Sarcoid
and Martina Feichter, medical editor and biologistSophie Matzik is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Sarcoid (Boeck's disease) is an inflammatory disease that can be acute or chronic. Typical features are nodular tissue changes. They can form anywhere in the body and disrupt the functioning of the organs concerned. The most common form of the disease is chronic sarcoidosis of the lungs: patients suffer from chronic dry cough and breathing difficulties. Here you can read everything you need to know about the symptoms, causes, treatment and prognosis of sarcoid.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D86
Brief overview
- What is Sarcoid? Inflammatory disease associated with the formation of nodular tissue changes. It mostly affects the lungs, but can also occur in other tissues and organs.
- Symptoms: depend on the organs affected and the course of the disease (acute or chronic). Typical signs of chronic sarcoidosis of the lungs (most common form) are increasing dry cough, stress-dependent shortness of breath and swollen lymph nodes in the lungs.
- Reason unknown. However, there are probably several factors involved in the development of the disease. In addition to genetic factors, there are also suspected harmful substances that have been inhaled.
- Therapy: not always necessary because sarcoidosis often heals on its own (especially acute sarcoidosis). However, if the symptoms are severe and / or the lung function is impaired, patients should be treated. First choice therapy is cortisone preparations.
- Prognosis: Mostly favorable, especially in acute sarcoid. The more advanced the chronic sarcoid, the worse the chances of recovery. In some patients, lung function remains impaired over the long term. About five percent of sarcoid patients die from complications.
Sarcoid: description
Sarcoid (Boeck's disease) is an inflammatory disease that can affect various organs and tissues in the body. That is why it is also known as a multi-system disease.
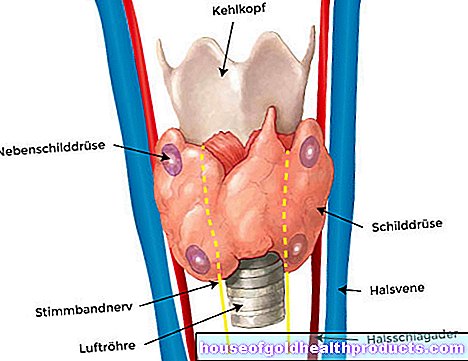
In most cases, sarcoid affects the lungs. The eyes, heart and skin are also more frequently affected. In principle, sarcoid can also show up in other parts of the body, for example in the area of the bones, kidneys, parotid and pancreas as well as in the central nervous system. The possible symptoms of Boeck's disease are correspondingly diverse.
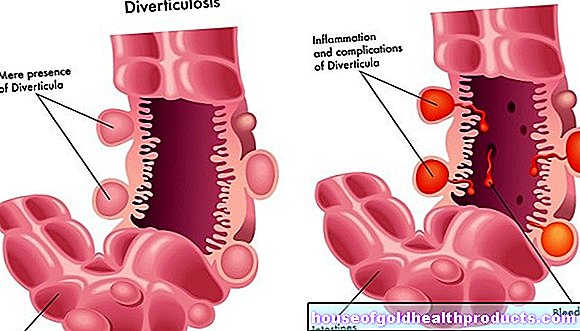
Sarcoid is one of the so-called granulomatous diseases. Their classic feature are small, nodular changes in tissue. These so-called granulomas can be seen under the microscope. It is still unclear why they develop. Doctors suspect, however, that hereditary factors combined with certain environmental factors can cause sarcoid.
Sarcoidosis: incidence
In Western Europe, it is estimated that around 40 to 50 out of 100,000 people have sarcoid. The highest incidence rates are found in Sweden and Iceland, and among people with dark skin in the United States.
The disease usually occurs between the ages of 20 and 40. Women are affected somewhat more often than men.
Sometimes children also get sarcoid. A disease up to the age of four is called "early childhood sarcoidosis" (early onset sarcoidosis, EOS or Blau syndrome). This rare form of disease is usually due to a genetic defect.
Sarcoidosis: symptoms
According to the course, doctors differentiate between acute and chronic sarcoidosis. Which symptoms occur depends on the course, the severity of the disease (sarcoid stages: see below) and the affected organs.
