Amyloidosis
All content is checked by medical journalists.Amyloidoses are diseases in which proteins form poorly soluble, pathogenic deposits. This leads to malfunctions and various symptoms. In some cases they are limited to certain organs or body regions - in others they affect the entire organism. Read here how the disease progresses, which signs indicate amyloidosis and how it is treated!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E85
Brief overview
- What is amyloidosis? Amyloidosis is a disease caused by protein buildup. Different organs are affected.
- Forecast: It is not possible to make a general statement on this. In addition to the subtype, it primarily depends on how many organs are affected.
- Symptoms: Different symptoms depending on the organs affected
- Risk factors: In addition to genetic risk factors, chronic inflammatory diseases, chronic infections and blood diseases increase the likelihood of developing amyloidosis.
- Diagnosis: blood count, urine test; Taking tissue samples to be examined in the laboratory
- Treatment: Treatment of the underlying disease causing it; Medicines that may reduce protein deposition
- Prevention: Rapid treatment of chronic inflammatory diseases and chronic infections
What is amyloidosis?
In amyloidosis, proteins accumulate in the spaces between cells. They form microscopic fiber structures, so-called fibrils. The name "amyloidosis" indicates something special. In Greek, "ámylon" stands for strength. This is because the deposits react in the laboratory in a similar way to starch granules: they turn blue in an iodine solution.
Strictly speaking, the term amyloidosis does not describe a specific disease, but a deposit of different proteins that leads to symptoms. Scientists have now found more than 30 of these proteins. Triggers are, for example, certain diseases or changes in the genetic make-up, which lead to the fact that poorly soluble proteins are increasingly deposited. Amyloidosis affects different organs.
causes
Background: Proteins consist of individual amino acids. They are strung together like threads during protein production. Many of these proteins are present in dissolved form in the blood or in organs. In amyloidosis, their concentration increases sharply for various reasons and the proteins are deposited. Certain changes in the genome lead to altered proteins with different properties that are deposited. In addition, the natural aging process sometimes favors development.
Classification, distribution and frequency
Amyloidosis is not a uniform clinical picture. There are localized amyloidoses with deposits in one area of the body or impairments throughout the body (systemic amyloidoses). There are no reliable figures on the frequency for Germany. Scientists cite one case per 100,000 population for systemic amyloidosis in Great Britain. Other research groups found five to 13 cases per 100,000 people for western industrialized nations.
The amyloidoses are divided into the following groups (subtypes) according to frequency, type and cause:
AL amyloidosis: This is the most common form, accounting for 68 percent of all amyloidoses. "AL" means "amyloid, consisting of light chains". Special cells in the bone marrow (plasma cells) that produce antibodies are affected. Antibodies consist of two light and two heavy chains, i.e. large and small protein chains.
In AL amyloidosis, plasma cells produce large quantities of modified light chains that are deposited. The changes in the light chain protein are often caused by a tumor in the lymph tissue (lymphoma). This form of amyloidosis usually occurs locally. The heart or kidneys are often affected.
AA amyloidosis follows in second place with an incidence of about twelve percent. It is triggered by the so-called acute phase protein. This is a protein that is produced in the body after injuries or infections. Some viruses, bacteria, inflammatory bowel diseases or cancers lead to this form. Symptoms usually occur in the kidneys, spleen, liver, adrenal glands and in the gastrointestinal tract.
ATTR amyloidosis follows with a frequency of 8.8 percent. This is about transthyretin as a trigger for amyloidosis. This is a protein that is produced in inflammation and is very unstable. The deposits are the cause of old age amyloidosis in seniors. This type of amyloidosis can be hereditary. Symptoms mainly occur in the eyes, kidneys, heart and rarely in the central nervous system.
Much less often patients suffer from A-Beta2-M amyloidosis, also known as AB amyloidosis (1.8 percent). The name suggests the protein beta2-microglobulin. It has a tendency to form fibrils: a problem that occurs particularly in patients on long-term dialysis. Those affected mainly report pain in the joints. Carpal tunnel syndrome also occurs in many cases.
AFib amyloidosis is similarly rare (1.7 percent). Doctors also speak of hereditary fibrinogen Aα chain amyloidosis because the deposits can be traced back to changes in the gene for fibrinogen. Fibrinogen is a protein that plays a central role in blood clotting. Clumping occurs mainly in the kidneys. The consequences range from mandatory dialysis to kidney transplants.
Can you die from it?
The following also applies to questions about the course and prognosis: amyloidosis is not a uniform clinical picture and general statements are not possible. In addition to the subtype, the individual situation plays a role here. The fewer organs that are affected, the better the prognoses.
