Medulloblastoma
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
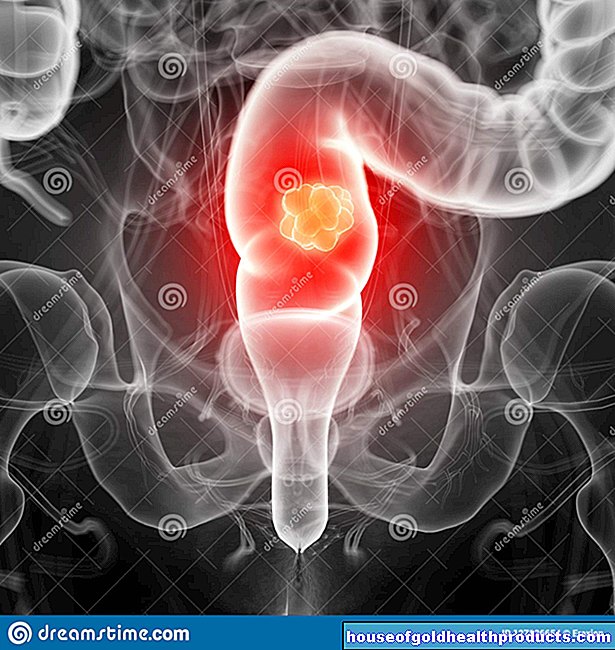
More about the experts All content is checked by medical journalists.Medulloblastoma is the most common malignant brain tumor in children and adolescents. It grows very quickly in the area of the cerebellum and often causes increased intracranial pressure with headaches and nausea. The tumor can be operated on, irradiated, and treated with chemotherapy drugs. About half of those affected can be cured with this intensive therapy. Here you can read everything you need to know about medulloblastoma.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D43C71D33

Medulloblastoma: description
With a share of 20 percent, medulloblastoma is the most common malignant brain tumor in children and adolescents. In a big city like Cologne with around one million inhabitants, around five children under the age of 15 fall ill every year. Most often, medulloblastoma is diagnosed between the ages of five and eight. Boys are more often affected than girls. The tumor is much less common in adults. The medulloblastoma only makes up about one percent of all brain tumors in them.
The tumors mainly develop in the posterior fossa. In children they are mostly in the middle, in adults they are more likely to be found laterally in the cerebellum. In many of those affected, the medulloblastoma grows into the cerebral waterways. This allows tumor cells to spread very easily via the cerebral fluid in the rest of the brain and also in the spinal canal. If these cells settle in a new location and form a daughter tumor there, one speaks of metastases. In every third person affected, the medulloblastoma had already spread at the time of diagnosis. Most of the tumor settlements are in the central nervous system (brain and spinal cord). Very rarely do they arise in a bone or in the bone marrow.
The medulloblastoma enlarges very quickly and can grow into the surrounding tissue. Therefore, it is classified as very malignant (grade IV) by the World Health Organization (WHO). In addition, medulloblastomas are broken down again according to their tissue type:
- classic medulloblastoma
- desmoplastic medulloblastoma
- nodular (nodular) medulloblastoma
- anaplastic medulloblastoma
- large cell medulloblastoma
Therapy and prognosis can differ between these individual tumor types.
Medulloblastoma: symptoms
Since a medulloblastoma grows very quickly, symptoms develop early on. The tumor takes up space in the head and often obstructs the cerebral waterways - that is, the cerebral water can no longer drain properly. It builds up, which increases intracranial pressure, and a head of water (hydrocephalus) can develop. Headache, morning sickness and vomiting, and dizziness in particular are typical signs of the pressure increase in the skull. In addition, those affected may find it difficult to concentrate, feel tired and have trouble sleeping. Some develop vision problems.
The medulloblastoma mostly displaces cerebellar structures. As a result, patients often cannot coordinate their movements properly and have difficulty walking. In principle, different muscle groups can also be paralyzed.
Medulloblastoma: causes and risk factors
The medulloblastoma is formed from embryonic cells (i.e. from very immature and undifferentiated cells) of the central nervous system. It has not yet been clarified why such cells suddenly begin to multiply in an uncontrolled manner. However, it has been observed that the tumor occurs more frequently in connection with certain chromosome changes. Ionizing radiation is considered a risk factor for a medulloblastoma: Children who have already had to be irradiated because of another malignant disease are therefore at an increased risk of the disease.
