embolism
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.In the case of an embolus, a so-called embolus (e.g. blood clots, fat, cells or air) closes a blood vessel. Depending on which area of the body the embolism occurs, various symptoms such as severe pain or paralysis occur. Embolisms are sometimes life-threatening because, among other things, they lead to a heart attack or stroke. Read more about definition, causes, signs and therapy here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I82O88I26I28T79I74I27

Brief overview
- What is an embolism? Complete or partial occlusion of a blood vessel by the body's own or foreign material (e.g. blood clots) that gets into the bloodstream.
- Symptoms: Depending on which blood vessel is affected, different symptoms arise. Sudden pain is common; but sometimes those affected are also symptom-free.
- Causes: A blood clot (thrombus) that detaches from the vessel wall and enters the bloodstream is often the trigger for an embolism (thromboembolism).
- Treatment: The doctor usually treats an embolism with medication, in some cases also surgically. The aim of therapy is to dissolve or remove the embolus.
- Prevention: exercise regularly, drink enough, avoid being overweight, stop smoking; if necessary thrombosis prophylaxis e.g. after operations (anticoagulant drugs, compression stockings)
- Diagnosis: conversation with the doctor, physical examination (including ultrasound, CT, MRI, angiography)
What is an embolism?
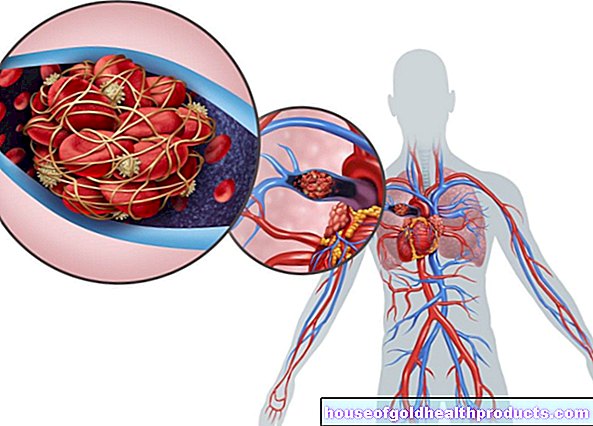
The term embolism comes from the Greek (“embolla”) and means “to throw in”. In the case of an embolism, a plug ("embolus" = vascular plug, plural "emboli") that is washed in via the blood blocks a blood vessel. It prevents the blood from flowing freely through the vessel.
As a result, the affected area is no longer adequately supplied with oxygen and important nutrients. Over time, the tissue there dies, and sometimes life-threatening consequences such as a heart attack or stroke occur. In Germany, 20,000 to 25,000 people die of embolism every year.
An embolus only causes an embolism if its diameter is larger than that of the blood vessel.
What types of emboli are there?
An embolism develops in the affected person in both the veins and the arteries. Emboli also form in both blood vessels. Doctors therefore differentiate between arterial and venous embolisms.
Arterial embolism
In the case of an arterial embolus, the embolus usually comes from the left atrium of the heart or a large artery (arterioembolic embolus), such as the main artery (aorta) or pulmonary artery (pulmonary artery). Often there, an embolus closes a vessel to the brain (cerebral embolism), to the arms or legs (arm or leg embolism) or to organs such as the intestine, kidneys or spleen (intestinal, kidney or splenic infarction). In most cases, an arterial embolus causes an embolus to reach the brain (cerebral embolism), where it triggers a stroke.
Affect arterial emboli
- about 60 percent the brain
- about 28 percent the legs
- about 6 percent of the arms
- about 6 percent the organs (e.g. intestines, kidneys, spleen)
Venous embolism
With a venous embolism, the vascular plug forms in the veins - preferably in the legs or in the pelvis. It enters the lungs through the right ventricle and pulmonary artery, where it often causes pulmonary embolism.
Paradoxical embolism
The paradoxical embolism - also crossed embolism - is a special form of embolism. The embolus arises in a vein and blocks an artery (but not the pulmonary arteries!). This is only possible if the embolus gets into the left ventricle through gaps or small openings in the heart septum (e.g. due to a congenital heart defect). This means that the embolus does not go to the lungs like a conventional venous embolus, but to the arterial system of the bloodstream.
How is an embolism different from a thrombosis?
In a thrombosis, a blood clot (thrombus) closes a blood vessel right where it originates. By definition, however, an embolism does not occur where an embolus forms. In some cases, however, a thrombus develops into an embolus.
