With the gene scissors against cancer
Dr. Andrea Bannert has been with since 2013. The doctor of biology and medicine editor initially carried out research in microbiology and is the team's expert on the tiny things: bacteria, viruses, molecules and genes. She also works as a freelancer for Bayerischer Rundfunk and various science magazines and writes fantasy novels and children's stories.
More about the experts All content is checked by medical journalists.Gene therapy is in the starting blocks: Using viruses as gene taxis and genetically modified immune cells, researchers have prepared for the fight against cancer.
Finally a miracle cure for cancer! Modified measles viruses kill tumor cells with a success rate of one hundred percent. But then it comes to a catastrophe: The virus mutates. Millions of people die, whoever survives becomes a zombie. This story about the virologist Dr. Robert Neville tells the Hollywood flick "I Am Legend" from 2007. The so-called oncolytic viruses that appear in the film are by no means science fiction. They are a form of gene therapy for cancer. And that's in the starting blocks.
Approval in the USA
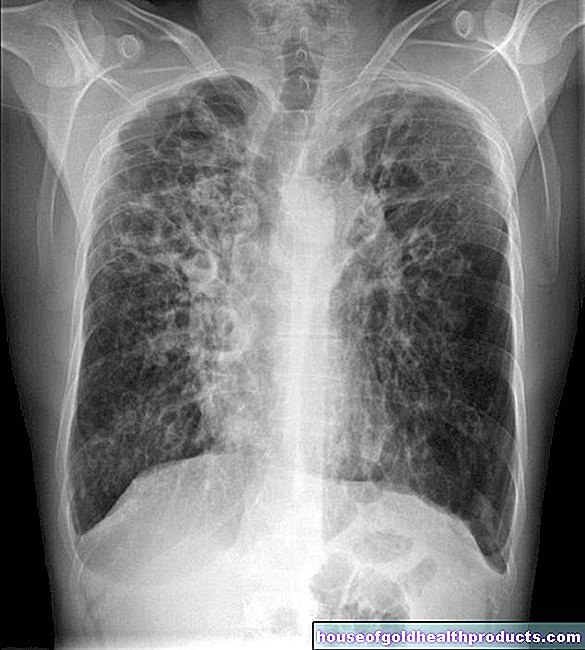
In October 2015, such a virus was approved for the first time in the USA to fight melanoma. This form of skin cancer is particularly malignant because it forms early metastases that spread through the lymphatic and blood vessels.
"Cancer is ultimately a genetic disease," explains Dr. Boris Fehse, Head of the Cell and Gene Therapy Research Department at the University Medical Center Hamburg-Eppendorf in conversation with “So it stands to reason that one also intervenes in the genome for therapy.” The central idea of classic gene therapy is to exchange a diseased gene for a healthy one. However, it is not that simple with cancer. “The changes in the genome are usually very complex,” says Fehse. The errors in the blueprint, so-called mutations, which allow cells to proliferate in an uncontrolled manner, are not just due to one gene, but to many different ones.
Introduced suicide genes
So many mistakes cannot be fixed with healthy genes. Instead, the scientists inject a so-called suicide gene into the tumor cells. These then die off and dissolve. This is why the method is also called “direct killing”. But somehow the suicide squad has to get into the cancer cells. The oncolytic viruses come into play here as a taxi for the genes. The scientists use the ingenious replication strategy of viruses to do this: They smuggle their genetic material into a host cell and use its replication apparatus to multiply.
In the fight against the highly aggressive black skin cancer, for example, a herpes virus is already being used that has been genetically modified so that it carries a suicide gene for the cancer cells.
The procedure was tested in a study with 436 patients. They all suffered from advanced melanoma that had spread and could no longer be operated on. The researchers injected the genetically modified viruses directly into the tumor. Over a period of several months. In 16.3 percent of the test persons, the malignant growth disappeared or at least receded. In the control group, this was the case for only 2.1 percent of the patients. “These patients had an extremely poor prognosis. Seen in this way, the result is very promising, ”explains Fehse.
Virus invasion of tumor cells
With the help of such oncolytic viruses, other cancer cells could also be killed in a very targeted manner in the future, but: "The biggest problem is really getting all of the tumor cells," explains Fehse. Because as long as cancer cells remained, they could continue to grow and multiply.
That is why viruses have been developed that can multiply in tumor cells. “This is a self-regulating process,” says Fehse, “as long as tumor cells are there, the viruses multiply, if all are defeated, they die.” The trick: the viruses are programmed in such a way that they react to specific features in the metabolism of the Tumor cells are dependent.Healthy body cells do not have these properties and are therefore not attacked.
In a bind
But there is another problem: when viruses multiply in the body, the immune system sounds the alarm. "Of course, the immune system cannot know that it is a 'good virus'," says Fehse. So it fights the rescuing viruses and eliminates them before they can complete their work. To prevent this, one could switch off the immune system. “But that would involve too great a risk,” explains the scientist. Because other pathogens would then have an easy time of it. Perhaps even more risky would be the strategy of building viruses that are not even recognized by the immune system. You could exterminate the tumor cells undisturbed. But if they should mutate at some point and attack healthy cells, the body would have no chance to defend itself - a scenario like in "I Am Legend".
In the case of the herpes viruses that were targeted at melanoma, the scientists found a compromise solution: so-called immune stimulators. The anti-cancer virus then also carries the information for a messenger substance that stimulates the patient's own immune system: the granulocyte-monocyte-stimulating factor GM-CSF. The immune system gradually eliminates the viruses, but thanks to the stimulation it then gives the tumor the rest of its own.
Armed immune cells
The second important form of gene therapy also targets the immune system: so-called immune therapy. It uses an ability that the immune system actually has anyway: namely, to switch off pathologically changed body cells every day. In addition to fighting pathogens, this is its most important task. Only when it does not meet these requirements for whatever reason does a tumor develop. "The question is: can we get it back?" Says Fehse. The idea: to arm the immune cells against cancer cells through genetic changes.
Immune cells identify friends and foes using certain proteins that are on the surface of cells: the so-called antigens. They do this with the help of specific receptors that, like the key to the lock, match the antigens and bind to them. T cells, for example, act as the memory of the immune system. Once the body has overcome an illness, the T cells in the future will be equipped with the right key to be able to quickly identify the pathogen in another case of infection.
Unmasked pests
With the help of genetic modifications, the scientists are now assembling receptors that match the respective cancer cells onto the T cells of cancer patients. As a result, the immune system exposes the cancer cells as pests and attacks them. “Of course, this only works if the tumor cells have surface structures that are not found on normal, healthy cells,” says Fehse.
Extinguished cancer
And that is the case, for example, with blood cancer. Patients have already been treated with this form of therapy in several studies, including in 2012 at the University of Pennsylvania. 30 patients with lymphocytic leukemia took part in the study, the majority of them children. All other therapies had not worked, and more than half had already had a bone marrow transplant. For the therapy, the doctors filtered the T cells from the patient's blood and then added a gene with the blueprint for the anti-tumor receptor to them in the laboratory. The changed immune cells were then given back to the patients in an infusion over three days. The results were astounding: the cancer regressed in 27 subjects, 19 remained cancer-free.
In Germany, too, cancer patients could soon benefit from gene therapies. “The oncological viruses will be approved in the next year or two,” estimates Fehse. Immunotherapy for blood cancer could go even faster. The researcher believes: "Maybe this year."
Tags: dental care prevention hair