Diabetic foot
and Martina Feichter, medical editor and biologistDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
A diabetic foot is a common complication of diabetes (diabetes mellitus). Due to the high blood sugar, blood vessels and nerve tracts are damaged. This makes it easier for wounds to develop on the foot, which can become infected. With the right care measures and good blood sugar regulation, serious complications can usually be avoided. Read everything you need to know about the diabetic foot here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E11E10E13O24H36E12E14
Diabetic foot: description
The term "diabetic foot" or "diabetic foot syndrome" (DFS) describes various clinical pictures, the common cause of which is the increased blood sugar level in diabetes mellitus:
- In around 30 to 40 percent of those affected, the diabetic foot is caused by diabetic nerve damage (diabetic polyneuropathy). This variant is also called a neuropathic diabetic foot.
- In around 20 percent of those affected, vascular damage and the resulting circulatory disorders are the trigger for the diabetic foot. Then there is a poorly perfused (ischemic) diabetic foot.
- In around 40 percent of patients with a diabetic foot, both nerve damage and circulatory disorders are responsible.
A diabetic foot is a serious complication of diabetes mellitus. The longer you have diabetes and the worse your blood sugar levels are, the more likely it is to occur. Overall, diabetics have a 25 percent risk of developing a diabetic foot in their lifetime. Treatment can be lengthy. In the worst case, there is a risk of a complete amputation of the toe, foot or the entire leg.
Diabetic foot: symptoms
A diabetic foot manifests itself differently in the person affected. Symptoms depend on the underlying cause and the stage of the disease. A neuropathic diabetic foot has different symptoms than an ischemic (low blood supply) diabetic foot.
Ischemic Diabetic Foot Symptoms
The reduced blood flow (reduced perfusion) usually discolors the skin pale or bluish. In addition, the skin often feels cool and the pulse of the arteries in the foot can no longer be felt.
The lack of blood circulation (ischemia) means that the muscles are no longer adequately supplied with blood. Many sufferers therefore complain of cramp-like pain (intermittent claudication) even after walking short distances. If there is a pronounced circulatory disorder, this pain can exist even at rest.
The toes and heels tend to have the poorest blood supply, which is why injuries are particularly difficult to heal here. A banal injury here easily leads to an open ulcer (ulcer). The surrounding tissue becomes inflamed or even dies (necrosis). Typically, necrotic tissue turns pitch black and looks charred.
Neuropathic Diabetic Foot Symptoms
The sensitivity of the cutaneous nerves is impaired here. For this reason, the patients only notice pressure points and pain less or no longer at all: Since those affected do not notice injuries to the foot, for example, they do not take sufficient care of the injured area. As a result, the wound cannot heal, it actually increases in size over time.
In addition, misalignments of the foot can result with muscle wasting. If the feet are not put under stress, more calluses often form on pressure points. However, these corneal structures promote pressure and shear forces under the skin, which can result in deep bruises. These often break open later - an open diabetic foot ulcer (malum perforans) develops.
The open ulcer can become infected with bacteria very easily. As a result, these often also affect the surrounding, healthy tissue. Since a diabetic foot still has sufficient blood supply due to a polyneuropathy, the skin of the feet is dry (due to insufficient nerve supply to the sweat glands), but still warm and pink (because there is still sufficient blood supply).
Symptoms when both clinical pictures are combined
Patients in whom the diabetic foot can be traced back to a circulatory disorder and damage to the nerve tracts show the signs of ischemic diabetic foot, but do not experience any pain.
Severity classification of foot lesions
The diabetic foot syndrome describes the above-mentioned clinical pictures (polyneuropathy, PAD), which in diabetics can lead from an injury to the foot to an infected ulcer. The foot lesions are divided into different stages (according to Wagner) depending on their severity:
|
Grade 0 |
Risk foot: No injuries, but possibly deformed feet |
|
Grade I. |
Superficial wound |
|
Grade II
|
Deep wound that reaches the tendon or capsule |
|
Grade III |
Deep wound that goes down to the bone or joint |
|
Grade IV |
Dead tissue (necrosis) on the heel or toe |
|
Grade V |
Dead tissue (necrosis) all over the foot |
Diabetic foot: causes and risk factors
A diabetic foot is the result of years of elevated blood sugar levels. This damages both the blood vessels (diabetic angiopathy) and the nerve tracts (diabetic neuropathy) in the foot and in the rest of the body.
