Endometrial ablation
Valeria Dahm is a freelance writer in the medical department. She studied medicine at the Technical University of Munich. It is particularly important to her to give the curious reader an insight into the exciting subject area of medicine and at the same time to maintain the content.
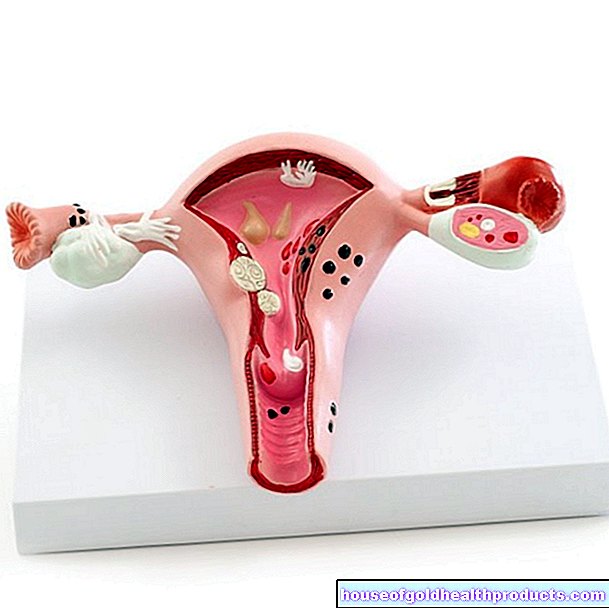
More about the experts All content is checked by medical journalists.With endometrial ablation, the uterine lining is obliterated and permanently removed by means of high heat. The most common reason for an endometrial ablation is menstrual disorders that cannot be treated with medication. Read all about endometrial ablation, how it works, and what the risks are.

What is an endometrial ablation?
With endometrial ablation, the mucous membrane of the uterus is obliterated to the muscles by very high levels of heat. The treated tissue dies. In rare cases, strong cold is used. This counteracts a renewed build-up of the mucous membrane in the monthly cycle and thus reduces the menstrual period to a normal level or even prevents it completely. Endometrial ablation is the less complicated alternative to surgical removal of the uterus (hysterectomy). A distinction is made between first and second generation procedures.
First generation process
- Resection with the resection loop: Current is passed through a wire loop and heats it up
- Coagulation with the roller ball electrode: Current is passed through a spherical attachment and heats it up
- Laser ablation with an ND: YAG laser: Lasers obliterate the mucous membrane
Second generation process
- Hydrothermal ablation: fluid is pumped into the uterus and heated there strongly
- Bipolar mesh (NovaSure, gold mesh method): a mesh is stretched inside the uterus and heated strongly
- Microwave Ablation: Microwave energy is delivered to the mucous membrane through a probe
- Uterine balloon methods (Thermachoice): a balloon at the end of a catheter is inserted into the uterus and filled with hot fluid
When to do an endometrial ablation
Endometrial ablation is performed if:
- Difficult-to-treat bleeding disorders such as heavy menstrual bleeding with normal bleeding duration (hypermenorrhea) or excessive menstrual bleeding with prolonged bleeding duration (menorrhagia)
- Bleeding disorders under long-term anticoagulant therapy
- as an alternative to surgical removal of the uterus (hysterectomy)
This bleeding can be triggered by hormonal imbalances, benign growths (polyps, fibroids) or tumors. Endometrial ablation is only performed when family planning has been completed, as the malformation rate in newborns is significantly increased. It is not a method of birth control (contraception).
Endometrial ablation is not used in the case of malignant changes in the uterus (carcinoma) or precursors to cancer.
What do you do with an endometrial ablation?
Ablation is a minimally invasive procedure that requires only the smallest injuries to the skin and soft tissues. As with any operation, a few standard examinations - such as an EKG and a blood sample - are carried out beforehand. In addition, there is in-depth personal advice and information from the attending doctor. An anesthetist explains the general anesthesia.
Every endometrial ablation is preceded by a scraping with a tissue examination in the laboratory for fibroids, polyps or preliminary stages of malignant changes. Giving hormones (GnRH = gonadotropin releasing hormone) before the operation thins the uterine lining and can shorten the duration of the operation and improve the result.
At the beginning of the operation, the surgeon uses a hysteroscopy to obtain a direct view of the uterus in order to rule out malignant changes, for example. The vagina forms the natural access route for the hysteroscope.
The most common method of endometrial ablation is a combination of loop resection and roller-ball coagulation. First, the surgeon removes the larger areas of the anterior, posterior and side walls of the uterus with the loop, then sclerosing the upper part (fundus uteri) and the corners of the fallopian tubes (tube) with the rollerball. The instruments in this first-generation procedure are inserted through the vagina and removed again at the end of the treatment.
In the meantime, second-generation processes are becoming more and more popular. They are easier to use and there are few complications. In the uterine balloon method, a folded plastic balloon is inserted into the uterine cavity and inflated with fluid. If the liquid is heated, the lining of the uterus dies within a few minutes. With the gold net method, a net is stretched inside the uterus and the mucous membrane is obliterated with high-frequency electricity.
What are the risks of ablation?
In addition to the general risks of surgery, such as infection, specific complications can arise. However, since endometrial ablation is a gentle procedure, these are rare.
- Piercing the wall of the uterus
- Wound healing disorders
- Post-endometrial ablation syndrome: the walls stick together and the uterus accumulates blood
- Injury to neighboring organs
- Recurrence of the treated disease
What should I watch out for after an endometrial ablation?
The discharge usually takes place several hours - rarely days - after the procedure.Before this, you will be examined in detail and you will have a final discussion with your treating doctor about further measures.
Your doctor will advise you that, despite endometrial ablation, there is still a possibility of pregnancy and that contraceptive measures are urgently required. Since an egg cell could implant itself in small islands of the mucous membrane, malformation rates are significantly increased after an endometrial ablation.
In the first few days after the operation, there may be bleeding from the wound and a brownish discharge. You should avoid swimming, bathing, sexual intercourse, tampons and sauna visits for three weeks, as the cervix is still a little open. After three, six and twelve months, and later every year, a follow-up sonography and an evaluation of the bleeding calendar should be carried out so that the success of the therapy can be assessed.
If the bleeding problems recur, another endometrial ablation or removal of the uterus (hysterectomy) may be necessary.
Tags: hair Diseases magazine