Acute sarcoid
Acute sarcoid makes up only about ten percent of all cases. The symptoms appear here quite suddenly. Usually the lungs are affected. Typical are:
- Fever and fatigue
- painful, initially red, later bluish nodules under the skin (erythema nodosum)
- painful swelling and inflammation of the joints (arthritis)
- Lymph node swelling in the area of both lungs
In sarcoidosis, erythema nodosum occurs primarily on the front of the lower legs. The spots are very sensitive to pain. In severe cases, the weight of clothing on the affected skin can cause pain. The skin nodules form due to inflammation of the fatty tissue just under the skin. In addition to sarcoid, possible causes of this inflammation are, for example, infectious diseases and autoimmune diseases.
Joint inflammation (arthritis) in acute sarcoid usually affects the ankles. Most of the patients experience pain when walking. Several joints can become inflamed at the same time (polyarthritis).
Swollen lymph nodes are found in acute sarcoid in the area of the main bronchi and large pulmonary vessels. This area is called the lung hili. The swellings usually do not cause any discomfort, but can be clearly seen on the X-ray. Lymph node swellings are a very typical feature of Boeck's disease. In people who do not have any other symptoms, Boeck's disease is often recognized by this "biliary lymphadenopathy" in the X-ray image alone.
Typical sarcoid symptoms
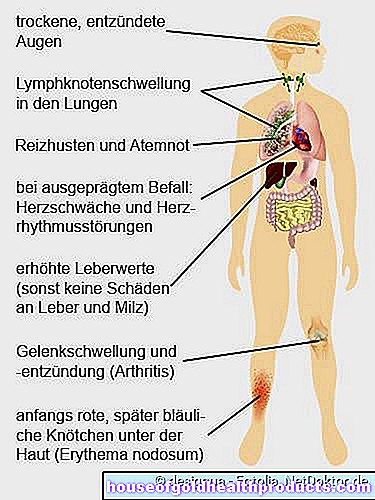
The three symptoms of lymph node swelling in the lungs, erythema nodosum and joint inflammation (arthritis) are also known as the "triad of acute sarcoid" or Löfgren's syndrome.
Chronic sarcoid
About 90 percent of all patients have chronic sarcoid. The lungs and adjacent lymph nodes are most commonly affected. Some patients are unaware of their illness. For others, the symptoms develop slowly and insidiously: increasing dry cough and stress-dependent shortness of breath. On the X-ray you can see the swollen lymph nodes in the so-called Lungenhili (biliary lymphadenopathy). Other signs of chronic sarcoidosis include:
- light fever
- Weight loss
- fatigue
- Joint pain (arthritis)
In principle, Boeck's disease can affect the entire body (extrapulmonary sarcoid). This results in different symptoms:
Sarcoid - eyes: Various structures in the eye can be affected here. In many patients, both the iris and the so-called ciliary body (on which the eye lens is suspended) are inflamed. This so-called iridocyclitis causes eye pain, which occurs mainly in bright light.
Sarcoid - Skin: Chronic sarcoid in the skin area triggers certain skin changes. These include the painful nodules under the skin (erythema nodosum) mentioned above. They tend to form on the front of the lower legs. In addition, bluish-purple discoloration of the skin (lupus pernio) can develop, especially on the cheeks and nose.
Sarcoid - Heart: The heart can be affected by sarcoid to different degrees. A slight infestation does not cause any complaints. A pronounced infestation can trigger cardiac insufficiency or cardiac arrhythmias. There is then a risk of serious complications!
Sarcoid - Kidneys: If the kidneys are affected by sarcoid, they excrete more calcium in the urine. This favors the formation of kidney stones.
Sarcoidosis - Central Nervous System (Neurosarcoidosis): Sarcoidosis rarely affects the central nervous system (brain and spinal cord). This often causes cranial nerve failure. If this affects the facial nerve, for example, the facial muscles are paralyzed as a result. This facial paralysis usually occurs on one side. Neurosarcoidosis also often leads to meningitis. Possible symptoms here are, for example, headache and vomiting.