Ischemic diabetic foot - causes
The main damage in an ischemic diabetic foot is the blood vessels, which affects the blood circulation in the foot. A circulatory disorder caused by narrowing of the arterial blood vessels is also generally referred to as peripheral arterial occlusive disease (PAD). It can result from diabetes, but also from other diseases.
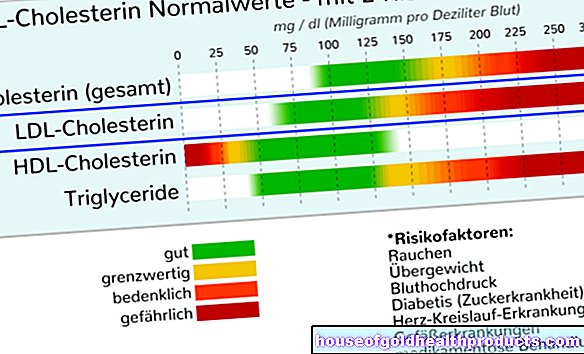
The high amount of sugar in the blood of diabetic patients causes damage to the inner walls of the blood vessels in particular. Usually the vessels of the feet and lower legs are affected first. In addition to high blood sugar, there are often other vascular damaging factors. These include smoking, high blood pressure and high cholesterol.
Due to the continuous damage to the inner layer of the vessels, the diameter of the vessel becomes smaller and smaller. This means that less and less blood can flow through the vessels - the tissue is insufficiently supplied with blood. This results in a lack of oxygen in the tissue, which affects all metabolic processes in the cells. For example, wound healing is disturbed so that injuries in a diabetic foot heal much more poorly. If the lack of oxygen is very pronounced, the cells in the tissue section in question die even without a causal injury (necrosis).
The lack of blood circulation also affects the body's defense function. Pathogens such as bacteria or fungi have an easy job: Even the smallest wounds can be enough for germs to get into the body and cause an infection.
Neuropathic Diabetic Foot - Causes
If the nerve tracts in a diabetic foot are mainly damaged by the increased blood sugar, this is a neuropathic diabetic foot. Due to the nerve damage, many patients do not notice injuries and wounds on the foot. Without treatment, however, these can easily become infected. Pain caused by too tight or incorrect footwear often goes unnoticed.
The nerve damage can also cause deformations of the foot and the skeleton of the foot. Doctors then speak of the Charcot foot. Due to the reduced feeling of pain, small fractures, for example in the area of the tarsal bones, often go unnoticed for a long time. They can lead to acute and chronic changes in the ankles by breaking down and remodeling bones and stiffening joints.
Diabetic foot: examinations and diagnosis
The right person to contact if you suspect a diabetic foot is a specialist in internal medicine and diabetology or a specialist in foot surgery.
The doctor first conducts a detailed discussion with the patient in order to collect their medical history (anamnesis). The patient should describe all current complaints and any previous illnesses in detail. The doctor will also ask questions such as:
- How long has diabetes mellitus existed?
- Do you feel tingling or numbness in your feet?
- Do you notice pain, pressure or temperature changes in your feet?
- Do you suffer from high blood pressure?
- Do you smoke? If so, how much and for how long?
- Which shoes do you wear?
- Do you perform regular foot care?
- Do you suffer from nail fungus?
Physical examination
The doctor will then examine you physically, especially looking at your feet. For example, the doctor feels the skin temperature and the foot pulses to get clues about a possible circulatory disorder.
Further investigations
As a rule, further examinations are necessary in order to precisely determine the extent of a circulatory disorder or nerve damage.