The thrombus detaches itself from the inner wall of the vessel on which it originated and moves through the body via the bloodstream. If this dragged-on plug (“embolus”) clogs a vessel at another point in the body, doctors speak of an embolism (or thromboembolism).
What are signs of an embolism?
Emboli cause very different symptoms depending on where they occur in the body. While some do not make themselves noticeable at all, others lead to numerous complaints and omens. Basically, people with an embolism have severe pain that occurs suddenly. The embolus disrupts the blood supply, which means that the affected organ no longer functions properly. In some cases, the tissue in the affected area even dies.
In some areas of the body that have good bypass circuits (collaterals) and supply the affected area via other vessels, it is also possible that people with a small embolism do not have any symptoms.
Embolism in the legs or arms
When an embolism develops in a large artery in the leg or arm, the symptoms are usually very typical. They can be characterized by the "6P" (after Pratt; six physical signs):
- Pain
- Paleness
- Paresthesia (disorder of feeling)
- Pulselessness (pulse failure)
- Paralysis
- Prostation (shock)
In severe cases, an embolism in the arm or leg means that the affected person is no longer able to move their arm or leg.
Embolism in the lungs
Pulmonary embolism is manifested by pain in the lungs, sudden shortness of breath (dyspnea), rapid breathing (tachypnea), racing heart (tachycardia), feeling of tightness, acute drop in blood pressure (hypotension) and circulatory shock. With the appropriate size, an embolus in the lungs overloads the heart and leads to death.
Embolism in the brain
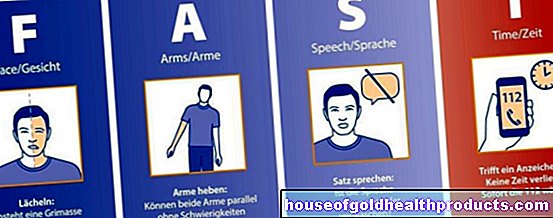
A brain embolism causes a stroke. In those affected, this manifests itself, for example, through paralysis (often on one half of the body), speech disorders and impaired consciousness.
Embolism in the heart
In rare cases, an embolus blocks the coronary arteries and causes a heart attack in those affected. In some severe cases, an embolism in the heart leads to heart failure.
Embolism in the internal organs
An embolism in the area of the internal organs triggers different symptoms depending on the organ affected:
Kidneys
If the kidneys are affected by an embolism, this often leads to a kidney infarction. Those affected usually have severe pain in the lumbar region and blood in the urine (hematuria). In extreme cases, kidney function fails completely (kidney failure).
spleen
A vascular occlusion in the spleen causes a splenic infarction. Typical signs are sudden pain in the upper left abdomen and pain in the left shoulder. The chest of those affected usually rises and falls less noticeably when breathing. Sometimes rubbing noises can be heard around the spleen while breathing (perisplenic rubbing). In severe cases, the spleen fails to function.
colon
In the intestinal mesentery - the band of connective tissue that fixes the intestine in the abdomen and in which the blood vessels and nerves run to the intestine (so-called mesentery) - an embolism causes severe abdominal pain in those affected. They also often have bloody diarrhea and fever. The bowel movements are also often reduced or fail completely. In extreme cases, the affected section of the intestine dies.
Typically, the larger the area that the embolism excludes from the blood supply, the more severe the symptoms.
What causes an embolism?
There are different causes for an embolism. The embolus, which blocks the vessel and thus triggers an embolism, usually consists of the body's own substances such as fat droplets, amniotic fluid, blood clots (thrombi) or air bubbles. In some cases it also consists of foreign materials such as foreign bodies (e.g. parts of a hollow needle) or parasites (e.g. tapeworms).
Emboli can therefore be divided into:
- Solid emboli, which for example consist of blood clots, tissues, parasites or tumor cells.
- Liquid emboli, e.g. consisting of drops of fat or amniotic fluid.
- Gaseous emboli, e.g. consisting of air bubbles.
Depending on the cause, the following embolisms can be distinguished:
Thromboembolism
The most common form of embolism is thromboembolism. It is caused by a blood clot (thrombus) that separates from the vessel wall and enters the bloodstream. This embolus then moves with the bloodstream through the body until it gets stuck somewhere and closes a vessel. It comes to thromboembolism.
Doctors differentiate between venous and arterial thromboembolism.