Sarcoid - Liver and Spleen: Sarcoid of the liver and spleen does not usually cause any symptoms. The function of the two organs is practically not restricted. Only the liver values in the blood can be increased as a result of sarcoidosis of the liver.
Heerfordt syndrome: This special form of sarcoid causes inflammation of the parotid glands and the eyes as well as swollen breast lymph nodes. In addition, one half of the face can be paralyzed (facial paresis).
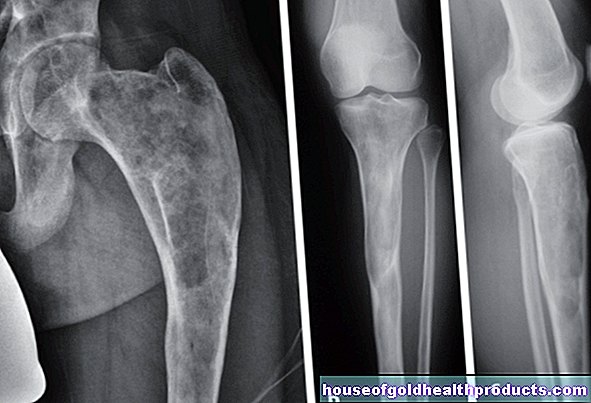
Youth syndrome (Morbus Jüngling): The term describes a chronic sarcoid in the area of the bones. The finger bones are very often affected.
The rare early childhood sarcoid (EOS) causes fewer symptoms than the disease in adulthood. The possible signs range from fever, loss of appetite, and tiredness to an enlarged liver and spleen (hepatosplenomegaly).
Sarcoidosis: causes and risk factors
The exact cause of sarcoid is unclear. However, various factors probably play a role in the development of the disease.
In most patients, sarcoid affects the lungs. Researchers therefore suspect that inhaling harmful substances activates the immune system in the lungs. This could then trigger the formation of tissue nodules (granulomas). Possible harmful substances are, for example, pollen, viruses, bacteria, fungal spores, dust and chemicals.
In addition, genetic factors are involved in the development of Boeck's disease. Scientists have discovered genes in the human genome that are often changed in sarcoid. Some of these genetic changes (mutations) have been shown to increase the risk of sarcoidosis. Presumably the affected genes have something to do with the function of the immune system. Due to their mutation, certain substances that are important for the immune system are probably no longer produced or are produced in a different form. This could trigger miscommunication in the immune system - with the result that sarcoidosis develops.
Sarcoid: examinations and diagnosis
Diagnosing sarcoid is often not easy. The symptoms can be so diverse that the disease often manifests itself very differently from patient to patient. In addition, other diseases can also be the cause of the various complaints. Therefore, several diagnostic steps are necessary before a sarcoid can be diagnosed with certainty.
The first point of contact if you suspect Boeck's disease is usually a general practitioner. If necessary, he will refer the patient to a specialist, such as a specialist in lung diseases.
First conversation
The doctor will first record your medical history (anamnesis) in a detailed discussion. Typical questions asked by the doctor in the anamnesis interview are, for example:
- Do you suffer from a dry cough?
- What other complaints do you have (skin changes, fever, etc.)?
- How long have the symptoms existed?
- Have you had symptoms like this in the past?
- Have you recently had an x-ray of the lungs?
- Did or do you have any lung diseases in your family?
Physical examination
The anamnesis will be followed by a physical examination. The main focus is on the lungs and skin. These two organs are most commonly affected by Boeck's disease.
The doctor will listen and tap your chest for example. This gives him clues about possible changes in the lungs.
