Fibromyalgia
and Christiane Fux, medical editor and Sabine Schrör, medical journalistClemens Gödel is a freelancer for the medical team.
More about the expertsChristiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane FuxSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.
Fibromyalgia is one of the pain syndromes. It is characterized by deep muscle pain in different parts of the body. In addition, there are exhaustion, concentration and sleep problems. The causes of fibromyalgia are not yet fully understood, but impaired pain processing is suspected. The treatment is complex and common painkillers are ineffective. Read everything you need to know about fibromyalgia syndrome here: symptoms, possible triggers and therapy.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M79
Brief overview
- What is fibromyalgia? A pain syndrome with no noticeable changes in muscles or joints.
- Symptoms: deep muscle pain, often exhaustion, sleep disorders, headaches, irritable bowel-like symptoms, depression, anxiety, etc.
- Causes: Trigger still largely unknown, possibly disturbed pain processing, genetic changes, altered nerve fibers, emotional trauma
- Diagnosis: based on the characteristic symptoms, the exclusion of other causes and pain questionnaires
- Treatment: planned individually; Components are e.g. movement therapy, heat therapy, psychotherapy, relaxation procedures, medication (antidepressants, anticonvulsants)
- Prognosis: Fibromyalgia cannot be cured, but it can be controlled with therapy. It leaves no permanent physical damage.
Fibromyalgia: Definition
Fibromyalgia is a pain syndrome. In addition to muscle pain, it brings with it other complaints such as tiredness, exhaustion and sleep disorders. In the case of a pronounced fibromyalgia attack, the performance of a person affected can be massively restricted. It is typical for this disease that the examination of the affected body parts (e.g. using MRI or ultrasound) does not reveal any organic causes for the symptoms.
Because of the diffuse chronic pain that can occur anywhere in the body, fibromyalgia is sometimes referred to as "generalized soft tissue rheumatism". It affects around two in 100 people in Germany. In 80 percent of the cases, these are middle-aged women.
Fibromyalgia: symptoms
The term "fibromyalgia" stands for fiber-muscle pain. That already describes the central symptom of fibromyalgia: deep muscle pain. These last longer than three months and are accompanied by other complaints, especially sleep disorders and exhaustion. Many of those affected also suffer from psychological symptoms such as depression or anxiety.
Due to the complex set of symptoms from various symptoms, doctors speak of fibromyalgia syndrome.
Main symptom is pain
The main symptom of fibromyalgia is chronic, diffuse pain. Those affected often describe it as deep muscle pain, which can be accompanied by stiffness, burning, knocking, numbness and tingling. In addition, joints or muscles sometimes feel swollen.
The pain occurs in several parts of the body. Typically, people with fibromyalgia report pain in the neck or middle back or lower back and at least one other location in both arms and legs.
Variable pain intensity: In fibromyalgia, pain stress and intensity are influenced by weather, temperature, time of day, stress and physical activity. In some patients, the pain is particularly intense in the morning and then gets better during the day.In general, warmth and moderate activity can usually improve symptoms of fibromyalgia.
Headaches & more: In addition to muscular pain, people with fibromyalgia often suffer from headaches or migraines. Irritable bowel symptoms with frequent abdominal pain, diarrhea or constipation are also common. Others suffer from pain similar to that of a urinary tract infection.
Pain in the face: A special variant of fibromyalgia manifests itself as what is known as the temporomandibular joint syndrome, in which the face and jaw hurt. Those affected can only move the latter to a limited extent, which causes them problems when chewing.
Fibromyalgia pain points: For a long time, painful pressure points (tender points, fibromyalgia pain points) on certain parts of the body were considered typical of fibromyalgia. If mechanical irritation resulted in pain at at least 11 of these 18 pressure points, the diagnosis "fibromyalgia" was considered confirmed. According to the current state of science, the tender points are no longer sufficient criteria for the diagnosis of fibromyalgia. Instead, a specific complex of symptoms must be present in order to be able to diagnose the disease.
Main symptoms of fatigue and insomnia
Fibromyalgia syndrome also includes fatigue and exhaustion in many cases. Often there are also sleep disorders - those affected are light sleepers and often wake up at night.
In addition, fibromyalgia patients are more likely to suffer from sleep apnea. Repeated short pauses in breathing occur during the night. As a result, sleep is not very restful and the risk of cardiovascular diseases increases.