Venous thromboembolism (VTE)
In venous thromboembolism, the embolus comes from a vein. It often forms in the veins of the pelvis or legs (e.g., venous thrombus in the leg). This often happens when those affected sit or lie down for too long and the blood no longer circulates properly. This causes the blood to stagnate in some cases.A blood clot (thrombus) forms, which hinders the blood supply at this point and, in extreme cases, completely closes the vessel. This may also be the case if those affected do not drink enough fluids (desiccosis).
The risk of venous thromboembolism is increased if someone is bedridden (e.g. people in need of care), after an operation (e.g. if they lie down a lot afterwards) or if those affected have phlebitis (thrombophlebitis).
Arterial thromboembolism (ATE)
In arterial thromboembolism, the embolus comes from an artery. It usually arises in the left half of the heart. When the embolus loosens, it often gets to the brain (brain embolism) and causes a stroke.
Heart disease is the most common cause of arterial thromboembolism, accounting for up to 90 percent. These include, for example:
- Arteriosclerosis ("hardening of the arteries"); the blood vessels narrow due to deposits of blood components (e.g. cholesterol, white blood cells)
- An injury or scarring of the inner lining of the blood vessels (endothelium)
- Clotting disorders (thrombophilia)
- Inflammation of the lining of the heart (endocarditis)
- Expansion of the heart wall (aneurysm)
- Atrial fibrillation; the heart beats irregularly too fast or too slowly
The most common embolisms are thromboembolism, which occurs after thrombosis of the deep veins in the leg (pulmonary embolism), and thromboembolism in the arteries of the brain (stroke).
Tumor embolism
A tumor embolism occurs when cancer cells (tumor cells) or cancer tissue are carried over. The embolus (or the so-called metastatic embolus) makes it possible for daughter tumors to form in other areas of the body.
Tumor embolisms are common in people with advanced cancer. The reason for this is that cancer increases the blood's ability to clot. This means that the blood coagulates faster. The more aggressive the cancer, the higher the risk of thrombosis and, subsequently, of embolism.
Fat embolism
A fat embolism is an embolism caused by fat droplets in the bloodstream. Fat embolism often occurs after bone fractures (especially long bones such as the ribs) when the bone marrow is also damaged. This consists, among other things, of fat, which sometimes leaks out in the event of an injury and gets into the bloodstream. Other causes of a fat embolism include: blunt injuries (e.g. bruises), burns, fatty liver or operations such as an amputation or a bone marrow transplant. Most often, a fat embolism forms in the blood vessels in the lungs (pulmonary fat embolism).
Bone marrow embolism
In the case of broken bones (fractures), in some cases, tissue from the bone marrow enters the vascular system and triggers an embolism there. This type of embolism therefore often occurs in fractures of long bones that contain bone marrow. These include, for example, the upper arm bone (humerus), the forearm bones ulna (ulna) and spoke (radius) and the thigh bone (femur).
Bacterial embolism (septic embolism)
In a bacterial embolism, bacteria enter the bloodstream and trigger an embolism. This happens, for example, as a result of blood poisoning (sepsis) or inflammation of the inner lining of the heart (endocarditis). A septic embolus can lead to a purulent infection of the affected tissue.
In contrast to the septic embolus, a so-called bland embolus is not infected with bacteria.
Gas embolism
A gas embolism occurs when gas bubbles enter the bloodstream and narrow or close the vessel. If the gas is air, it is called an air embolism. A gas embolism can occur, for example, when a medium-sized or large blood vessel is injured (e.g. the superior vena cava, superior vena cava), when air is introduced into a blood vessel (air insufflation) or through a tear in the lung (lung rupture).
A life-threatening gas embolism can also occur in the event of a so-called decompression sickness (decompression sickness). Gas bubbles form in the blood vessels when the external pressure decreases too quickly. This can happen, for example, if you emerge from the water too quickly (diving illness) or if you ascend too quickly.
Amniotic fluid embolism
If amniotic fluid reaches the mother's bloodstream via the uterus during childbirth, amniotic fluid embolism occurs (also called “obstetric shock syndrome”). This is a rare but life-threatening complication of childbirth that often leads to brain damage in mothers and children. The exact cause of an amniotic fluid embolism has not yet been clearly clarified.
Parasitic embolism
With a parasite embolism, parasites clog the vessel. Often these are tapeworm larvae that enter the gastrointestinal tract. There they pierce the intestinal wall and get into the blood.