|
investigation |
Significance of the examination method |
|
Ultrasound (duplex) |
The duplex ultrasound provides information on possible circulatory disorders. |
|
Ankle-arm index |
The ankle-arm index is the ratio of systolic blood pressure values in the lower leg and in the upper arm. If it is less than 0.9, it indicates arterial occlusive disease. |
|
Angiography (DSA) |
This X-ray examination with contrast agent can show the vessels. Constrictions or closures can be recognized in this way. |
|
Reflex tests |
In the case of a neuropathic diabetic foot, the reflexes of the lower leg / foot may be weaker or no longer triggerable at all. |
|
Tuning fork test |
With the help of a tuning fork struck by the doctor, the vibration sensation is tested by sustained vibrations of the fork. In a neuropathic diabetic foot, it is reduced. |
|
Monofilament test |
The sensitivity of the skin to touch is checked by placing a 0.1 mm wide thread on the sole of the foot. |
|
Smear the wound |
A swab should be taken from wounds on the feet to determine the exact bacterial pathogen. Then the right therapy can be initiated. |
|
Pedography (pressure measurement of the foot) |
The patient stands and walks on a plate equipped with sensors. This can indicate a changed pressure load on the foot due to misalignments. |
Diabetic foot: treatment
A diabetic foot can only be treated successfully if the causes are corrected. The blood sugar values must therefore be adjusted as well as possible so that the vascular or nerve damage does not progress any further. Existing nerve damage cannot be healed, but circulatory disorders can be improved with various measures.
Various professional groups are involved in the treatment of a diabetic foot: In addition to doctors (diabetologists, foot surgeons), specialized wound therapists, podiatrists and orthopedic technicians are also indispensable.
Blood sugar control
The most important measure to prevent the disease from progressing is to control your blood sugar levels as precisely as possible. The "long-term blood sugar value" HbA1c shows whether the blood sugar is well adjusted. Patients diagnosed with diabetic foot should aim for an HbA1c of less than 6.8 percent.
Eliminating risk factors
Eliminating risk factors for peripheral arterial occlusive disease (PAD) is also very important: those affected should never smoke, as this will severely damage the blood vessels. In addition, existing high blood pressure and high cholesterol levels should be reduced with suitable therapy.
Training and regular check-ups by the doctor
Various training courses are offered for diabetics. There, patients learn everything they need to know about diabetes. This also includes information on how a diabetic foot can be prevented with the right foot care and suitable footwear. In addition, the patients are trained to recognize changes such as skin tears, pressure points or nail changes at an early stage.
In addition, diabetics should go to the family doctor regularly to examine their feet and lower legs and have their blood sugar levels checked.
Daily inspection and care of the feet
As a patient, you should also inspect your feet every day, especially if you already have vascular and nerve damage. In this way you can recognize any changes and small injuries at an early stage. In places that are difficult to see, you can use a mirror to discover possible thickening of the cornea, pressure points or corns (clavus).
You should wash the spaces between your toes and the soles of your feet every day. Use mild, neutral and moisturizing soaps for this. Make sure the water temperature is 37 to 38 degrees Celsius and soak your feet in it for three to five minutes. Afterwards you should dry your feet carefully.
Avoid such foot baths in the event of skin injuries. Instead, you should treat the wound with a skin disinfectant, cover it with a sterile gauze bandage, and see a doctor.
It is also advisable to put cream on your feet every day (avoiding the spaces between the toes). This prevents the skin from drying out and tearing. Use an ointment or cream that is high in fat but low in water. In addition, no emulsifiers, perfumed additives and preservatives should be on the list of ingredients.
Also pay attention to proper nail care: you should file (not cut off) the nails and use them to round off the corners. Pointed nail scissors pose a risk of injury.
Some patients cannot perform regular foot care on their own, for example because they have trouble stooping. Then you should definitely seek professional medical foot care.
Podiatry therapy as a remedy
Patients with diabetic foot syndrome can have podiatry therapy prescribed for the care of their feet as part of the medication prescription - either for one or both feet.
When is podiatry therapy an option?
Such a therapy is an option if there is a threat of consequential damage to the feet such as inflammation and wound healing disorders. If inflammation and ulcers have already formed, the treatment must be carried out by a doctor. The podiatrist can then continue to treat those areas of the foot that have not yet been damaged.
What do you do as part of podiatry therapy?
Podiatry foot care begins with a foot bath, a detailed anamnesis, and an inspection of the feet. This is followed by the actual medical foot care for diabetics. This includes:
- Corneal ablation: By ablating the thickened cornea, skin damage such as cracks, ulcers and inflammation can be prevented. To do this, the cornea is carefully peeled off and ground down.
- Nail processing: With the help of nail processing, damage to the nail bed and nail wall can be prevented, for example also ingrown nails. For this purpose, thickened and deformed nails are cut, sanded and milled off.
Note: The combination of corneal removal and nail processing is called a podiatry complex treatment.