Fatigue in fibromyalgia: The sleep disorders can lead to a chronic fatigue syndrome (chronic fatigue syndrome, CFS). Fatigue is the technical term for chronic fatigue. In fact, most fatigue sufferers meet the criteria for fibromyalgia. Conversely, the majority of fibromyalgia sufferers suffer from CFS.
Restless legs syndrome: A disease that also often occurs in fibromyalgia patients is the so-called restless legs syndrome. Those affected suffer from painful pulling or tingling in their legs when they are at rest. The only way to relieve symptoms is through exercise. This, too, can cause significant sleep disorders and subsequent fatigue. Patients with symptoms of fibromyalgia should therefore be examined to see whether they also have restless legs syndrome.
More fibromyalgia symptoms
Sometimes people with fibromyalgia also report symptoms of the eyes: swelling or fluid retention (edema) in the eye area is possible. In addition, fibromyalgia can cause visual disturbances such as flickering in front of the eyes.
It is not uncommon for the disease to be associated with emotional complaints. Nervousness, inner restlessness, depression and loss of drive are particularly common. Between 62 and 86 percent of patients even develop depression in the course of their lives. Anxiety disorders can also occur in connection with fibromyalgia.
Hypersensitivity is another common trait: People with fibromyalgia are often particularly sensitive to stimuli such as smells, noise, or light.
Further fibromyalgia symptoms occur as a result of the impaired body regulation. Such vegetative symptoms include increased tremor (tremor), excessive sweating (hyperhidrosis), reduced salivation and cold fingers.
Fibromyalgia Severity
How strong and varied the symptoms of fibromyalgia show varies greatly from patient to patient. Doctors divide the disease into different degrees of severity:
In addition to the pain in various parts of the body, those affected with milder forms have little or no other physical complaints and no emotional symptoms. They often experience longer symptom-free intervals and their quality of life is hardly affected.
In other cases, the chronic pain is accompanied by other physical and emotional symptoms of varying severity. The everyday life of those affected can be moderately to significantly impaired as a result.
Fibromyalgia: Therapy
Cure is not possible with fibromyalgia. With the right treatment, however, the symptoms of fibromyalgia can be controlled. However, there is no checklist of generally effective therapeutic measures. Rather, each patient receives an individually tailored treatment:
Appropriate therapeutic measures are selected by the doctor and patient together, tailored to the type and extent of the symptoms and the course of the fibromyalgia. Because it is crucial for the success of the therapy that the patient actively supports all measures.
Many fibromyalgia therapy measures are paid for by health insurance companies.
Exercise training
The focus of fibromyalgia treatment is usually to relieve muscle pain permanently. Move. Doctors recommend endurance training two to three times a week at low to medium intensity for patients. The aim is to stay in the so-called aerobic range when exercising, in which the body does not use more oxygen than it is currently taking in. A good starting point for this is if you still have enough air during exercise to be able to talk easily.
Sports suitable for endurance training in fibromyalgia include, for example:
- hike
- swim
- To go biking
- To dance
- Training on the ergometer
- Aqua jogging
- Walking
Such sports train cardiovascular fitness. In addition, targeted training of joint and muscle function as well as flexibility, strength and coordination is recommended for fibromyalgia, namely through:
- Water aerobics (two to three times a week)
- Dry gymnastics (two to three times a week)
- Functional training (twice a week)
Physical therapy
Heat treatment can improve the symptoms of fibromyalgia syndrome.
Cold, on the other hand, makes symptoms worse - at least in most cases. However, some patients report positive effects of whole-body cryotherapy. You spend a few minutes in a cold chamber with extremely low temperatures.
So-called balneotherapy with medicinal baths also has a soothing effect on many patients.
On the other hand, massages are expressly not recommended for fibromyalgia treatment.
psychotherapy
How severe pain is perceived depends on the inner attitude towards the complaints. As part of cognitive behavioral therapy, patients learn to reevaluate pain. He is then still there, but is no longer the focus of consciousness.
In addition, the therapist, in cooperation with the patient, reveals patterns of thought and perception that negatively influence the course of the disease. If they are broken, this can significantly change the perception of pain.