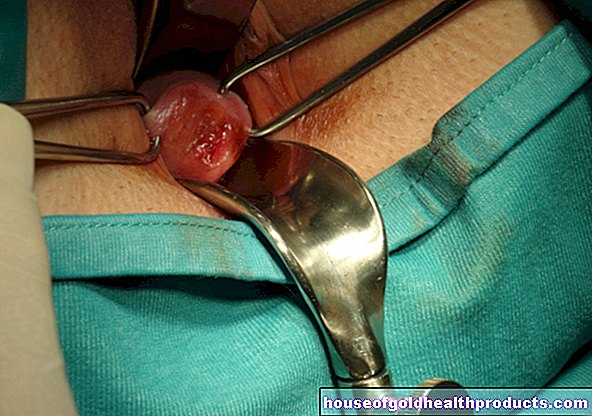
The doctor will take a closer look at any skin changes. If necessary, he also takes a tissue sample (biopsy) in order to examine it under the microscope. In sarcoid, the inflammation-related tissue nodules (granulomas) appear in the sample.
X-ray examination
Sarcoid almost always affects the lungs and lymph nodes in the lung area. This can be determined by an X-ray examination of the chest (chest X-ray): In Boeck's disease, an X-ray of the lungs shows, among other things, enlarged lymph nodes in the area of the main bronchi and large pulmonary vessels (biliary lymphadenopathy).
The doctor can also use the X-ray findings to determine the stage of the sarcoid. This stage affects the prognosis:
|
stage |
description |
|
Type 0 |
Signs of sarcoid outside the chest but no noticeable change in the lungs. |
|
Type I. |
Swelling of the lymph nodes on the pulmonary hili (biliary lymphadenopathy). The lung tissue itself shows no abnormalities. Spontaneous healing rate approx. 70 percent. |
|
Type II |
Swelling of the lymph nodes on the lung hili and lung involvement. Spontaneous healing rate approx. 50 percent. |
|
Type III |
No swelling of the lymph nodes on the lung hili, only lung involvement. Spontaneous healing rate approx. 20 percent. |
|
Type IV |
Lung fibrosis recognizable in the X-ray image (conversion of the inflamed lung tissue into scarred connective tissue). The lung function is irreversibly restricted as a result. Complete healing is no longer possible. |
Pulmonary function test
Sarcoid of the lungs can significantly reduce lung function. If lung tissue has hardened as a result of the disease (pulmonary fibrosis), it is less elastic when inhaled. This can be clearly determined with a lung function test.
Lungoscopy & biopsy
In a lung specimen (bronchoscopy), the doctor inserts a flexible, thin tube into the lungs. A small camera is attached to its tip. In this way, the doctor can examine the lung tissue directly.
Tiny instruments can also be inserted through the tube to take a sample of the lung tissue (biopsy). This is then examined in the laboratory for the typical granulomas.
Blood test
Blood tests are less used to diagnose sarcoid. However, different blood values help to assess the course of the disease. In sarcoid patients, for example, a certain enzyme is elevated in the blood, the so-called angiotensin converting enzyme (ACE). From the level of the measured value, the doctor can estimate how active the disease is. A high ACE value indicates high disease activity. When the sarcoid therapy works or the disease clears up on its own, the ACE in the blood drops.
In addition, inflammation parameters such as the erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) can be increased. This generally points to inflammatory reactions in the body - in sarcoid patients, therefore, to increased disease activity.
Further investigations
Since sarcoid can affect practically all organs of the body, further examinations are necessary depending on the symptoms. Some examples:
If the doctor suspects that the kidneys are involved, he will determine the kidney values in the blood. He can also examine the kidneys using ultrasound (sonography).
The heart function can be assessed with an electrocardiogram (EKG). The doctor can use the heart ultrasound (echocardiography) to check the size and function of the heart.
If neurosarcoidosis is suspected, the doctor can take a sample of the cerebrospinal fluid (CSF puncture) and have it analyzed in the laboratory.
If sarcoid (presumably) affects the eyes, an examination by an ophthalmologist may be necessary.
With a computed tomography (CT) the organs of the chest can be shown in much more detail than with an X-ray examination. This allows tissue changes to be assessed more precisely. Above all, however, the CT helps to rule out other diseases as the cause of the symptoms. These include, for example, lung cancer and tuberculosis.