Scientific studies only give mean values; the numbers differ individually. Therefore, always talk to your doctor. With standard therapies, patients with AL amyloidosis survive an average of three years and with AA amyloidosis an average of four years. Studies have shown that people with AA amyloidosis have very different disease courses - depending on the amount of the triggering protein, serum amyloid A. With ATTR amyloidosis and after a successful liver transplant, more than half of all patients are still alive after 20 years.
Is amyloidosis hereditary?
There are different amyloidoses. The two most common forms are not inheritable. AA amyloidosis is caused by some inflammations, infections, or cancers; hereditary factors do not play a role here. AL amyloidosis is caused by certain blood disorders and is not directly inherited. Patients on long-term dialysis occasionally develop AB amyloidosis. It is due to the treatment.
Hereditary forms include ATTR amyloidosis, also known as ATTRv amyloidosis. The cause is changes in the genes for the protein transthyretin. So far, experts have known more than 80 such mutations. AFib amyloidosis is also a familial form. Changes in the gene for fibrinogen are inherited.
Regardless of whether it is inherited or acquired - it is equally true of all amyloidoses that those affected form too many poorly soluble proteins, which are deposited and ultimately make you sick. Many of these proteins are present in dissolved form in the blood or in organs. Different metabolic diseases, chronic inflammations or chronic infections cause their concentration to rise sharply until they can no longer dissolve.
In the case of inheritable forms, changes in the genetic code are the cause: modified proteins with different properties are formed and deposited. In many cases, aging is also behind such changes. Proteins get into the spaces between cells. They gather together and form what are known as beta sheets. These are accordion-like folded structures. Ultimately, microscopic fibers are created that are very resistant. They are deposited and are not removed by the body's own phagocytes.
The deposits disrupt the architecture of tissues and are toxic to the cells. This leads to restrictions in organ function, for example in the heart, in the kidneys or in the central nervous system.
What are the symptoms of amyloidosis?
The symptoms of amyloidosis vary from person to person. The spectrum ranges from complete freedom from symptoms right at the beginning to severe, life-threatening symptoms when the disease is very advanced. Depending on which organ is affected, different symptoms develop.
Symptoms of kidney involvement
Poorly soluble proteins form either on the capillary vessels of the kidney corpuscles or on the incoming and outgoing vessels of the kidneys. Patients often notice that their urine foams a lot. The kidney is no longer working properly and water builds up (edema).
Symptoms of cardiac involvement
The proteins are also deposited on the heart muscle, which worsens the pumping capacity. Heart failure (heart failure) occurs. The heart pumps too little blood to supply the body. Sometimes the walls of the heart chambers thicken. Patients are short of breath, have low blood pressure, and suffer from general weakness. Doctors then speak of cardiac amyloidosis.
Symptoms of brain and central nervous system involvement
Protein deposits in the brain lead to various symptoms that doctors are familiar with from patients with Alzheimer's disease. Those affected have problems memorizing information and learning new things while long-term memory is still working. As the disease progresses, fine motor skills and language deteriorate.
If the deposits form on the nerves outside of the brain, many sufferers develop movement disorders or abnormal sensations. Depending on the location of the deposit, people with amyloidosis may have problems emptying their stomach, intestines and / or bladder properly. Erectile dysfunction is also common.
Symptoms when various soft tissues are involved
Soft tissues perform very different tasks in the body. If proteins are deposited in amyloidosis, this leads to various complaints. These include swollen, painful joints, nodules under the skin, changes in fingernails or toenails, hair loss and discomfort in the hand caused by carpal tunnel syndrome.
A dry feeling in the mouth and throat with hoarseness, a swollen tongue, and difficulty swallowing suggest amyloidosis. The eyes are also often affected: dry, reddened eyes are just as possible as opacities of the vitreous humor or glaucoma. These are a group of eye diseases that damage the optic nerve and eventually reduce the person's vision.
Symptoms with involvement of the stomach and intestines
In addition, amyloidosis in the digestive tract leads to nausea, gas, constipation and even intestinal obstruction. Affected people lose weight unintentionally because components of the food are no longer adequately utilized. They are often tired and quickly exhausted. Abdominal pain sometimes indicates abnormal liver enlargement.
What does the doctor?
Amyloidosis is a rare disease. Complaints such as tiredness, flatulence, diarrhea, nausea, vomiting, weight loss, joint pain or water retention are quite unspecific - they also occur with many other diseases. This is why doctors often take some time to make the actual diagnosis.
First examinations at the family doctor
In a conversation with the patient, the doctor records possible previous illnesses and listens to breathing, heart, vascular and intestinal noises. A complete blood count and urinalysis are also appropriate. Signs of amyloidosis are high amounts of protein in the urine, diseases of the heart muscle (cardiomyopathies), diseases of the nervous system (neuropathies), cancer of the blood-forming system (multiple myelomas) or an enlarged liver.
