Subarachnoid hemorrhage
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Subarachnoid hemorrhage (SAB) is bleeding between the middle meninges (arachnoid or spider webs) and the inner meninges (pia mater or soft meninges), which is filled with cerebrospinal fluid (cerebrospinal fluid). Many blood vessels run in this narrow, gap-shaped space around the brain. If a vessel bursts before it dips into the brain tissue, the escaping blood spreads in the subarachnoid space and presses on the brain from outside. However, there is no bleeding in the brain tissue itself. Learn more about the triggers and dangers of subarachnoid hemorrhage here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. I60
Subarachnoid hemorrhage: causes
About five percent of all strokes are caused by spontaneous (non-traumatic) subarachnoid hemorrhage. In Central Europe and the United States, approximately six to nine out of every 100,000 people develop SAB annually. Subarachnoid hemorrhage usually occurs between the ages of 30 and 60, but on average by the age of 50. Women are affected somewhat more often than men.
In about 85 percent of cases, subarachnoid hemorrhage occurs when a so-called aneurysm in the brain ruptures: This is a vascular malformation in the form of a sac-like enlargement of the vascular wall. In the area of this bulge, the vessel wall is less firm than normal and can easily tear - the result is subarachnoid hemorrhage.
The rupture of the aneurysm is not linked to a specific disease, but often happens in full health without previous symptoms, often even in complete calm. In some people, subarachnoid hemorrhage is preceded by physical exertion, such as heavy lifting, difficult bowel movements (heavy pressing), or sexual intercourse. A sudden increase in blood pressure can also cause the aneurysm to burst.
Rare triggers of subarachnoid hemorrhage are, for example, traumatic brain injuries, sinus vein thrombosis (blood clot in a certain brain vessel), vascular inflammation, coagulation disorders, tumors, infections and poisoning (for example with alcohol, cocaine, amphetamines, drugs). Despite an intensive search, no cause at all for the subarachnoid hemorrhage can be found in some of those affected.
Subarachnoid hemorrhage: risk factors
Avoidable risk factors for subarachnoid hemorrhage are high blood pressure, smoking, excessive alcohol consumption and the use of cocaine. Unavoidable risk factors for SAB are, for example, age, a previous SAB, the occurrence of SAB in the family and genetic factors. Past traumatic brain injuries, as a result of which a vascular wall bulge has formed, can also result in subarachnoid hemorrhage.
Subarachnoid hemorrhage: symptoms
The main symptoms of subarachnoid hemorrhage are sudden, violent headaches that have never been experienced before, which quickly spread from the neck or forehead over the entire head and within the following hours also towards the back. This "annihilation headache" is often accompanied by nausea, vomiting, photophobia and stiff neck (meningism). Depending on the extent of the subarachnoid hemorrhage, impaired consciousness up to a deep coma can occur.
In addition, subarachnoid hemorrhage can lead to other symptoms such as rise or fall in blood pressure, fluctuations in body temperature, and changes in pulse and respiratory rate. Depending on the location and extent of the bleeding, symptoms of paralysis and (less often) epileptic seizures can occur.
Five degrees of subarachnoid hemorrhage
Experts in Germany divide the severity of a subarachnoid hemorrhage into five grades (Hunt and Hess classification). These are based on the severity of the symptoms and can be related to the point value in the so-called Glasgow Coma Scale (GCS): In this scale, the patient receives certain reactions (such as opening eyes, reaction to pain stimuli) during the examination at the scene of the accident and verbal utterances) each have a defined number of points. The points are finally added up. The worst value is three, the best 15.
- Hunt and Hess grade I: no or only slight headache, possibly slight stiff neck, GCS value 15.
- Hunt and Hess grade II: moderate to severe headache, stiff neck, no neurological deficits except cranial nerve disorders due to direct pressure of the leaked blood on the cranial nerves, no change in consciousness, GCS value 13-14.
- Hunt and Hess grade III: drowsiness or sleepiness, confusion and / or mild neurological deficits (paralysis, sensory disorders), GCS value 13-14.
- Hunt and Hess grade IV: severe disturbance of consciousness / deepest state of sleep (Sopor), moderate to severe incomplete hemiparesis (hemiparesis), vegetative disorders (such as respiratory disorders or temperature regulation), GCS value 7-12.
- Hunt and Hess grade V: deep coma, no light reaction of the pupils, indications in the neurological examination of an entrapment of the brain due to the excessive pressure in the skull, GCS value 3-6.
Subarachnoid hemorrhage: diagnosis
Subarachnoid hemorrhage manifests itself as a devastating headache and is life-threatening. Therefore, everyone with massive, sudden headaches that they have never experienced before should go to the emergency room of a hospital (if there are no other symptoms) or call the emergency doctor (if there are additional symptoms).
In the hospital, the doctor asks the patient how the symptoms have developed over time. An accompanying person can provide valuable information, especially if the patient is drowsy or unconscious. The doctor also asks about family members with strokes and cerebral haemorrhages, because subarachnoid haemorrhage sometimes occurs in families.
Imaging procedures
When examining the skull using computed tomography (cranial computed tomography, cCT), the doctor usually recognizes the subarachnoid hemorrhage as a flat, white area adjacent to the brain surface. Within the first 24 hours after the bleeding, 95 percent of the subarachnoid hemorrhage can be seen in the cCT, after which the rate drops. Therefore, the cCT is the examination method of first choice in the acute phase after a subarachnoid hemorrhage.