Relaxation procedure
Stress increases the discomfort of people with fibromyalgia. Therefore relaxation techniques are important elements of fibromyalgia therapy. This includes autogenic training and progressive muscle relaxation according to Jacobsen. Far Eastern relaxation techniques such as tai chi, qigong and yoga can also help.
Medical therapy
There are no drugs in Germany that are explicitly approved for the treatment of fibromyalgia. In the case of a severe course of the disease, the therapy can be supplemented by drugs that have been developed for other diseases: antidepressants and anticonvulsants.
Antidepressants
Many patients with fibromyalgia develop psychological comorbidities such as anxiety disorders or depression. In addition to cognitive behavioral therapy, antidepressants can then be prescribed. They influence the messenger metabolism in the brain and thus have a mood-enhancing, anxiety-relieving and - depending on the active ingredient - dampening (sedating) or activating.
Antidepressants can also reduce pain and fatigue and thus increase general well-being. This is why they are often prescribed to patients who do not have symptoms of depression.
Some antidepressants from the group of selective serotonin-norepinephrine reuptake inhibitors (SSNRIs) such as duloxetine or tricyclic antidepressants such as amitriptyline are recommended.
Antidepressants should only be used for a longer period if they are effective.
Anticonvulsants
Another important group of drugs for fibromyalgia therapy are the so-called anticonvulsants. They were developed to treat nerve pain and epilepsy, but can also be used as part of fibromyalgia therapy.
For example, some patients receive the anticonvulsant pregabalin, which also has an analgesic effect - it blocks certain messenger substances that are responsible for transmitting pain. This can especially help patients for whom severe pain is the main focus of the disease.
Mostly ineffective: painkillers
Although pain is the main symptom of fibromyalgia, most popular pain relievers are not recommended for fibromyalgia therapy - they have little or no effect.
Since fibromyalgia is not accompanied by inflammatory changes, anti-inflammatory pain relievers such as ibuprofen, acetylsalicylic acid or paracetamol also make no sense. Nor is the strong anti-inflammatory cortisone used.
Painkillers containing opioids are also unsuitable for fibromyalgia therapy. Most of them don't work. Tramadol is an exception. It is mainly prescribed to patients with pronounced symptoms of pain.
Alternative healing methods
In addition to conventional medical methods, some fibromyalgia patients use alternative healing methods. This includes methods of traditional Chinese medicine (TCM) such as acupuncture, but also osteopathy.
Other fibromyalgia patients rely on homeopathy. Different homeopathic remedies can be used depending on the nature of the symptoms. So should for example Rhus toxicodendron Reduce pain.
Fibromyalgia: Cannabis is not recommended
In principle, medical cannabis can help treat chronic pain under certain conditions. So far, however, there are no valid studies that prove its effectiveness in fibromyalgia pain. Therefore, cannabis is not recommended in current medical guidelines for the treatment of fibromyalgia.
Patient education
Training can be very helpful when starting fibromyalgia therapy. The patients learn more about their disease and the treatment. You will receive information and suggestions for self-management (physical activity, stress reduction, etc.) and can exchange ideas with other people affected. This can help each individual to cope better with the disease.
Rehab measures
Some patients suffer so much from symptoms such as pain, extreme exhaustion, depression or anxiety that they are often absent from work. In extreme cases, some people with fibromyalgia retire early.
Rehabilitation therapy in a clinic can make sense for such severe impairments and performance losses. A wide variety of treatment approaches are bundled as multimodal fibromyalgia therapy (e.g. patient training, physical measures, relaxation procedures, psychological or psychotherapeutic care).
Fibromyalgia: Diet
There is no particular diet that has been shown to help reduce symptoms of fibromyalgia. However, there is evidence that a diet with an emphasis on plant-based foods can have a positive effect on the course of the disease.
You can find more information on how to eat best with fibromyalgia in the article Fibromyalgia - Nutrition.
Fibromyalgia: causes and risk factors
The causes of fibromyalgia are still not fully understood. Usually there is no clear trigger for the pain disorder. What is certain is that it is not an inflammatory rheumatic disease of the muscles or joints, nor is it pain caused by wear and tear.
