Rectal cancer
and Martina Feichter, medical editor and biologist and Florian Tiefenböck, doctorDr. med. Mira Seidel is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day.She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts
Florian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian Tiefenböck All content is checked by medical journalists.Rectal cancer (rectal cancer, rectal cancer) is a malignant tumor in the last section of the intestine. It usually develops from initially harmless intestinal polyps. Typical symptoms are blood in the stool or pain when defecating. Read more about the signs, causes, treatment and prognosis of rectal cancer here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C19C20
Brief overview: rectal cancer
- What is rectal cancer? Colon cancer in the last section of the colon
- How do rectal cancer develop? Usually from initially benign intestinal polyps (especially adenomas)
- Frequency: Every year around 25,000 people develop rectal cancer, men slightly more often
- Symptoms: blood in the stool, painful stool, sometimes changes in stool, later pencil stools, involuntary stool and wind leakage, sacrum pain
- Causes: poor diet (little fiber, a lot of meat and fat), lack of exercise, obesity, alcohol, nicotine, genetic factors, inflammatory bowel disease
- Treatment: radiation and surgery for healing, often in combination with chemotherapy; sometimes artificial anus
Rectal cancer: description
In many colon cancer patients, the tumor is located in the rectum or rectum. This is the last section of the intestine before the anus. It is about 15 to 18 centimeters long and plays a crucial role in defecating.
Rectal cancer (rectal cancer, rectal cancer) is almost always a so-called adenocarcinoma. This is a malignant growth that develops from the glandular tissue. Almost half of all colon cancer cases are in the rectum.
Rectal cancer: causes and risk factors
Rectal cancer usually develops from benign growths of the intestinal mucosa, so-called intestinal polyps. Such polyps are found in the intestines of a great many people. Most of the time they remain harmless. But they can also degenerate over the course of years and develop into cancer - a rectal cancer develops.
A cancer tumor grows quickly and uncontrollably. It penetrates the surrounding healthy tissue and destroys it. In addition, individual cancer cells can spread in the body via the blood and lymph vessels and form daughter tumors (metastases) elsewhere, for example in the lymph nodes, lungs or liver.
Genetic predisposition
Sometimes rectal cancer has a family history. This suggests that there is a genetic predisposition to rectal cancer in such families: those affected have an increased risk of developing rectal cancer from benign colon polyps in the rectum.
There are also some hereditary diseases that promote the development of rectal cancer (and other cancerous tumors). These include, for example, Lynch syndrome (hereditary non-polyposis colorectal cancer, HNPCC) and familial adenomatous polyposis (FAP).
Pre-existing illness
Inflammatory bowel disease also increases the risk of rectal cancer (and other malignant colon tumors). This is especially true of ulcerative colitis. According to current knowledge, diabetes mellitus also increases the risk of colon cancer.
Unhealthy lifestyle
An unhealthy lifestyle very often contributes to the development of rectal cancer and colon cancer in general: Little exercise, obesity and an unhealthy diet increase the risk of cancer.
Above all, lots of red meat, processed sausages, high-fat foods and little fiber are considered risk factors for rectal cancer and other forms of colon cancer. The same is true of nicotine and alcohol.
The regular consumption of vegetables and fruit as well as a low-fat, low-meat, high-fiber diet and regular exercise reduce the risk of colon cancer (including rectal cancer)!
age
Another common risk factor for all forms of colon cancer is age: the risk of developing the disease increases with age. The mean age of onset at the time of diagnosis is around 71 years (men) and 75 years (women).
Rectal cancer: symptoms
In the early stages, rectal cancer usually does not cause any symptoms. As the disease progresses, however, signs such as blood in the stool, painful bowel movements and changes in bowel habits (diarrhea and / or constipation) become noticeable.
Not every change in bowel habits is cancer. However, have any persistent abnormalities clarified by a doctor!
General symptoms
Rectal cancer can also trigger general symptoms. Many patients feel less productive and tired. Some patients also report unwanted weight loss or fever.
Anemia
Symptoms of anemia (anemia) also often occur. These include, for example, paleness, reduced resilience and a racing heart. Anemia results from rectal cancer bleeding easily and often.
Pencil chair and intestinal obstruction
Once rectal cancer has progressed, it can narrow the passage through the rectum. Bowel movements then appear as thin as a pencil ("pencil stools"). If the tumor continues to grow, there is a risk of an intestinal obstruction (ileus).
pains
In addition to pain during bowel movements, pain in the lower abdomen or sacrum can also occur. If cancer cells have spread throughout the body (metastasis), daughter tumors cause further symptoms. Liver metastases cause right-sided upper abdominal pain, lung metastases cause coughing and breathing difficulties.
Rectal cancer: examination and diagnosis
If you have noticed abnormal bowel movements, it is best to first contact your family doctor. If necessary, he will refer you to a specialist doctor. This is usually a gastroenterologist, proctologist or visceral surgeon.
Medical history
If you suspect rectal cancer, the doctor will first ask you in detail about your medical history (anamnesis). He can, for example, have the symptoms described in detail, ask about any pre-existing and underlying illnesses and your lifestyle. He also asks if there are already cases of colon cancer in your family (family history).
