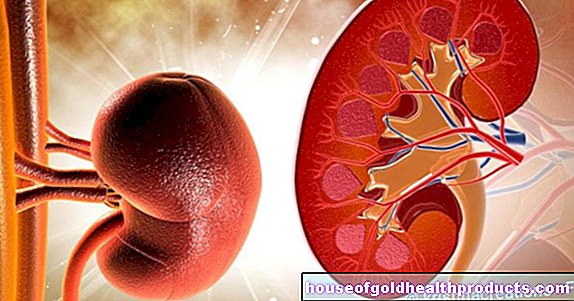
Kidney function
Dr. Manuela Mai studied medicine at the Universities of Heidelberg and Mannheim. After graduating, she gained clinical experience in gynecology, pathology and clinical pharmacology. She is particularly interested in the broader connections that lead to diseases - also outside of conventional medicine.She completed additional training in classical homeopathy as well as ear and skull acupuncture.
More about the experts All content is checked by medical journalists.The most important kidney function is the filtration of the blood and the excretion of so-called urinary substances - end products of metabolism that have to be excreted with the urine. But the kidney also fulfills a number of other functions.
Read everything you need to know about kidney function here!
The functions of the kidney
The kidney function is diverse. The kidneys function as an excretory organ and as hormone producers. In summary, the tasks of the kidney are as follows:
- Excretion of toxic substances
- Regulation of the water and electrolyte balance as well as the acid-base balance
- Hormone production
- Regulation of blood pressure (via the hormone renin produced in the kidney)
- Regulates the production of red blood cells (via the hormone erythropoietin produced in the kidney)
The excretory function of the kidney (urine production)
A major aspect of kidney function is urine production. This takes place in the nephrons (glomeruli) - the functional units of the kidney, which each consist of a kidney corpuscle (capillary tangle of vessels, enclosed by the Bowman capsule) and the associated tubular apparatus (kidney tubules). The formation of urine takes place in several steps:
Formation of the primary urine
The blood flows through the capillary loops of the kidney corpuscle and is filtered: The pressure prevailing here forces water and smaller blood molecules such as blood sugar (glucose) and urea through the pores in the capillary walls into the surrounding capsule (Bowman's capsule). In contrast, blood cells and other large molecules, such as most blood proteins, are retained in the capillaries when the kidneys are functioning normally.
The aqueous filtrate is called primary urine or glomerular filtrate. It is an almost protein-free ultrafiltrate. The kidneys produce 150 to 180 liters of primary urine per day.
Formation of the secondary urine
The primary urine is directed into the tubular system of each nephron. There it is decisively changed in its composition and strongly concentrated - around 99 percent of the filtrate is reabsorbed. The rest - about 0.5 to two liters per day - leaves the body as secondary urine. If the body were already excreting the primary urine, one would die within a short time from loss of water.
The reabsorption of substances dissolved in the primary urine and of water into the bloodstream takes place in different ways. Electrolytes such as chlorine, bicarbonate, sodium, calcium and potassium are actively returned. Water always flows back with it. The water therefore flows passively ("quasi in tow" of the substance transport) back into the bloodstream.
In addition to electrolytes, amino acids and glucose are also actively brought back into the blood.
The reabsorption of substances from the primary urine with good kidney function serves to keep the loss of these substances for the body to a minimum. However, if the concentration of the substances exceeds the absorption capacity of the tubular system, the excess is excreted with the secondary urine, even if the kidney function is adequate.
In the tubule system, however, not only are substances reabsorbed, but other substances are also specifically released from the blood system into the tubule (tubular secretion). As a result, the body accelerates the excretion of foreign substances such as drugs. But the body's own breakdown products such as uric acid are also eliminated from the body via this kidney function.
Excretion of urine
The tubule system finally merges into a collecting tube - together with the tubules of several other nephrons. In the collecting pipes, the secondary urine is concentrated even more under the influence of the hormone adiuretin through further dehydration. The urine passes through the collecting tubules into the renal pelvis and then via the ureters into the urinary bladder. From there the path leads to the outside via the urethra.
The regulation of kidney function
The following parameters must be correct for adequate kidney function:
Effective filtration pressure
This is the filter pressure, which is responsible for the fact that the blood plasma is pressed out of the kidney corpuscles into the Bowman capsule. It is calculated by subtracting from the prevailing blood pressure in the kidney corpuscle the two forces that counteract the blood pressure here: the hydrostatic pressure in the Bowman capsule and the colloid-osmotic pressure of the blood.
Glomerular Filtration Rate
This is the volume filtered per unit of time in the glomeruli of both kidneys. In young adults with normal kidney function, it is around 120 milliliters per minute. This corresponds to a filtrate volume of around 180 liters of primary urine per day. The driving force of glomerular filtration is the effective filtration pressure.
The kidney as an endocrine organ
The function of the kidney is not just to produce urine. Another kidney function is hormone production. The kidneys produce the two hormones renin and erythropoietin.
Renin
The hormone renin is produced in the area of the nephron and has a blood pressure-increasing effect.
If the blood supply to the kidneys is reduced (due to a drop in blood pressure or a narrowing of the renal artery), sodium deficiency or activation of the sympathetic nerve, increased renin is released. A complex interaction with other hormones (angiotensin I and II, aldosterone) ensures that more sodium and water are returned to the blood in the kidneys. In addition, renin leads to a significant constriction of the blood vessels.
Both mechanisms together increase arterial blood pressure.
Erythropoietin
Erytropoietin (also known as EPO) is a protein hormone that is increasingly excreted when there is a lack of oxygen. It increases the formation of new red blood cells in the bone marrow (erythropoiesis). This allows more oxygen to be transported in the blood. This regulation mechanism is activated, for example, when adjusting the altitude to high mountain air.
The kidney function in the water and acid-base balance
A healthy kidney function is also important for the water balance and the acid-base balance. Excess fluid and blood salts (electrolytes) are eliminated through the kidneys. If there is a lack of fluids or electrolytes, the kidneys ensure that less of them is excreted.
The kidney function in the area of the acid-base balance is based on the fact that the kidneys determine how many acids and bases are present in the body. This ensures that the blood is neither too acidic nor too alkaline (basic) - the pH value of the blood therefore remains in the normal range.
The consequences of impaired kidney function
Healthy blood pressure is essential for normal kidney function: excessively high blood pressure damages the kidney vessels in the long term and can therefore cause kidney disease. Conversely, high blood pressure can also be the result of kidney disease.
In the long run, disorders of kidney function can also lead to other diseases such as water retention in the tissue (edema), heart failure, cardiac arrhythmias, heart attacks and strokes.
Impaired kidney function can also trigger disorders of the nervous system and bone metabolism as well as anemia (due to erythropoietin deficiency). If the kidney function is disturbed during pregnancy, it can lead to premature birth, the death of the child in the womb or a deficiency birth (baby with underweight).
Tags: tcm skin care first aid