Disturbed pain processing
The most important hypothesis about the causes of fibromyalgia is currently that the central nervous pain perception of the patient is changed. The threshold of pain perception in fibromyalgia sufferers is lower than usual, so that the brain perceives even light stimuli as pain and attaches greater importance to it. One possible explanation for this is low levels of serotonin, which has been shown in some studies in fibromyalgia patients.
Genetic predisposition
Fibromyalgia often occurs in families. This suggests a genetic component - certain genetic changes could result in increased pain sensitivity, but have not yet been identified.
Altered nerve fibers
Studies by the University of Würzburg have produced organic findings in fibromyalgia, i.e. initial evidence of physical changes in those affected: The researchers found that the small nerve fibers in the muscle tissue of patients with fibromyalgia were changed. Further study results from the university also suggest that the severity of fibromyalgia symptoms depends on how severely the skin nerves are damaged. However, the researchers' findings have not yet had any impact on the diagnosis and treatment of fibromyalgia.
Psyche, stress and trauma
Since there is usually no organic explanation for the pain, those affected have long been considered imaginary patients. Or it has been wrongly assumed that the symptoms of fibromyalgia are the purely psychosomatic expression of depression.
This hypothesis has now been refuted, even if the psyche can play a central role in the development of the disease. Stress and physical or emotional injuries (trauma) can promote fibromyalgia. The disease often appears in phases of great stress. In addition, people who were ill-treated or sexually abused in childhood or as adults are more likely to develop fibromyalgia.
Last but not least, the high level of stress associated with a severe course of the disease can promote anxiety and depression.
Unhealthy lifestyle
An unfavorable lifestyle can also promote your fibromyalgia. These include smoking, obesity and little physical activity.
Middle age, female gender
Fibromyalgia can occur at any age. Most often, however, it develops between the ages of 40 and 60. Gender also plays a role: 80 percent of those affected are female.
Secondary fibromyalgia
In some cases, fibromyalgia appears to develop in conjunction with another condition. Then one speaks of secondary fibromyalgia - in contrast to primary fibromyalgia, in which no other diseases are possible causes.
The diseases that can favor fibromyalgia include:
- other rheumatic diseases
- Infectious diseases, mostly viral infections with Epstein-Barr viruses (causative agent of Pfeiffer's glandular fever), hepatitis viruses and HI viruses
- certain tumor diseases
- Disorders of the hormonal balance
Fibromyalgia: diagnosis
If a fibromyalgia syndrome is suspected, the family doctor is the first point of contact. If necessary, he treats the disease in cooperation with specialist colleagues such as specialized pain therapists, neurologists, psychotherapists and physiotherapists.
It often takes a long time before the diagnosis of fibromyalgia is made because the clinical picture is very diverse and difficult to grasp. It is not uncommon for those affected to wander from doctor to doctor for years and suffer from the fact that their symptoms cannot be assigned to a diagnosis. This unsettles those affected, delays treatment and thus worsens the prognosis.
Anamnesis interview
The first step in clarifying a possible fibromyalgia is the conversation between doctor and patient to collect the medical history (anamnesis). Typical questions the doctor may ask are, for example:
- Where exactly are you in pain?
- How does your pain feel?
- Do you have any known rheumatic diseases?
- Is your everyday life impaired by the symptoms?
- Do you suffer from insomnia?
- Do you have gastrointestinal complaints?
- Is your mood impaired?
Cornerstone of diagnosis
For a long time, the so-called tender points or fibromyalgia trigger points played a central role in diagnosis. These are certain points on the body that can be painful when put under pressure. If at least 11 of a total of 18 tender points react to pressure with pain in a patient, this was considered an indication of fibromyalgia syndrome.
However, the exclusive diagnosis based on the tender points is now considered obsolete. Instead, experts advise making the diagnosis on the basis of the following symptoms:
- chronic pain in several parts of the body for at least three months
- physical and / or physical exhaustion / tiredness
- not restful sleep
- Stiffness of the hands and feet
- reduced physical and / or mental performance
Further notes provide information from the anamnesis:
- similar chronic pain in multiple parts of the body in family members
- Pain in the musculoskeletal system, head, or abdomen in childhood or adolescence
- high level of suffering
- increasing pain during massage
- unsuccessful orthopedic treatment
Pain diary as a diagnostic aid
The doctor will ask the patient to keep a pain diary in which, in addition to the type, duration and location of the pain, he also precisely records accompanying abnormalities. These include gastrointestinal complaints or problems urinating, for example.
