penicillin
Updated onSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.Penicillin is one of the antibiotics. These are substances that act against microorganisms - especially bacteria. According to this, penicillin is used to treat bacterial infections. In general, it can also be used by pregnant women, breastfeeding women and small children. Depending on the chemical structure, a distinction is made between different types of penicillin. Read here what these are, how penicillin works and what side effects it can cause!

What is penicillin?
Penicillin is a medicine that is made from cultures of brush mold Penicillium chrysogenum (old name: P. notatum) is obtained. In addition to penicillin, which occurs naturally in mold, there are also semi-synthetic or fully synthetic (artificially produced) forms of this active ingredient.
Penicillin is one of the antibiotics. This is understood to mean active ingredients that are primarily effective against bacteria and are therefore used against bacterial infections.
The terms antibiotics and penicillin are often used synonymously. In fact, penicillins are only a subgroup of antibiotics. Other representatives of antibiotics are, for example, macrolides, aminoglycosides and carbapenems.
When is penicillin used?
Penicillin is used against infections with sensitive germs. Important areas of application for penicillin are, for example:
- Tonsillitis (tonsillitis)
- Otitis media
- Inflammation of the sinuses (sinusitis)
- bronchitis
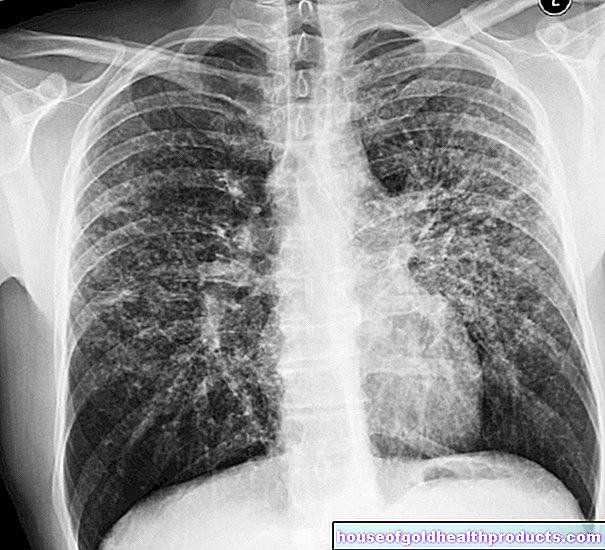
- Inflammation of the lungs (pneumonia)
- Scarlet fever
- Meningitis
- Inflammation of the lining of the heart (endocarditis)
- Urinary tract infections
- Biliary tract infections
- Inflammation of the bones (osteomyelitis)
- Rheumatic fever
- syphilis
- Gonorrhea (gonorrhea)
- Listeriosis
- Typhoid and Paratyphoid
- Bacterial dysentery (shigellosis)
- "Blood poisoning" (sepsis)
In some cases, different penicillins (see below) can be considered for the treatment of the various diseases. Sometimes the antibiotics are also prescribed preventively (e.g. before an operation).
What penicillins are there?
There are many different penicillins that differ in their chemical structure. The natural penicillin that Alexander Fleming discovered is the so-called penicillin G.
In order to expand the spectrum of action and to circumvent resistance, further variants have been developed over the decades. They are manufactured partially or fully synthetic.
Important penicillins are:
- Penicillin F (penicillin I; δ2-pentenylpenicillin)
- Penicillin G (Penicillin II; Benzylpenicillin)
- Penicillin X (penicillin III; p-hydroxybenzyl penicillin)
- Penicillin K (penicillin IV; n-heptylpenicillin)
- Penicillin V (phenoxymethylpenicillin)
- Penicillin O (allyl mercaptomethylpenicillin)
- Dihydroflavicin (n-amylpenicillin)
A distinction is made between narrowband and broadband penicillins according to the spectrum of activity.
Narrow band penicillins
Narrow-band penicillins are primarily effective against gram-positive bacteria. This group of active substances includes:
- Penicillin G and long-term depot penicillins such as benzathine-benzylpenicillin (a hardly water-soluble salt of penicillin G): They are acid-labile and must therefore be administered intravenously (as a syringe or infusion). If given by mouth (orally), stomach acid would break them down.