Medulloblastoma: examinations and diagnosis
Patients with symptoms of brain cancer often go to their family doctor or pediatrician first. He asks about the exact complaints and their course. If he finds evidence of a malignant tumor in the central nervous system, he usually refers the patient to a specialized center for cancer (oncology) for further examinations. Doctors from different disciplines work together there to make the correct diagnosis. For this, an exact survey of the medical history (anamnesis) and various examinations are necessary. The most important :
MRI and CT
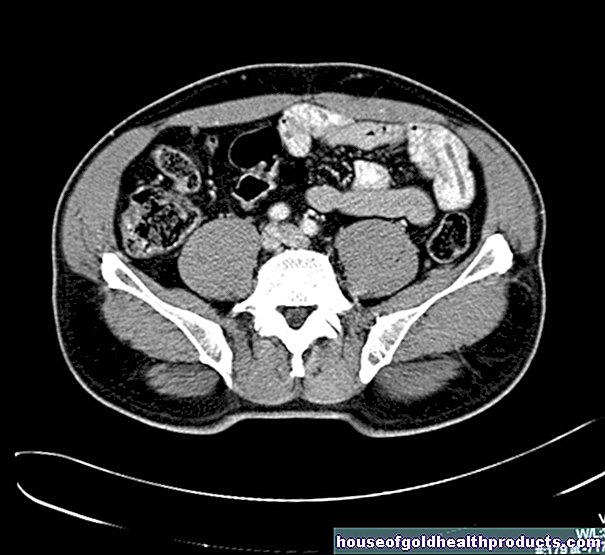
The best way to visualize a medulloblastoma is magnetic resonance imaging (MRI). Most often, a contrast agent is injected into a vein of the patient before the examination. The tumor absorbs this contrast agent and lights up irregularly in the MRI image. This allows you to determine its location, size and extent very well. Since a medulloblastoma can also spread into the spinal canal, an image is also taken of the head.
If an MRI is not possible for certain reasons or if a quick diagnosis has to be made due to an emergency situation, the brain is visualized using computed tomography (CT).
Examination of the cerebrospinal fluid
The cerebral water examination (liquor diagnosis) supplements a detailed diagnosis in medulloblastoma. The doctor takes some cerebral fluid with a fine hollow needle, usually from the spinal canal (lumbar puncture). The sample is examined for tumor cells and thus for the presence of metastases in the spinal cord.
biopsy
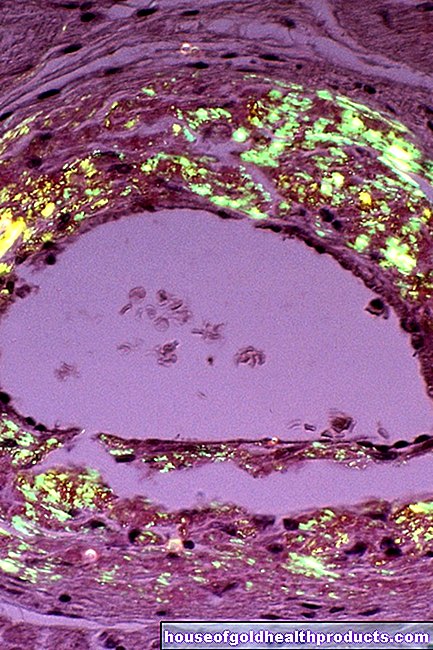
In addition, a tissue sample is usually taken from the tumor (biopsy) and examined under a microscope. This is necessary in order to be able to optimally design the subsequent therapy for the patient.
Medulloblastoma: treatment
Because of its malignancy, medulloblastoma requires rapid and intensive treatment.
Medulloblastoma: surgery
The treatment of choice for medulloblastoma is surgery. The surgeons try to remove the entire tumor if possible. Since the medulloblastoma mostly grows into the surrounding brain structures, this goal can almost never be achieved. That is why more and more treatments follow after an operation.
Medulloblastoma: radiation and chemotherapy
If there are no tumor deposits (metastases), children are irradiated for three to five years after the operation in the area of the head and spinal cord and then treated with chemotherapeutic agents. This should also destroy individual tumor cells in the cerebral waterways.
If the medulloblastoma has already metastasized, an individual and more intensive treatment plan is developed.
Children under three to five years should not be irradiated if possible. You will receive chemotherapy immediately after the operation. In most cases, several drugs that are supposed to kill the cancer cells are combined with one another. Examples are chemotherapy drugs such as vincristine, CCNU and cisplatin.
Shunt implantation
Sometimes the medulloblastoma obstructs the cerebral waterways. If these cannot be reopened even after an operation, the brain water must be artificially drained. To do this, the surgeons place a small tube in the cerebral waterways (liquorshunt). The brain water can then either drain into an outer container or into the body. In 80 percent of cases, the liquorshunt does not have to be left on permanently. As soon as the brain water drains sufficiently on its own, it can be removed again.
Accompanying therapy measures
In addition, intracranial pressure symptoms can be treated with the cortisone preparation dexamethasone. Most often it is used during the period of surgery and radiation therapy.
Depending on the symptoms, the acute treatment in the hospital can be followed by rehabilitation measures. Most hospitals also offer psychosocial care for patients and their families.
Examination and treatment
You can read more information about examination and treatment in the article Brain Tumor.
Medulloblastoma: disease course and prognosis
The course of the disease and the prognosis for a medulloblastoma depend on various criteria. It is beneficial if the tumor can be completely surgically removed, there are no metastases and there are no tumor cells in the cerebral fluid. If individual tumor cells remain in the head after the operation, the tumor can grow again (relapse). Relapses usually occur in the first three years, but in rare cases can occur ten years after successful therapy. Therefore check-ups should be carried out for all patients years after a successful therapy. With intensive therapy, more than half of children with medulloblastoma can be cured today.
Tags: prevention travel medicine dental care








-warten-auf-den-piks-der-freiheit.jpg)