Psychological stress such as concentration or sleep disorders as well as lack of drive should also be noted and discussed with the doctor. Such accompanying symptoms are typical of fibromyalgia syndrome.
Exclusion of other diseases
The symptoms that fibromyalgia patients suffer from also occur with other diseases. This includes:
- Rheumatoid Arthritis (RA)
- Systemic lupus erythematosus (SLE)
- Bechterew's disease (ankylosing spondylitis, AS)
- Polymyalgia rheumatica (PMR)
- Hyperthyroidism and other hormonal disorders
- Inflammation of the muscles
- Diseases of the central or peripheral nervous system
With the help of various examinations, the doctor can exclude or uncover such diseases as the cause of the symptoms, for example by means of:
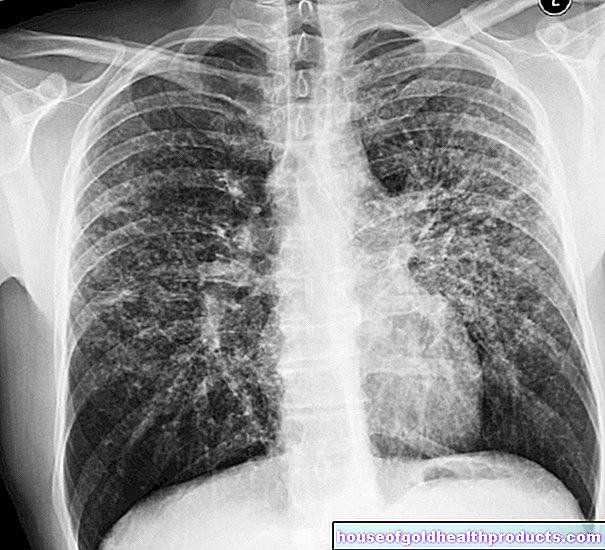
- roentgen
- Computed tomography (CT)
- Magnetic resonance imaging (magnetic resonance imaging, MRI)
- Blood test, including for the so-called rheumatoid factors
If no pathological changes are found during these examinations, this speaks for fibromyalgia.
Imaging (e.g. X-ray, CT) does not show any pathological changes in the painful areas of the body in fibromyalgia even after several years of illness. Common laboratory tests (e.g. for rheumatoid factors) also remain inconclusive.
Mentally conditioned pain disorders
There is also a risk of confusion with fibromyalgia symptoms with “persistent somatoform pain disorder” and “chronic pain disorder with psychological and somatic factors”. In these clinical pictures the pain is caused by strong psychological stress - which does not mean that it is mere imagination! In fibromyalgia, on the other hand, strong psychological stress is not the cause, even if this can worsen the symptoms.
Fibromyalgia Tests For Self Diagnosis?
Various online questionnaires for the fibromyalgia self-test can be found on the Internet. However, they are not very meaningful, for example they often only contain individual symptom areas such as pain. Diagnosing the complex clinical picture of fibromyalgia belongs in the hands of experienced doctors!
Fibromyalgia: course and prognosis
Fibromyalgia is currently not curable. However, it does not cause permanent damage to muscles and joints, so that fibromyalgia patients are not threatened with severe disability. The life expectancy of those affected is not reduced either.
The chronic pain and other fibromyalgia symptoms can, however, have a significant impact on the quality of life of those affected. Treatment therefore aims to reduce the symptoms as much as possible. In order for this to be successful, close cooperation between doctor and patient is necessary - fibromyalgia treatment is usually complex and difficult.
An early start can increase the chances of success: if treatment is initiated within two years of the onset of symptoms, it can largely relieve up to 50 percent of those affected from their pain. After the age of 60, the symptoms of fibromyalgia often improve on their own.
Early retirement?
If the symptoms of fibromyalgia cannot be relieved sufficiently, the suffering is high for those affected. Those who work often have to take sick leave due to illness. In their distress, some patients consider applying for a severe disability or even retiring early.
Getting a pension actually approved is difficult, however, as the symptoms of fibromyalgia have so far hardly been proven by hard findings (such as x-rays or laboratory values). Sufferers should turn to support groups and fibromyalgia organizations on this matter.
Tags: smoking sleep toadstool poison plants







.jpg)