- Oral penicillins: These are acid-resistant and can therefore be administered orally. These include penicillin V, propicillin, and azidocillin (the latter two are no longer available today).
- Beta-lactamase-resistant penicillins: They were developed to fight bacteria that produce the enzyme beta-lactamase - this can make certain antibiotics ineffective (see below: Penicillin resistance). Examples of beta-lactamase-resistant penicillins are oxacillin, dicloxacillin and flucoxacillin.
Broad spectrum penicillins
Broad spectrum penicillins are not only effective against gram-positive, but also against some gram-negative types of bacteria. These active ingredients include:
- Aminopenicillins: ampicillin, amoxicillin
- Acylaminopenicillins: Mezlocillin, Piperacillin
- Carboxypenicillins: They are no longer used today.
Those penicillins that are not resistant to the bacterial enzyme beta-lactamase are usually used as a combination preparation together with a beta-lactamase inhibitor, for example:
- Amoxicillin with clavulanic acid
- Ampicillin with sulbactam
- Piperacillin with tazobactam
How does penicillin work?
Penicillin belongs to the group of beta-lactam antibiotics. All representatives of this group have a so-called beta-lactam ring in their chemical structure.
In doing so, they inhibit a bacterial enzyme (D-alanine transpeptidase), which is required for the construction of the bacterial cell wall. As a result, as the bacterial cell divides further, the cell wall becomes unstable and tears - the bacterium dies.
The penicillin action (i.e.the effect of all beta-lactam antibiotics) on dividing pathogens is therefore bactericidal (bactericidal).
Penicillin has no effect on bacteria that are already fully grown, i.e. in which cell division no longer takes place. These bacteria are neutralized by the immune system.
Penicillin is primarily effective against gram-positive bacteria (such as streptococci) and against some gram-negative bacteria (such as meningococci). Gram is a dye that is used in the microscopic examination of bacteria. Depending on whether the examined bacterium accepts the dye (gram-positive) or not (gram-negative), the doctor initiates a suitable antibiotic therapy.
Penicillin Resistance
The penicillin discoverer Sir Alexander Fleming warned of the danger that bacteria could become resistant through the excessive use of penicillin. This means that the microorganisms change over time in such a way that they become insensitive to the active ingredient - they develop defense strategies against it.
In relation to penicillin, this defense strategy involves the enzyme beta-lactamase, which some types of bacteria produce. With this enzyme, the germs can override the beta-lactam ring of penicillin - and thus the bactericidal penicillin effect.
Such resistances are promoted by various factors. Penicillin, for example, is often taken too briefly or in too low a dose. Then some bacteria in the patient's body can survive the treatment and pass on their "experience" with the active ingredient.
Over time, resistance can develop in subsequent generations of bacteria. The unnecessary use of broad spectrum penicillins - penicillins that act against many different bacteria - can also promote resistance.
Experts therefore recommend using pathogen-specific penicillins (narrow-band penicillins) as far as possible. Last but not least, penicillins should only be used for infections that cannot be controlled otherwise.
This is how penicillin is used
Penicillins are usually taken orally (e.g. as penicillin tablets) or administered directly into a vein (intravenously) (as an injection or infusion). Some preparations (depot penicillins) are injected into a muscle.
Oral preparations contain acid-resistant penicillins such as azidocillin or penicillin V, which cannot be broken down by stomach acid. Non-acid-resistant penicillins such as penicillin G, on the other hand, must be administered bypassing the stomach (parenterally) so that they can develop their effect (e.g. as an infusion).
The dosage depends on the active ingredient, the type of illness and the individual characteristics of the patient (height, weight, etc.). It is determined by the doctor and should be strictly adhered to.
Duration of application
A common rule for penicillin tablets is: take until the prescribed pack is empty - even if the symptoms have subsided before then. However, current studies show that a shorter treatment seems to be at least as promising for some infections.
In any case, patients should not decide for themselves how long to use a penicillin drug, but should always stick to the duration of use recommended by the doctor. This is the only way to ensure that the medication can work properly.
What are the side effects of penicillin?
Penicillins are generally very well tolerated. But they make no difference between "bad" bacteria (the invading pathogens) and the "good" bacteria in the intestine (intestinal flora), which are important for digestion, among other things.