Foreign body embolism
In a foreign body embolism, foreign bodies enter the bloodstream. This is the case, for example, if parts of examination tools such as catheters (tubes that are inserted into organs) or cannulas (hollow needles) break off during an examination and get into the bloodstream. Other foreign objects include shrapnel or pellets.
What are risk factors for embolism?
There are several factors that increase your risk of embolism. One of the most important risk factors for thromboembolism, for example, is heart disease - especially atrial fibrillation, in which blood clots form in the atria. Risk factors are also:
- smoking
- High fat diet
- Little physical exercise
- Vascular and heart diseases, e.g. arteriosclerosis, heart failure
- Diabetes (diabetes mellitus)
- High blood pressure (hypertension)
- Morbid overweight (obesity)
- Cancers
- Operations
- Use of female hormones (e.g. hormonal contraception, hormone replacement therapy)
- Increasing age
- Insufficient movement of the legs (due to bed rest, paralysis, rigid bandages or during long journeys, especially air travel)
- Pregnancy and the puerperium
- Severe injury
- Previously suffered embolisms
- Venous diseases, e.g. phlebitis, varicose veins (varices)
- Female gender (women are more often affected than men)
In principle, the same risk factors apply to emboli as to thrombosis.
What can you do about an embolism?
The aim of embolism therapy is to ensure that sufficient blood flows through the blocked vessel again. To do this, doctors administer anticoagulant drugs. In severe cases, the blood clot is dissolved with medication (drug thrombolysis) or surgically removed (embolectomy).
Medication
In the event of an embolism, especially pulmonary embolism, rapid medical treatment is important. The doctor gives the patient anticoagulant medication (anticoagulants, e.g. heparin) as a syringe or infusion. They ensure that the embolus does not enlarge and that no new blood clots form.
In severe cases, medication is used to dissolve the blood clot. To do this, doctors administer so-called fibrinolytics (medicinal thrombolysis).
In order to prevent a new thromboembolism, the patient is then given anticoagulant medication in tablet form for several months (e.g. so-called DOAK or vitamin K antagonists such as phenprocoumon). This is called oral anticoagulation, which translates as "anti-coagulation through medication". The anticoagulant drugs are effective, but there is some risk of bleeding. Some patients therefore receive acetylsalicylic acid (e.g. ASA 100 mg) as a long-term therapy to prevent blood clots and at the same time to keep the risk of bleeding low.
Removal of the embolus using a catheter
If drug thrombolysis is not possible, doctors use a catheter to remove the blood clot. You carefully push the catheter through a vein up to the blocked blood vessel. With small instruments or a drug (thrombolytic), which they insert into the catheter, they dissolve the embolus.
Surgery (embolectomy)
The last option to remove the blood clot is what is known as surgical embolectomy. Doctors remove the embolus in an open operation. In the event of a pulmonary embolism, the patient is connected to general anesthesia and a heart-lung machine.
How can you prevent an embolism?
If you want to prevent embolism, it is important that you keep the risk as low as possible by doing the following:
Lifestyle changes
- If you are a smoker, quit smoking.
- Avoid being overweight and eating a balanced diet.
- Drink enough fluids (at least one and a half to two liters per day)
- On long flights or car journeys, make sure you get regular exercise.
- Go to your family doctor's regular check-ups so that diseases such as high blood pressure or diabetes mellitus can be identified and treated at an early stage.
- After surgery, get up as soon as possible after consultation with the attending physician and exercise enough.
Prevent thrombosis
Because every injury activates blood clotting, operations also increase the risk of thrombosis or embolism. In pregnant women, childbirth also increases the risk of thrombosis or embolism. That is why doctors often prescribe heparin injections after an operation or childbirth, which those affected usually inject under their skin once a day. Heparin inhibits blood clotting and thus prevents thrombosis and embolism.
To prevent an embolism, the doctor also often prescribes compression stockings ("thrombosis stockings"). As a rule, those affected put these stockings on in the morning after getting up and take them off again in the evening before going to bed. They can also be worn continuously. Compression stockings support better blood flow in the leg and thus prevent thrombosis.
The duration of this thrombosis prophylaxis depends on the individual risk.
In the case of certain diseases (e.g. severe circulatory disorders in the arteries), those affected are usually not allowed to wear compression stockings. Therefore, ask your doctor beforehand whether thrombosis stockings are suitable for you.
How does the doctor diagnose an embolism?
