radiotherapy
and Martina Feichter, medical editor and biologistDr. med. Philipp Nicol is a freelance writer for the medical editorial team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Radiation therapy is the medical application of ionizing, cell-destroying radiation. Doctors also speak of radiation, radiotherapy or radiation. Cancer is a common reason for radiation therapy. But it is also used for other diseases. Here you can read everything about the course of radiation therapy, possible side effects and what you need to be aware of afterwards.
What is radiation therapy?
Medical radiation therapy is based on what is known as ionizing radiation from particles and their harmful effects on living cells. The high-dose radiation damages the genetic material of the cells exposed to it - both healthy and cancer cells. In contrast to healthy cells, cancer cells can hardly repair such damage: they die.
Radiation therapy is divided into soft radiation (up to 100 kV), hard radiation (over 100 kV) and megavolt therapy (over 1000 kV) based on the energy it contains. Soft and hard radiation is mainly used for superficial tumors, whereas megavolt therapy is used for deep-seated tumors.
When is radiation therapy performed?
The best known is radiation for cancer. Sometimes, however, the treatment is also carried out for other diseases.
cancer
The areas of radiation therapy and oncology (study of tumor diseases) are closely linked: Cancer patients very often receive radiation - in addition to other therapies. The goal can be:
- to cure the cancer patient as much as possible (curative radiation) or
- at least the symptoms Uz.B. Pain) if the tumor disease is already too far advanced to cure (palliative radiation)
Cancer radiation can be carried out either alone or in combination with chemotherapy (as radio chemotherapy). Sometimes radiation therapy is also started before a tumor operation (neoadjuvant radiation therapy), for example to reduce the size of the tumor before the operation. Irradiation can also be useful after the surgical removal of the tumor in order to eliminate any remaining cancer cells (adjuvant radiation therapy).
How a tumor is treated in each individual case depends on several factors such as the type and extent of the cancer as well as the age and general condition of the patient. The treatment of a cancer patient is usually planned individually by an interdisciplinary team, the so-called tumor board. Below you will find examples of the most important information on three of the most common tumor diseases and their treatment with radiation, among others (breast cancer, lung cancer and prostate cancer).
Radiation for breast cancer
Breast cancer is the most common cancer in women. In Germany there were almost 69,000 new cases in 2016.
In addition to surgery and drug therapy (chemotherapy, anti-hormone therapy, antibody therapy), radiation therapy for breast cancer is an important treatment option.Usually the tumor is removed surgically. Sometimes the whole breast has to be removed for this (mastectomy). If possible, however, surgery is performed to conserve the breast.
After the operation, patients usually receive radiation to destroy any cancer cells that are still present (adjuvant radiation therapy). Breast cancer tumors that are so large that a mastectomy would actually be necessary can also be irradiated beforehand in order to shrink them (neoadjuvant radiation therapy). In the best case, breast-conserving surgery can then be performed.
However, drugs can also shrink the tumor. Therefore, neoadjuvant breast cancer radiation is now rare.
In a few patients, radiation therapy is carried out without surgery. This can be the case, for example, if the cancer has spread so far that it can no longer be surgically removed. Radiation therapy alone is an option even if the woman is not allowed to have an operation due to comorbidities or if she does not want an operation.
Radiation for lung cancer
Lung cancer is the second most common cancer in men and the third most common in women. In Germany, around 36,000 men and around 21,500 women were newly diagnosed with a malignant lung tumor in 2016.
Lung cancer therapy depends primarily on which type of cancer is present (non-small-cell or small-cell lung cancer) and how far the tumor has spread.
There are basically three treatment methods to choose from for the treatment of lung cancer: surgery, radiation therapy and chemotherapy. They can be used individually or in different combinations. Very often radiation and chemotherapy are combined with each other in lung cancer (chemoradiotherapy).
In order to minimize the risk of daughter tumors (metastases) in the brain, many patients also receive prophylactic skull radiation.
With brain metastases, but also with lung tumors themselves, stereotactic radiotherapy (SRT) can also be useful in some cases. The cancer tumor is irradiated very precisely and with high intensity from different angles. Read more about this below.
Radiation for prostate cancer
Prostate cancer is the most common tumor disease in men. In 2016, almost 58,800 men were newly diagnosed with it in Germany.
Surgical tumor removal is the gold standard in prostate cancer therapy. Alternatively, radiation therapy can be carried out if an operation is not possible (poor general condition) or is refused by the person concerned.
A combination of prostate cancer radiation and surgery is also possible: if the tumor has spread beyond the prostate capsule, the cancer cells that were not surgically removed can be destroyed with the ionizing radiation. Cancer radiation is usually carried out on an outpatient basis by a radio-oncologist or radiation therapist in several sessions over a period of a few weeks.
Other diseases
Sometimes patients are also treated with radiation therapy for a non-cancer-related, "benign" disease - most often for painful joint wear and tear (osteoarthritis). Other areas of application for radiation therapy include:
- Dupuytren's disease (hardening and shrinking of tendon structures in the palm of the hand)
- Ledderhose's disease (like Dupytren's disease, but on the sole of the foot)
- Vertebral hemangioma ("blood sponges" in a vertebral body)
Irradiation for such diseases is similar to that for malignant tumors.