Magnetic resonance imaging (MRI) can also be used to detect subarachnoid hemorrhage in the first few days after the event. If CT or MRI produce an unremarkable finding, a lumbar puncture will help establish the diagnosis. The spinal cord fluid taken during the lumbar puncture can indicate a subarachnoid hemorrhage due to its changed appearance (for example bloody).
Over time, as a reaction to the subarachnoid hemorrhage, convulsions (vasospasms) may develop in the affected blood vessels, which lead to additional paralysis in some people. The vasospasms can be recognized with the help of a special ultrasound examination of the brain vessels (transcranial Doppler sonography, TCD).
To identify the source of the bleeding (aneurysm), the doctor can perform an X-ray vascular imaging (angiography).
Subarachnoid hemorrhage: therapy
People with subarachnoid haemorrhage must be treated to intensive care immediately as the bleeding can be life-threatening. The basic measures of treatment include bed rest and monitoring and, if necessary, adjusting blood pressure and blood sugar. Any fever that occurs is treated.
Surgery to eliminate the aneurysm
If a ruptured aneurysm (pathological vascular bulge) is the cause of the subarachnoid hemorrhage, it is separated from the bloodstream as quickly as possible. This can be done in two ways: either surgically by a neurosurgeon (clipping) or via the blood vessels by an experienced neuroradiologist (endovascular coiling).
When clipping, the surgeon ties the aneurysm at its base with a clamp. This interrupts the supply of blood to the aneurysm. However, surgery can only be performed if there is no cramping of the vessels. Therefore, clipping operations are mainly performed on the first and second day after the first SAB symptoms. If there are vasospasms or if the patient is in poor neurological condition, doctors tend to wait before the operation, as the procedure can worsen the spasm.
When coiling, the doctor inserts a platinum coil ("platinum coil") into the aneurysm. To do this, he pushes a catheter over the inguinal artery to the vascular sac. The coil fills the aneursyma and stops the bleeding. This method is less stressful on the circulatory system and provokes less vascular spasms than clipping. It is therefore recommended if it is not possible to operate with low risk. On the other hand, the aneursyma cannot be switched off quite as effectively by coiling as it is by clipping. Therefore, all patients who have been coiled must be checked after a few months using angiography (visualization of the vessels using an X-ray contrast medium).
Vasospasm
Vascular spasms set in after the fourth day after the subarachnoid hemorrhage and last for about two to three weeks. By impairing the cerebral blood flow and they often cause an appearance or an increase in paralysis or impaired consciousness. Vascular spasms are treated with medication.
"Water head" (hydrocephalus)
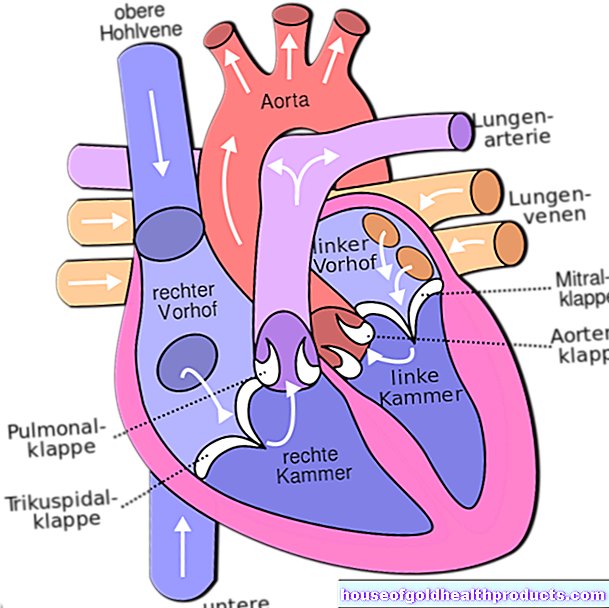
Another possible complication of subarachnoid hemorrhage is the "head of water" (hydrocephalus) - an expansion of the cerebral chambers caused by cerebral fluid that has built up. In some cases, the hydrocephalus resolves spontaneously. Usually, however, the pent-up brain water has to be drained to the outside via a hose for a few days. If a drainage is necessary over a longer period of time, the patient is given a shunt - a surgically inserted catheter that drains excess cerebrospinal fluid either into the abdominal cavity (ventriculoperitoneal shunt) or into the right atrium of the heart (ventriculoatrial shunt).
Subarachnoid hemorrhage: prognosis
The prognosis of subarachnoid hemorrhage depends on many factors, such as the age of the person affected, the severity of the bleeding, and the location of the aneurysm. For example, aneurysms in the back of the brain have a worse prognosis than those in the front of the brain.
In general: Subarachnoid hemorrhage is a life-threatening disease. Overall, around 50 percent of those affected die from SAB. Of the survivors, around half suffer from severe deficits (paralysis, coordination disorders, mental impairment, etc.), while a third remains dependent on outside help for life. Early intensive care treatment of the subarachnoid hemorrhage improves the prognosis.
Tags: hospital home remedies pregnancy




















.jpg)


