brain death
Updated onClemens Gödel is a freelancer for the medical team.
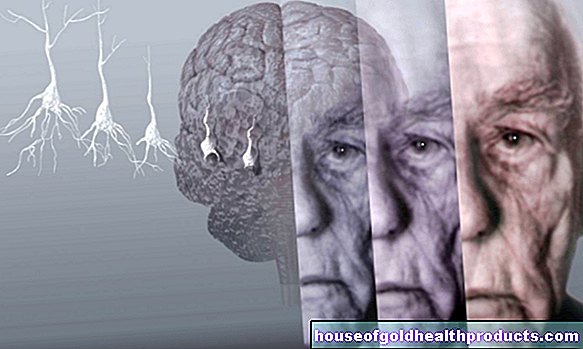
More about the experts All content is checked by medical journalists.The term brain death is used to describe the irreversible failure of crucial areas of the brain. Its determination (brain death diagnosis) is a condition for organ donation that is precisely regulated by the German Medical Association. Only when brain death has been definitively diagnosed is a person considered dead in Germany. Read everything you need to know about brain death here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. G93
Brain death: description
In the second half of the 20th century, medical professionals were confronted for the first time with the fact that they could keep deeply unconscious patients, who no longer had their own respiratory drive, alive with mechanical and medicinal support. The first definition of brain death was published in the late 1950s. It was only later that the organ donation option for the brain dead was added.
The concept of brain death is widespread almost worldwide. According to the Federal Center for Health Education (BZgA), one percent of the around 400,000 dying people in German hospitals suffer from brain death before cardiac arrest each year. In Germany, statistically speaking, only every second brain death diagnosis is related to a planned organ or tissue donation.
How is brain death defined?
The concept of brain death is often confusing and controversial, which makes the issue fearful for many people. An American study showed that only 28 percent of the enlightened relatives of the brain dead could give a correct definition of brain death. The first difficulties arise with the question "What is brain death?" on.
The definition of brain death differs internationally in some details. However, it always says that there is irreversible brain dysfunction. At the same time, however, the spinal cord - also part of the central nervous system - can still function (to a limited extent). The brain-dead person has a measurable pulse and blood pressure in the intensive care unit. The body is still able to keep various body functions in balance. However, this is only possible with intensive machine support.
It is crucial that a brain-dead person cannot breathe spontaneously - a machine must take over the breathing (artificial ventilation), otherwise the heart and circulation will also come to a standstill.
The German Ethics Council agreed that brain death is a sufficient condition for organ removal. However, a minority in the German Ethics Council does not see brain death as a "sufficient condition" for a person's death.
Brain death: symptoms
When a person is brain dead, they can no longer breathe on their own. Indications of brain death are a lack of response to pain (including no grimacing), no respiratory drive and the failure of brain stem reflexes. These reflexes are mediated by the brain stem, an important part of the brain. These include the gag reflex and cough reflex. The loss of eye reflexes can also be an indication of brain death.
Most of the affected patients have low blood pressure and need medication to support the circulation. At the same time, the functions of other organs - apart from the brain - are preserved. Brain-dead people can, for example, have a bowel movement, urinate and sweat. The body can therefore maintain its internal balance (homeostasis) with the help of intensive medical support. Motor reactions, which are usually mediated via the spinal cord, can also occur. This includes the so-called Lazarus sign. These are reflex reactions, mostly from the arms or legs. Twitching of the facial muscles does not fundamentally rule out brain death either. Such signs can be misinterpreted as signs of life and lead to additional psychological stress for relatives.
Brain death: causes and risk factors
Ultimately, an insufficient supply of oxygen to the brain is always the cause of brain death. Even an interruption of the oxygen supply for a few minutes can lead to a failure of the brain, the superordinate control organ of the human body.