Emergency radiation
So-called emergency radiation or oncological emergency therapy is carried out when a cancer patient's condition deteriorates acutely - for example, when a tumor squeezes the superior vena cava and thus hinders the return of blood to the heart (upper congestion). Tumor bleeding is also an oncological emergency that must be treated as quickly as possible. In addition to other treatment options (such as medication or surgery), radiation therapy can then also be considered as an emergency treatment.
What do you do with radiation therapy?
Radiation therapy is usually carried out in several sessions and carefully planned for this. To do this, the doctor uses imaging (computed tomography, magnetic resonance imaging) to determine the radiation field.
It is also very important to determine the correct radiation dose and duration. In the case of cancer patients, the type of tumor is included in the planning. There are radiation-sensitive tumors (e.g. seminoma, lymphoma), which can be treated well with a low dose, and radiation-resistant tumors (e.g. malignant melanoma, sarcomas), which can be treated with a high radiation dose. In addition, the dose is chosen so that it effectively destroys the tumor tissue, but puts as little stress on the surrounding tissue as possible.
In this context one speaks of the “fractionation” of the radiation, ie the distribution of the radiation dose over a longer period of time (usually several weeks). This allows the healthy tissue to recover and regenerate between treatments.
There are different forms of radiation therapy. A basic distinction is made between irradiation from the outside (teletherapy) and irradiation from within (brachytherapy). Stereotactic radiotherapy is a special form.
Teletherapy
This radiation therapy from the outside through the skin (percutaneous) is also called percutaneous radiation therapy. The patient usually lies on a treatment table in a bright room. The radiation source is placed approximately at arm's length where it should work. So that the irradiation field cannot accidentally "slip", the patient is fixed in a suitable position for the irradiation. Special, individually adapted storage systems may be necessary for this. In some cases, marking points (e.g. with henna) are attached or tattooed in order to find the exact points for each therapy session.
In some cases, total body irradiation (TBI) is indicated, for example to treat blood cancer (leukemia). On the one hand, this can destroy tumor cells throughout the body and, on the other hand, suppress the immune system (in preparation for a bone marrow transplant).
The actual irradiation generally only takes a few minutes or even seconds. It is completely painless. The rays are also not visible and cannot be heard or smelled. The doctor and technical assistants leave the room for the irradiation, but remain in visual contact with the patient via a pane of glass and communicate with him via microphones.
In addition to conventionally performed percutaneous radiation therapy, there are also some special variants. One of them is stereotactic radiation therapy:
Stereotactic Radiotherapy (SRT)
In the stereotactic radiotherapy (stereosurgery) several, non-parallel beam paths are used. These meet at one point (the tumor tissue) and bundle there to form a stronger, therapeutic total dose. The surrounding, healthy tissue is only hit by the individual, energetically weaker rays and is thus spared. This reduces the risk of side effects from radiation therapy.
Stereotactic radiotherapy is mainly used for tumors or vascular malformations in the brain. Whether stereotactic radiation can be considered instead of conventional radiation therapy in individual cases depends on various factors:
- Tumor size: Tumors over four centimeters in diameter should not be stereotactically irradiated, as the risk of radiation therapy side effects in healthy neighboring tissue increases with the size of the tumor.
- Tumor location: Radiation-related side effects depend on the location of the tumor in the brain. The risk is lower for a location in the area of the temple or forehead (temporal or frontal lobe) and higher for tumors of the brain stem, among other things.
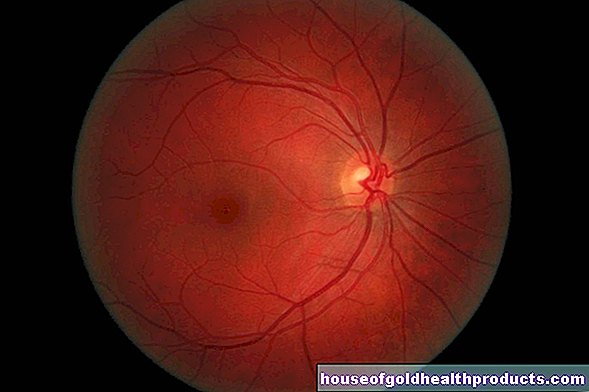
- Nerve proximity: If important cranial nerves such as the optic nerve (nervus opticus) are in the immediate vicinity of the tumor, stereotactic radiation should also not be carried out. The risk of nerve damage from radiation therapy is too great.
There are various systems that are used today for stereotactic radiation such as the gamma knife, the Cyberknife or the ExacTrac Robotic System. What all systems have in common is that you have to fix the patient's head very precisely for the operation in order to hit the tumor that was previously shown with the imaging as precisely as possible. Apart from different types of this fixation, the systems differ from one another mainly in technical details. In contrast to conventional radiation therapy, with the Gamma-knife / Cyberknife etc. there is no division of the total radiation dose over a longer period of time - the dose is only administered once during the operation.