The first point of contact if an embolism is suspected is the family doctor. If he suspects an embolism behind the symptoms, he usually refers the person affected to a hospital. There, a specialist in internal medicine (internist) specializing in vascular diseases (angiologist or phlebologist) continues to treat those affected.
Embolism is often life threatening. It is therefore important that the doctor immediately clarifies symptoms that indicate an embolism and acts accordingly.
Talk to the doctor and physical examination
Since the symptoms of an embolism are sometimes ambiguous, it is important that the doctor examine the patient carefully. To do this, he first conducts a detailed discussion (anamnesis) with the person concerned. For example, he asks him about the symptoms and whether an operation has recently taken place or whether he has ever had a blood clot. He will then perform a physical exam on him. Often this already gives indications of the diagnosis. If, for example, the doctor notices sudden pain and pale skin as well as a missing pulse and vascular noises in the arms or legs, these are already clear signs of an embolism in the arm or leg.
Blood test
A blood test is also part of the diagnosis of an embolism. Certain blood values confirm the suspicion of an embolism. These include the so-called D-dimers. D-dimers are proteins that are produced when a blood clot breaks down. If they are elevated, this is an indication that a blood clot, i.e. a thrombosis or embolism, is breaking down somewhere in the body.
Ultrasound, CT, MRI
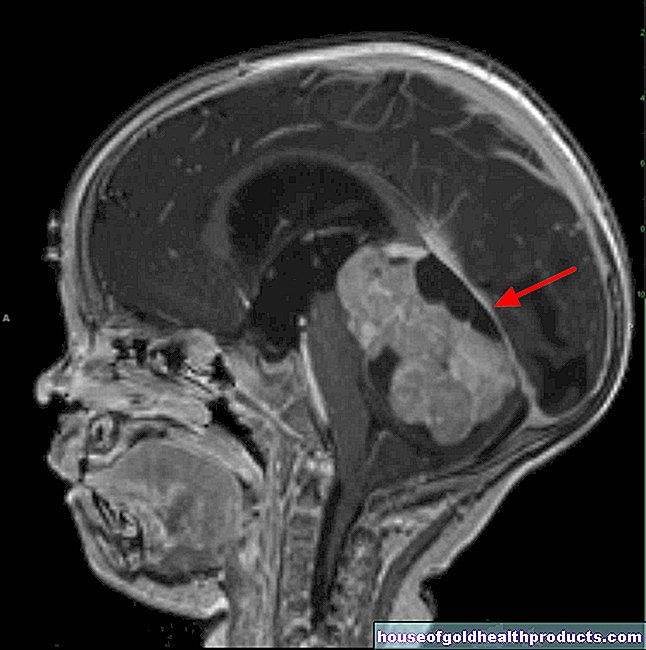
If the examination confirms the suspicion of an embolism, the doctor carries out an imaging examination, e.g. using ultrasound (sonography), computed tomography (CT) or magnetic resonance imaging (MRT).
For example, during an ultrasound examination of the vessels (color duplex sonography), the doctor can see whether the vessel wall is narrowed. He also uses ultrasound to determine the direction in which the blood flows in the vessels and how fast the blood flows through the vessels (flow speed). The latter gives the doctor information about whether there are constrictions or obstructions in the vessels.
Angiography
With the help of computed tomography or magnetic resonance tomography, the doctor takes pictures of the vessels and the vascular system (so-called CT angiography or MRT angiography). To do this, the doctor injects contrast agent (iodine-containing, water-clear and colorless liquid that is visible in the X-ray image) into the blood vessel and then performs the computed tomography or magnetic resonance tomography. The interior of the vessels is then visible in the CT or MRT image. In this way, the doctor recognizes whether an embolus is clogging a vessel or whether the arterial wall has changed (e.g. narrowed) due to other causes such as arteriosclerosis (hardening of the arteries).
Scintigraphy
If an embolism in the lungs is suspected, a nuclear medical examination, the lung scintigraphy, is useful. The examination consists of two parts: First, the doctor examines the ventilation of the lungs. The patient must inhale a weakly radioactively labeled gas. This measures the distribution of activity in the lungs.
The doctor then examines the blood flow in the lungs. To do this, he injects weakly radioactive protein particles into a patient's vein. These get into the lungs with the bloodstream, where they get stuck in some of the finest blood vessels. With a special camera (gamma camera, SPECT) the doctor makes these visible and takes pictures. He can then tell where the blood clot has reduced blood flow.
Tags: eyes desire to have children drugs