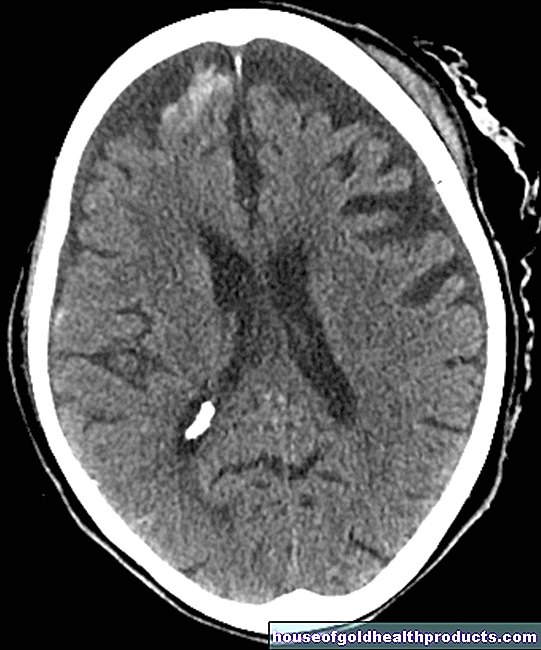
Cerebral haemorrhage is the cause of brain death in over half of all cases. Cerebral haemorrhages are usually the result of a long-standing high blood pressure or a previously damaged blood vessel. Since the bony skull cannot expand, the pressure on the brain increases due to the bleeding, so that the blood circulation in the vessels supplying the brain comes to a standstill.
The second most common cause is so-called ischemic-hypoxic brain damage, which is caused by an insufficient supply of oxygen to the brain (e.g. due to cardiovascular arrest).
Only in third place of the causes of brain death are accidents with traumatic brain injuries. Other causes are cerebral infarction (ischemic stroke), tumors, brain inflammation and the appearance of a water head (hydrocephalus).
Brain death: examinations and diagnosis
In Germany, the diagnosis of brain death is regulated in detail by the German Medical Association in accordance with the Transplantation Act (TPG). Most recently, the relevant guideline in Germany was revised in December 2018. Precise and strict rules are intended to reduce uncertainties among medical staff, but above all fears and worries of relatives.
A precisely regulated process must be followed for brain death diagnostics. If the regulations are followed exactly, brain death diagnostics are considered safe. The aim of the detailed examination is to determine the irreversible failure of the functions of most of the brain, especially the cerebrum, cerebellum and the brain stem. In the guidelines of the German Medical Association, the term "irreversible brain function failure" is used instead of "brain death".
Two qualified doctors must independently determine brain death. The diagnosis of brain death should only be carried out by experienced and specially qualified doctors (intensive care medicine, anesthesia, neurology or neurosurgery). At least one of the doctors should be a neurologist or neurosurgeon with many years of experience in intensive care medicine and brain death diagnostics.
The two doctors may not be involved in any subsequent organ donation and may not accept any instructions from the doctors involved.
The process of determining brain death is precisely regulated by a protocol and takes place in three steps:
1. Are the prerequisites for irreversible brain dysfunction present?
First of all, it must be determined whether there is any sufficiently severe brain damage at all. On the one hand, a distinction is made between whether the brain is affected directly or as a result of other damage (e.g. cardiovascular arrest). In addition, it is investigated where in the brain the damage is located. So-called supra- and infratentorial brain damage is roughly divided:
A connective tissue membrane, the "cerebellar tent" (tentorium cerebelli), is located above the cerebellum. A supratentorial damage lies above this membrane, an infratentorial damage below it. This subdivision is important for the further diagnostic procedure.
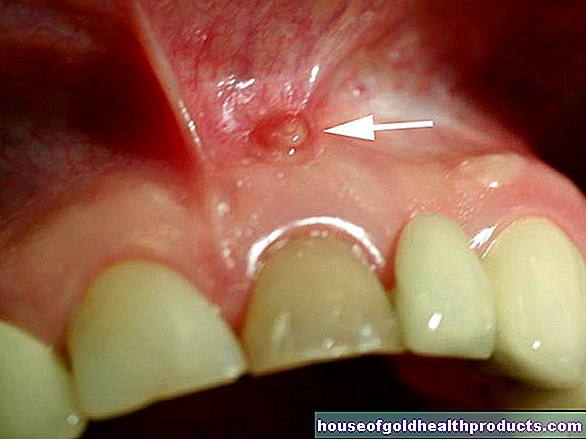
A computed tomography of the brain (cranial CT) helps to identify where the damage is in the brain. This imaging exam can reveal massive damage to the brain. However, shortly after resuscitation or immediately after acute damage, the CT image may still appear normal. It must therefore also be documented when this state of illness began or when the causal accident took place.
Before the detailed brain death diagnosis can be initiated, other causes for the patient's condition must be ruled out. Possible other causes would be, for example, poisoning (also from medication or drugs administered), hypothermia or shock. For this purpose, the pain medication and / or anesthetic medication may have to be discontinued (for a sufficiently long time).
