause of Henoch-Schönlein purpura is unknown. Almost 80 percent of the cases are based on medicinal, viral and bacterial triggers. Presumably there is an immunological reaction after infections of the upper respiratory tract, such as with influenza A viruses (flu pathogens) or β-hemolytic streptococci.
Most drugs can cause Henoch-Schönlein purpura, but above all antibiotics, anti-inflammatory drugs (anti-inflammatory drugs such as cortisone and non-steroidal anti-inflammatory drugs) and drugs that promote water excretion (thiazides). Other triggers such as insect bites, vaccinations, hyposensitizations or certain diseases of the immune system such as connective tissue diseases (collagenoses), liver diseases and malignant tumors are also possible. Sometimes Henoch-Schönlein purpura occurs for no apparent reason.
Henoch-Schönlein purpura: inflammation of the blood vessels
The antibodies, which are so-called immunoglobulins A (IgA), are deposited on the vessel walls in Henoch-Schönlein purpura. IgA immune complexes are formed, which trigger an inflammatory reaction (complement activation) and can lead to the destruction of the small vessels not only in the skin, but also in the gastrointestinal tract and kidneys. The vascular damage results in blood leaking into the surrounding connective tissue and triggering the typical bleeding. An inflammatory reaction of a blood vessel is known in technical terms as vasculitis. It is also known as a type III allergy (Arthus reaction).
Henoch-Schönlein purpura: contagious?
Since Henoch-Schönlein purpura is an autoimmune inflammation of the blood vessels, this disease is not contagious. No precautionary measures need to be observed.
Henoch-Schönlein purpura: examinations and diagnosis
If you suspect Henoch-Schönlein purpura, it is advisable to present your child to a pediatrician. This can determine whether the rash is actually Henoch-Schönlein purpura or another disease.
the characteristic symptoms as well as other examination methods and laboratory values.
Medical history and physical examination
There is no specific laboratory value for Henoch-Schönlein purpura that allows a clear diagnosis. However, the doctor can determine the disease in other ways. To do this, he first determines the medical history (anamnesis). Possible questions from the pediatrician could include:
- Since when does your child have punctiform skin bleeding?
- Does your child have joint pain and / or a fever?
- Has your child recently had a cold?
- Have you noticed movement restrictions while playing or exercising?
- Does your child complain of stomach ache or nausea?
- Have you noticed blood in the child's stool or urine?
- Does your child have diarrhea?
This is followed by a physical exam. The pediatrician pays particular attention to the characteristic skin appearance of Henoch-Schönlein purpura. A skin biopsy is only required if the findings are unclear. If the typical appearance of Henoch-Schönlein purpura is shown, this is not necessary. A histological (histological) evidence can confirm Henoch-Schönlein purpura.
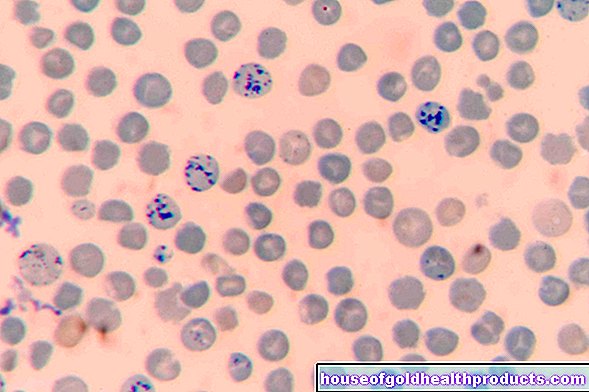
Blood test
Inflammation parameters, such as the rate of sedimentation and the C-reactive protein, are determined in a blood sample from the child. These are usually only slightly increased in Henoch-Schönlein purpura.
In addition, the coagulation factors should be determined to determine whether there is a possible deficiency in coagulation factor XIII, as this can cause a tendency to bleeding.