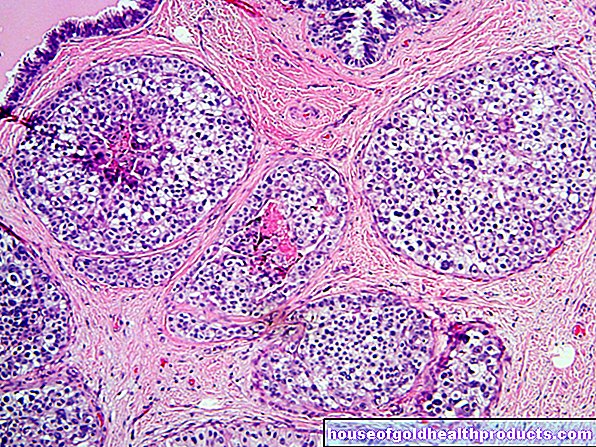
Diagnosis through tissue samples and imaging
To confirm amyloidosis as a diagnosis, specialists use a special needle to remove some subcutaneous fatty tissue from the affected organ. They send this sample to the laboratory for further analysis. There, specialists examine the tissue by staining it with Congo red, a special chemical, and looking at it under a microscope. Such methods are also suitable for detecting the fibrils. Laboratory doctors give certain antibodies to the sample, which only recognize specific proteins.
In contrast, a method from nuclear medicine, SAP scintigraphy, is suitable for finding deposited proteins in AA amyloidosis. Patients receive a weakly radioactive substance (123I-labeled serum amyloid-P). It accumulates in regions of the body where amyloid deposits can already be found. The medical professionals record the radiation with a special device called a gamma detector. In this way it can be determined whether and, if so, which tissue has absorbed the marker.
How is amyloidosis treated?
There is no general treatment for amyloidosis. The therapy is based on the one hand on the subtype of amyloidosis and on the other - if applicable - on the underlying disease. The doctor tries to reduce the concentration of precursor proteins so that less amyloid is deposited. The aim is to enable patients with amyloidosis to live with the highest possible quality of life. There are also experimental therapies that are currently being investigated in clinical studies.
Supportive treatment
Some general medicine therapies have proven effective in amyloidosis. For heart failure, doctors recommend low-salt diet, water medication (diuretics) and special heart medication (ACE inhibitors). If the symptoms are more severe, other drugs, a pacemaker or an implantable cardioverter defibrillator are used. This is a device that helps prevent sudden cardiac death in the case of life-threatening cardiac arrhythmias.
If the kidneys are affected, doctors also recommend low-salt diets, diuretics, and medication to lower high blood lipids, ACE inhibitors, and certain anti-high blood pressure drugs (AT1 antagonists). More severe restrictions in kidney function ultimately lead to dialysis or kidney transplantation. If doctors find amyloid tumors, they will surgically remove them.
Therapy of AL amyloidosis
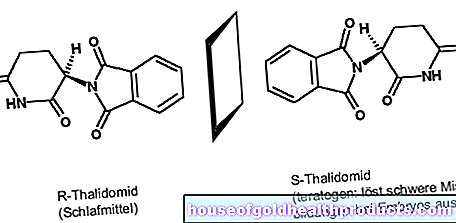
In the case of AL amyloidosis in particular, doctors try to prevent the multiplication of plasma cells. These immune system cells produce large quantities of light chain proteins. The drug of choice is often special chemotherapy (melphalan chemotherapy) followed by an autologous stem cell transplant. The patient receives his own blood stem cells back, which were taken from him before the chemotherapy. If the treatment does not lead to the desired result, there are special chemotherapies as an alternative: the active ingredients thalidomide plus dexamethasone, bortezomib or lenalidomide together with dexamethasone.
Therapy of AA amyloidosis
AA amyloidosis is associated with inflammatory diseases. To reduce the level of serum amyloid A, doctors will always try to find the cause and treat it with appropriate medication. If it is familial Mediterranean fever, an inherited disease with attacks of fever and pain, the active ingredient colchicine is the first choice.
So-called biologics are used for inflammatory rheumatic diseases. These molecules intercept messenger substances in the body and inflammation is reduced. There are numerous other treatment options. If the cause of the amyloidosis is tuberculosis, those affected are given a combination of different antibiotics. The medication usually has to be taken for a long time.
Therapy of AATR amyloidosis
If patients suffer from hereditary AATR amyloidosis, mutations in the genetic make up an altered form of the protein transthyretin - more than 99 percent of which is in the liver. Liver transplants prevent this and prevent AATR amyloidosis.This procedure is carried out at the onset of the illness, if possible, in order to avoid consequential damage.
Prevent
There are no preventive measures against hereditary forms of amyloidosis. To prevent other forms, it is important to treat chronic infections and chronic inflammatory diseases quickly.
Tags: drugs Menstruation home remedies
.jpg)