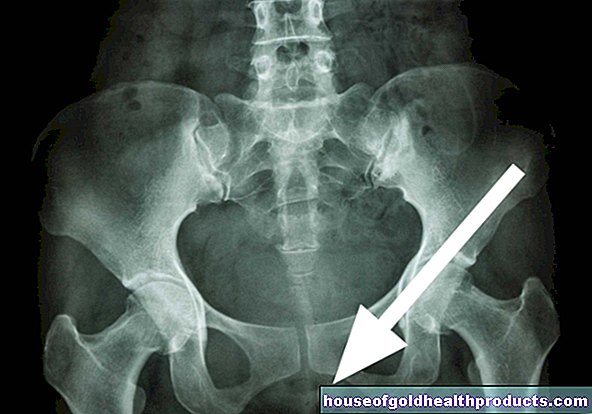
Physical examination
The next step is a physical exam. On the one hand, the doctor can better assess your general condition. On the other hand, he is looking for possible clues about the cancer. This also includes a digital rectal examination: the doctor scans your rectum with a finger over the anus. In some patients, the rectal cancer can be palpated.
Colonoscopy
A colonoscopy will provide more detailed information. It is the best method of diagnosing rectal cancer: the doctor inserts a tube-shaped instrument (endoscope) through the anus. It has a light source and a small camera built into its tip. The doctor recognizes rectal carcinoma even with a "small" colonoscopy (rectoscopy, rectosigmoidoscopy).
With a colonoscopy, the doctor can remove colon polyps directly and take small tissue samples (biopsies) from suspicious areas of the mucous membrane. Pathologists then examine them under a microscope.
Ultrasound of the rectum
For a more detailed examination, the doctor sometimes also performs an ultrasound in the rectum. With this so-called endorectal sonography, the examiner pushes the ultrasound probe over the anus into the rectum like a colonoscopy. In this way, he can better assess the individual intestinal wall layers and neighboring organs.
Staging exams
A detailed examination of the intestine and the analysis of tissue samples taken are sufficient to reliably diagnose rectal cancer. If the suspicion is confirmed, the doctor orders further examinations, the so-called staging. It is used to determine the exact location and size of the tumor and its spread in the body.
Possible examinations for this are, for example, computed tomography (CT), magnetic resonance tomography (magnetic resonance tomography, MRT) and ultrasound examinations of the abdomen. As a rule, doctors use contrast media in order to better differentiate individual tissue structures from cancer foci.
If women suspect rectal cancer has spread to the vagina or uterus, a pelvic examination is necessary.
Rectal cancer: treatment
The exact treatment for rectal cancer is individually tailored to each patient. The tumor stage, age and general condition of the patient as well as any accompanying illnesses play a role.
Classification based on the location
An initial classification is also based on the location of the rectal cancer in the rectum. Doctors divide the rectum into thirds and measure from the anus. This results in rectal carcinoma of the lower (0-6 cm), middle (6-12 cm) and upper third (12-18 cm). Doctors often treat rectal cancer in the upper third like colon cancer.
surgery
The only way to cure rectal cancer at the moment is surgery. The surgeon cuts out the tumor as completely as possible during what is known as a deep anterior rectal resection (TAR).
In the case of larger tumors, the surgeon must remove the surrounding fat and connective tissue (mesorectum) together with the tumor. This procedure is called total mesorectal excision (TME). The doctor also removes the adjacent lymph nodes.
Usually the surgeon creates an artificial anus (anus praeter or stoma). It initially serves to protect the operating theater area (protective stoma) and can be moved back again after a certain period of time. However, if the doctor had to remove parts of the sphincter, the artificial anus may have to remain permanent.
Radiation and chemotherapy
For rectal cancer in the early stages, surgery is usually sufficient treatment. If the tumor is a little further advanced, patients receive radiation therapy or combined radiation and chemotherapy (radiochemotherapy) before the operation.
They can shrink the tumor and sometimes prevent the anal sphincter from having to be removed as well. This neoadjuvant therapy also lowers the risk of relapse. Recurrence of rectal cancer is less common.
Chemotherapy or chemoradiotherapy can also be useful after the operation: any cancer cells that may remain in the body can be killed in this way (adjuvant treatment).
Nowadays, doctors often combine chemotherapy with immunotherapy. Special substances (antibodies) are directed against blood vessel formation (VEGF blockers such as bevacizumab) or the growth of the tumor (EGF inhibitors such as cetuximab).
Treatment of metastases
Sometimes advanced rectal cancer causes metastases to other parts of the body, such as the liver and lungs. If possible, doctors remove these surgically, like rectal cancer itself. If doctors cannot perform an operation, other options are available for liver metastases (lasers, freezing, heat cooked).
You can read more about the treatment in our article on liver metastases.
Palliative treatment
In some cases, rectal cancer is so advanced that doctors can no longer operate on the cancer itself and its metastases. Then doctors try to contain the further spread for as long as possible.
This palliative treatment delays further complaints and ideally increases the quality of the remaining lifetime. Typically, doctors use chemotherapy for this.
Rectal cancer: course and prognosis
The more advanced the rectal cancer, the worse the prognosis: the greater the size and spread of the tumor, the lower the chances of recovery and the higher the risk of relapse. This can be concluded from the survival rates observed: five years after the diagnosis of rectal cancer in stage I, 95 percent of the treated patients are still alive, in stage IV only five percent.
Therefore, use the cancer screening examinations! The earlier the cancer is discovered, the better the prognosis.
In this way, rectal cancer can often be detected early and treated in good time. Also, talk to your loved ones about any malignancies in the family. This enables you to better assess your risk, but also that of your relatives.
You can find out more about this in our article Colon Cancer Prevention.
A healthy lifestyle also lowers the risk of cancer. Adequate exercise, a high-fiber diet and abstaining from nicotine are important first steps.
If you have had rectal cancer, it is important that you go to regular follow-up examinations even after successful treatment has been completed. A possible relapse of rectal cancer can thus be detected and treated at an early stage.
Additional information
You can find more information about colon cancer and colon cancer screening on the Felix Burda Foundation website (www.felix-burda-stiftung.de)
Tags: womenshealth teenager interview