Accordingly, nausea, vomiting, and diarrhea are possible penicillin side effects. Other undesirable effects that can occur are dizziness, confusion, and impaired vision and hearing.
Penicillin allergy
Penicillins can cause allergic reactions. It is believed that this happens in 0.5 to 2 percent of treatments.
A penicillin allergy can manifest itself in different ways. The symptoms range from reddened skin or swelling to anaphylactic shock, which can lead to death within minutes. Signs of anaphylactic shock include shortness of breath, burning or itching in the throat, feeling hot, and a drop in blood pressure.
A so-called pseudo-allergy must be differentiated from the penicillin allergy. Symptoms during the treatment are similar to those of an allergic reaction (e.g. reddened skin or swelling), but are actually side effects of the drug.
Penicillin allergies do not always last for life
Studies show that people who have had an allergic reaction to penicillin do not necessarily persist with the allergy. The next time you take penicillin, there may be no allergic reaction.
For this reason, a skin test (prick test) and a blood test should always be carried out before penicillin is given, even for patients classified as allergic. In this way, one can rule out the possibility that alleged allergy sufferers, who are actually no longer so, receive another drug instead of the well-tolerated and highly effective penicillin, which may be less suitable for the treatment.
What should be considered when using penicillin?
Contraindications
Penicillins should not be used if there is hypersensitivity to the respective active ingredient. In addition, if you are hypersensitive to penicillin, you should be aware of the risk of cross-allergies.
There are also other contraindications for some penicillins. Some examples:
- Amoxicillin and amoxicillin / clavulanic acid are contraindicated in infectious mononucleosis (Pfeiffer glandular fever) and lymphatic leukemia.
- Flucloxacillin is contraindicated in infectious mononucleosis (Pfeiffer glandular fever), lymphatic leukemia, jaundice (jaundice) and liver dysfunction after previous administration of flucloxacillin.
Interactions
With the simultaneous use of penicillin and other drugs, interactions can occur. For example, penicillin enhances the effects of methotrexate, a drug used to treat cancer and various autoimmune diseases such as rheumatoid arthritis.
In addition, penicillins can increase the effect of the drugs phenprocoumon and warfarin, which are prescribed as anticoagulants when there is a risk of thrombosis.
Before prescribing penicillin, doctors always clarify whether and which other drugs a patient is using.
Basically, experts recommend completely avoiding alcohol during antibiotic treatment. Because both the antibiotic and the alcohol are broken down by the liver, which puts a double burden on the detoxification organ. This can lead to side effects or make them worse. In addition, the body is weakened by the infection and the immune system is working at full speed. Alcohol puts even more stress on the organism, which can delay healing.
Many antibiotics are incompatible with milk, as its constituents prevent the active substances from being absorbed in the intestine. But this does not apply to penicillins. Milk and dairy products can usually be combined with it without any problems.
However, there are penicillins that generally have to be taken at a sufficient distance from a meal (regardless of whether it is a dairy product or not). For example, penicillin V should be taken 30 to 60 minutes before a meal.
The attending doctor or pharmacist can explain to you in more detail when and how you should take your penicillin medication.
Age restriction
Penicillin can be used to treat bacterial infections from birth.
pregnancy and breast feeding period
Penicillins are among the antibiotics of choice during pregnancy and breastfeeding. Previous observations gave no indications of a teratogenic effect.
Before each prescription, however, the doctor will always weigh the expected benefit against the theoretical risk of treatment.
Who Discovered Penicillin?
The discovery of penicillin dates back to 1928 and was a chance hit by the Scottish bacteriologist Alexander Fleming. This had a sample dish with bacteria from the strain Staphylococcus aureus forget. After returning from vacation, he discovered the mold Penicillium chrysogenum (back then P. notatum called) had displaced the bacteria. So there had to be something about this mold that was causing an antibacterial effect.
It would be ten years before the scientists Howard Florey and Ernst Boris Chain recognized the potential of the fungal active ingredient penicillin for the treatment of infectious diseases in humans. In 1945, together with Alexander Fleming, they were awarded the Nobel Prize for Medicine for their work.
Tags: foot care dental care womenshealth







.jpg)