Brachytherapy
The irradiation from the inside takes place by means of radiating substances that are introduced into a body opening or cavity or - in the case of skin cancer, for example - are placed directly on the tumor. Because the radiation they emit only has a range of a few millimeters to centimeters, the radiation source must be brought as close as possible to the site of action (e.g. cancerous tumor).
There are different forms of brachytherapy:
Intracavitary (intraluminal) Brachty therapy
A radiating substance (radionuclide) is introduced into a natural body cavity - for example into the windpipe (for lung cancer) or the vagina or uterus (for uterine cancer):
Usually, a sleeve (called an applicator) is placed in the body cavity first, under local or general anesthesia. Then the doctor - usually computer-controlled - inserts the radionuclide into the sleeve through a tube. It is usually removed after a few minutes - the actual irradiation usually does not take any longer.
Interstitial Brachty Therapy
Catheters, i.e. small hollow needles or tubes, are used as applicators for the radionuclide. They are inserted directly into the tumor tissue by the doctor. Depending on the type of tumor and the radionuclide used, these implants remain in the body permanently or only temporarily.
Permanent "seed" implantation
This form of internal radiation therapy is mainly used for prostate cancer. The tumor is peppered with radiating "seeds" - a radiation source in the form of small capsules or radioactive metal particles. The "seeds" remain permanently in the body. This allows longer-term irradiation so that the patient does not have to go to the hospital for a radiotherapy appointment again. The radiation dose decreases significantly in the first few days after implantation because the radionuclides used disintegrate quickly.
Surface contact therapy
In the case of a superficial tumor (e.g. black skin cancer), a coated radiation source can be placed directly on the affected area. As soon as the cancer tissue has absorbed the necessary radiation dose (usually after a few minutes), the source is removed again.
What are the risks of radiation therapy?
Radiation therapy can - depending on the radiation dose and duration - trigger a large number of severe side effects. A distinction is made between acute radiation therapy side effects and chronic side effects of radiation therapy.
Acute radiation therapy side effects
The acute side effects are the result of tissue swelling (edema) triggered by the radiation, which mainly develops in the irradiated area. They depend on the irradiated area. Here is a selection of the possible side effects:
- Radiation therapy of the abdomen: feeling weak, nausea and vomiting
- Radiotherapy of the chest: inflammation of the mucous membrane of the esophagus (esophagitis) and radiation pneumonitis, cardiac arrhythmias
- Radiation therapy of the head: swelling and pain of the neck and neck, increase in brain pressure, seizures, hair loss
- Radiotherapy of the pelvis: changes in urinary and stool behavior
In addition, the bone marrow can change, which affects the blood formation taking place there: A reduction in red blood cells (erythrocytes) leads to anemia with a feeling of weakness and reduced performance. The decrease in blood platelets (thrombocytes) affects blood clotting. The reduction in the number of white blood cells (leukocytes) increases the susceptibility to infections.
Fatigue, fever and loss of appetite are also possible side effects of radiation.
Most of these acute side effects go away completely after the end of radiation therapy.
Chronic radiation therapy side effects
Radiation therapy often also causes chronic side effects: The radiation mainly leads to a reactive increase in connective tissue (fibrosis). The consequences of this depend on the area being irradiated. Examples:
- Radiation therapy of the abdomen: bowel dysfunction (constipation, diarrhea)
- Radiotherapy of the chest: pulmonary fibrosis, heart failure
- Radiation therapy of the head: growth disorders due to hormone deficiency, hypothyroidism, "radiation caries" due to loss of function of the salivary glands, loss of cognitive functions
- Radiotherapy to the pelvis: sterility (infertility) due to the destruction of testicular or ovarian tissue
In addition, the bone marrow can change permanently.
Treatment of radiation therapy side effects
Treatment of the side effects of radiation therapy falls within the scope of supportive therapy. It is individually adapted to the needs of the patient.
For example, the very frequent nausea and the associated vomiting can be relieved with special drugs (antiemetics).
The increased susceptibility to infections can be counteracted, among other things, with careful hygiene and an environment that is as germ-free as possible. Sometimes those affected are also given antibiotics to prevent bacterial infections.
Anemia caused by radiation can be treated with blood transfusions.
In the case of malnutrition (e.g. as a result of swallowing difficulties), a high-calorie diet is important.
What do I have to consider after radiation therapy?
What to watch out for during and after radiation therapy depends very much on the type of radiation being given and, of course, the underlying disease. Talk to your doctor about what activities you are not allowed to do during and after radiation therapy, whether you are fit for work and what you need to consider with regard to your diet. In the long term, it is important to pay attention to the development of the chronic side effects of radiation therapy.
With every cancer treatment with radiation there is the risk that it will cause a second tumor - that is, a new tumor. This risk is small, but there is. The second tumor can develop years or even decades after radiation therapy. Regular check-ups are therefore recommended. Discuss this with your doctor.
In summary: Radiation therapy is now a widespread and well-established therapy method with a wide range of possible applications. It is particularly suitable for the treatment of malignant cancers (e.g. radiation after breast cancer).
Tags: digital health tcm first aid

















.jpg)