2. Determination of clinical symptoms as criterion for brain death
In the second step of brain death diagnosis, the clinical symptoms are checked according to the brain death protocol:
- State of unconsciousness (coma): The patient must be spoken to loudly and clearly. To do this, intense and repeated pain stimuli must be set. A comatose state exists when all attempts are not followed by a reaction, especially not opening their eyes.
- Light rigidity of both medium to maximally dilated pupils (without dilating medication)
- Absence of the oculo-cephalic or vestibulo-ocular reflex: By turning the head to the side, it is checked whether the eyes can fix a point against the turning movement. This is also known as the doll's head phenomenon (oculo-cephalic reflex). Alternatively, an ear canal can be rinsed with cold water, which, if the reflex is preserved, would lead to eye movement (vestibulo-ocular reflex). If fixation is no longer possible or an ear canal irrigation is achieved, the reflexes are considered to have failed.
- Failure of the corneal reflex in both eyes: In healthy people, touching the cornea (clear skin in front of the pupil) causes the eyelid to close immediately.
- Absence of any pain reactions in the area of the facial nerve (trigeminal nerve) and other regions.
- No cough and gag reflex (pharyngeal / tracheal reflex)
- Complete failure of independent breathing: mechanical ventilation is briefly interrupted for this. This test examines whether and how much the carbon dioxide level in the blood rises as a sign of not breathing.
3. Establishing irreversibility
The third stage of brain death diagnosis is the determination that this state can no longer change. Experienced doctors choose the right means of determining the irreversibility of brain death depending on the case constellation. All procedures have advantages and disadvantages with regard to their diagnostic value. Particularly with the infratentorial brain damage described above, certain conditions must be observed.
In most cases, either a defined observation period of 12 or 72 hours is waited for before a second brain death diagnosis and / or apparatus-based examinations are carried out. The following test results suggest brain death:
- Electroencephalography (EEG) for 30 minutes no deflections from the zero line (isoelectric, repeated)
- Evoked potentials (measurement of electrical voltage differences with targeted stimulation of certain nerve tracts): no electrically measurable reactions to visual stimuli (visual evoked potentials, VEP), acoustic stimuli (acoustic evoked potentials, AEP) and touch (somatosensitive evoked potentials, SEP).
- Determination of the cessation of blood circulation in the brain with angiography, perfusion scintigraphy or Doppler ultrasound
After completing the brain death diagnosis
If the patient is declared brain dead and is eligible for an organ donation, a report is made to the German Organ Donation Foundation (DSO) - the nationwide coordination office for post-mortem organ donation. Important: An organ donation must be expressly approved in Germany - by the donor before his death (e.g. by means of an organ donation card) or afterwards by his relatives. Organ removal is only possible after brain death has been determined.
Organ donation is a difficult but important topic that relatives are often overwhelmed with in this acute situation. The DSO offers them support and guidance.
Special rules apply to children
In children up to the second year of life, especially in premature babies, special regulations apply to the determination of brain death. The examiners must have precise knowledge of the maturation and age-related differences. For example, healthy newborns can also have reduced brain activity. The protocol for brain death diagnostics has been adapted accordingly.
Brain Death: Treatment?
According to the current state of medical research, apart from maintaining critical body functions and the circulatory system in intensive care, no treatment of brain death is possible.
Brain death: course and prognosis
According to current knowledge, recovery from established brain death is not possible. Reports about people who have awakened after a brain death diagnosis have so far been attributed to an incorrect diagnosis. It is extremely rare that a pregnant woman with brain dead was able to carry a child to term while maintaining the intensive care measures. Even with artificial respiration, however, a continuous breakdown of the dead brain matter begins. After about a week, the brain has largely disintegrated.
After the death of a potential organ donor has been determined, organs may be removed subject to approval in accordance with the strict regulations of the Transplantation Act (TPG). When the decision to donate organs has been made, the mechanical and medical support of the circulatory system is maintained until the organ is removed. Otherwise, all (intensive) medical measures will be discontinued after the (brain) death has been determined.
The time of the definitive confirmation of brain death is considered to be the time of death in Germany.
Tags: travel medicine skin magazine





















.jpg)