In addition, the podiatrist treats foot problems such as ingrown nails or fungal infections during a session.
What are the risks of podiatry therapy?
When working on the nails, the podiatrist can slip and injure the toe or foot. This wound - especially in diabetics - can easily become infected and heal poorly. In addition, if too much cornea is removed, it can really stimulate new formation. Performed by experienced staff, podiatry therapy is very safe.
What do I have to consider during podiatry therapy?
The most important thing about podiatry treatment is that you put yourself in the hands of a trained specialist.
Medication
For circulatory disorders, the doctor can prescribe the daily intake of acetylsalicylic acid (ASA). The active ingredient has a "blood-thinning" effect.
If a diabetic foot has already become infected, the responsible pathogens must be identified by a smear and treated with a suitable antibiotic. Different germs are often found in the wound. Then the doctor can either prescribe different antibiotics or a broad spectrum antibiotic that helps against several germs. It may be necessary to rest in bed for some time so that the open areas of skin can heal in peace.
Wound cleansing
Wounds on the feet and lower legs should not only be treated with medication, but should also be cleaned daily by trained professionals. If necessary, dead tissue must be removed (debridement). The wound must also be softly positioned so that there are no further pressure points and the wound can heal better. Many foot surgery departments in hospitals offer consultation hours for the treatment of diabetic foot.
Appropriate footwear and diabetic socks
Correctly fitting footwear is very important so that wounds on diabetic feet heal and do not enlarge or recur. There must be enough space for your feet in the shoes and there must be no pressure anywhere. The footbed can be adjusted with insoles if necessary.
Orthopedic advice can be very helpful in choosing the right shoes. The patient may also need specially made diabetic shoes.
There are also special socks for diabetics that allow better ventilation of the feet. The diabetic socks have a high percentage of cotton and have no seams that could cause pressure points. You can get diabetic stockings in special medical footwear stores.
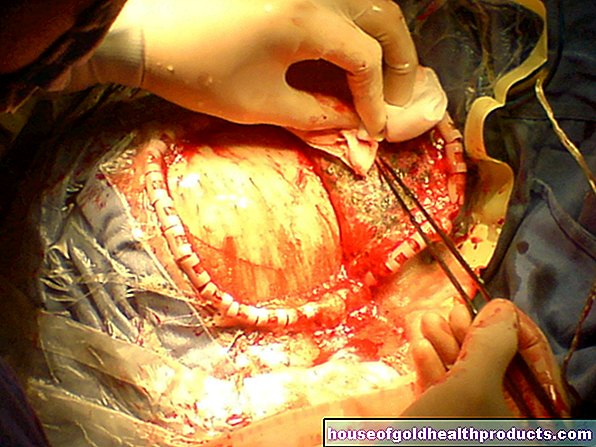
Balloon dilation, stent placement, bypass surgery
If an ischemic diabetic foot is accompanied by a narrowing of the vessels, this can be expanded with the help of a so-called catheter (angioplasty). In principle, several methods are available for this. Balloon dilatation is very often performed. A tube is pushed through the leg artery (arteria femoralis) from the groin to the narrowed point. At its tip there is a small expandable balloon. At the destination (bottleneck) the balloon is filled with air or liquid via the tube. So he can expand the bottleneck.
This procedure alone does not always bring the desired success: Many patients soon find another narrowing in the same place. Therefore, after the vessel has been expanded, a small metal tube (stent) is often inserted to keep the vessel open.
If the narrowing affects a longer section of the vessel, bypass surgery can be useful. The constriction is bypassed with a surgically inserted, different blood vessel.
amputation
In very severe cases of diabetic foot it may be necessary to amputate toes, feet or even the leg. Before that, however, all other therapy options should be exhausted and the condition of the affected limb should be assessed by a second doctor (second opinion).
Diabetic foot: disease course and prognosis
Diabetic foot is a serious and common complication of diabetes mellitus. Diabetes patients have a 25 percent risk of developing a diabetic foot in their lifetime. Every year around 40,000 foot amputations are performed in Germany due to a diabetic foot. This makes it clear that the disease is a very serious complication of diabetes. Those affected have a very large influence on the course of the disease. A diabetic foot can often be avoided if it is possible to control blood sugar in the best possible way, to eliminate risk factors and to observe thorough daily foot hygiene.
Tags: drugs elderly care skin