Sarcoidosis: treatment
Sarcoid does not always have to be treated. It can heal spontaneously. This is especially true for acute sarcoid. Chronic sarcoid can also heal on its own. But that depends heavily on the stage of the disease. The higher the stage, the lower the self-healing rates.
In addition to the course, the severity of the symptoms also influences the decision: Treatment - yes or no? If the symptoms are not severe, it is often possible to wait and monitor the further course regularly. However, if there are serious symptoms, if lung function decreases and / or if critical organs such as the heart, kidneys or central nervous system are affected, the sarcoid should be treated. The condition can, for example, greatly increase the level of calcium in the blood. This so-called hypercalcemia can cause kidney stones and damage the kidneys. If the heart is affected, dangerous cardiac arrhythmias can occur.
How is sarcoid treated?
The treatment is based on the symptoms. If severe symptoms occur in acute sarcoid, so-called non-steroidal anti-inflammatory drugs (NSAIDs) are primarily used. These include, for example, acetylsalicylic acid and ibuprofen. They have an antipyretic, mild anti-inflammatory and analgesic effect. Cortisone ("glucocorticoids" such as prednisolone) can also be used for a short time in the event of severe complaints. It is very effective against inflammation.
For chronic sarcoidosis, cortisone is the treatment of choice. It is usually used over several months. Then the dose is slowly reduced again ("tapering off" the therapy).
Many patients fear the side effects of cortisone. The active ingredient can promote bone loss (osteoporosis), among other things. Side effects of this kind occur above all with prolonged and / or higher-dose use. The doctor will take this into account when planning therapy. For each sarcoid patient, he will choose a dosage and duration of therapy that is as low as possible, but at the same time has a sufficient effect. Patients should strictly follow these recommendations.
In severe cases of sarcoid, treatment with other drugs may be necessary. For example, some patients receive methotrexate or azathioprine. Both active ingredients are among the so-called immunosuppressants. They effectively suppress the immune system (in a different way than cortisone). This is how the inflammatory reaction comes to a standstill in the case of sarcoid.
Sometimes the doctor will also prescribe chloroquine. This active ingredient is usually used to prevent and treat malaria. It is suitable for sarcoid treatment because it can inhibit immune reactions, similar to immunosuppressants.
With type IV of chronic sarcoidosis (irreversible pulmonary fibrosis), further therapeutic measures may be necessary. Depending on the severity of the shortness of breath, the doctor may prescribe further medication (such as substances that expand the bronchi) or oxygen therapy. The lungs are rarely so badly damaged that they can no longer supply the body with sufficient oxygen. The only thing that can help those affected is a lung transplant.
Sarcoid: disease course and prognosis
The prognosis of sarcoid depends primarily on whether it is an acute or chronic form:
In most cases, the prognosis for acute sarcoid is good. In around 95 percent of patients, the disease heals spontaneously and without treatment within a few months.
Spontaneous healing is also possible with chronic sarcoid, but less often than with the acute form of the disease. The self-healing rates depend on the stage of the disease: they are best in the early stages. The more advanced Boeck's disease is, the worse the prognosis - even with therapy. About half of all patients with chronic sarcoid disease suffer permanent lung damage. However, they are often not very pronounced.
Overall, the following applies to acute and chronic sarcoidosis: In 20 to 30 percent of all patients, lung function remains permanently restricted. Around ten percent of patients even develop pulmonary fibrosis, which means that inflamed lung tissue turns into scarred connective tissue and thus loses its function.
About five percent of sarcoid patients die from complications such as sudden cardiac death or completely impaired lung function (terminal pulmonary fibrosis).
Additional information
Books:
- Live better despite sarcoid (Sigi Nesterenko, Rainer Bloch Verlag, 2010)
Guideline:
- Guideline "Sarcoid in Children and Adolescents" of the Society for Child and Adolescent Rheumatology and the German Society for Child and Adolescent Medicine
Self help:
- German Sarcoidosis Association non-profit: http://www.sarkoidose.de/
- Sarcoidosis Network e.V .: http://www.sarkoidose-netzwerk.de/