To rule out other forms of vascular inflammation, immunoglobulins (Ig), antinuclear antibodies (ANA) and antineutrophil cytoplasmic antibodies (ANCA) are examined. For Henoch-Schönlein purpura, ANA and ANCA are negative.
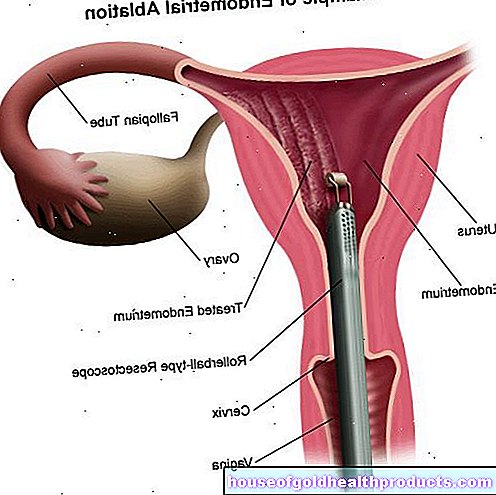
Urine and kidney studies
A urine test may indicate kidney involvement. If the values for protein (proteinuria) and red blood cells (hematuria) are elevated, glomerulonephritis may be present.
If there are signs of kidney involvement over a long period of time or if the affected child quickly deteriorates kidney function, the doctor takes a tissue sample from the kidney (kidney biopsy).
Stool examination
If a child with Henoch-Schönlein purpura is suspected of having vascular bleeding in the gastrointestinal tract, a test for hidden (occult) blood in the stool (hemoccult test, guaiac test) can provide an indication.
Ultrasonic
The ultrasound examination for abdominal pain is used to determine bleeding in the intestinal wall and whether there is a possible intussusception. In addition, the affected joint, the kidneys and, in boys, the testicles are examined using ultrasound.
Examination of the brain
If it is suspected that the central nervous system is also affected by the vascular inflammation, magnetic resonance imaging (MRI) of the head is usually done.
Exclusion diagnostics
Based on the clinical examination and laboratory results, the doctor will try to rule out other diseases such as coagulation disorders, sepsis, septic arthritis, and other forms of vascular inflammation.
Henoch-Schönlein purpura: treatment
In children with Henoch-Schönlein purpura, the symptoms usually improve on their own and therapy is not necessary. A hospital stay is only advisable in the case of a complicated course with abdominal pain, fever, painful joint problems, poor general condition as well as children under two years of age and adults (a severe course is possible).
The complaints can be treated symptomatically. For pain, the doctor will prescribe acetaminophen or nonsteroidal anti-inflammatory drugs such as ibuprofen or naproxen. If the intestine is affected, cortisone preparations are also used. Cortisone has anti-inflammatory effects and slows down the excessive reaction of the immune system. Usually, cortisone is given for a week and then the dosage is slowly reduced over a period of one to two weeks (“tapering off” of the cortisone therapy).
Treatment of severe Henoch-Schönlein purpura
If the kidneys are involved, the so-called creatinine level in the urine provides information about the severity of Henoch-Schönlein nephritis. Creatinine is a breakdown product of creatine that serves as an energy reserve in the muscles.
If the creatinine level is slightly increased for six weeks (less than two grams of creatinine per gram of urine: 2g / g), high-dose cortisone preparations are possible. These are given over a period of about twelve weeks, with the dosage gradually being reduced again in the last few weeks (“tapering off”).
In connection with kidney involvement, it can lead to increased blood pressure. In this case, the doctor will adjust your child's blood pressure with medication. He will also recommend that you have your child's kidney function checked regularly for up to two years after Henoch Schönlein nephritis.
Henoch-Schönlein purpura: disease course and prognosis
Henoch-Schönlein purpura usually heals on its own after a few days. If the course is severe, skin and soft tissue necroses (dying tissue parts) can form, which heal spontaneously with scarring. The healing process can then take between four and six weeks. In very rare cases, Henoch-Schönlein purpura leads to terminal kidney failure.
Tags: alcohol drugs foot care smoking