Antibiotics: personalized therapy against resistance
Christiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.The situation is threatening: more and more bacteria are becoming resistant to common antibiotics. If the drugs were administered in a more targeted manner, this process could be contained. One possibility for this is a new method with which the administration of antibiotics can be individually adapted to the patient. It is based on a trick that was copied from pathogens.
"Everyone reacts differently to medication - this also applies to antibiotics," says Dr. Can Dincer, microsystem technician at the University of Freiburg im Breisgau in conversation with
The reason for this is, among other things, metabolic processes that take place at different speeds from person to person. That means that one breaks down the active ingredients faster, the other more slowly. Together with biotechnologists led by Prof. Wilfried Weber, Dincer has developed a method that can be used to test whether the amount of antibiotic administered is sufficient to reliably kill the pathogen. If this does not happen, the risk increases that new, resistant germs will form.
Biosensors for antibiotics
To do this, the researchers used a clever trick: they integrated antibiotic sensors into their measuring devices that were originally developed by the pathogens themselves.
In order to defend themselves against antibiotics, bacteria are equipped with special sensor proteins. When an antibiotic attaches to such a protein, it becomes detached from the DNA segment to which it is normally attached. The DNA snippet is then activated and produces proteins that are important for the pathogen's defense mechanisms.
Dosage control by flash test
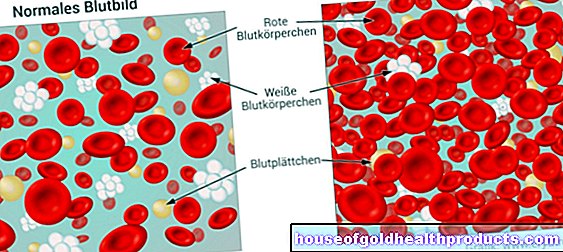
It is precisely this combination of sensor protein and DNA snippets that the researchers use to determine the amount of antibiotics in the blood of patients. If these degrade too quickly, you can add more. In this way, the optimal medication administration can be checked. “This also enables us to avoid underdosing, which would promote the development of resistance,” says Dincer.
The process can be used to prove it within ten minutes - in doctors' offices, during house calls or in pharmacies, but also in environmental and food controls. “It would even be conceivable that the devices, comparable to blood sugar measuring devices, could be operated by the patients themselves,” says Dincer. Up to eight different antibiotic substances can be measured quickly and easily at the same time.
Threatening resistances
The increasing antibiotic resistance is a global problem that experts have been warning about for years. Among other things, they have developed because antibiotics are often prescribed unnecessarily - for example in the case of viral infections, against which they do not help at all. But even if the patient discontinues the medication prematurely because he feels better, surviving germs quickly become resistant.
Antibiotics are also used en masse in animal husbandry - this, too, is a breeding ground for resistant germs, some of which can also spread to humans.
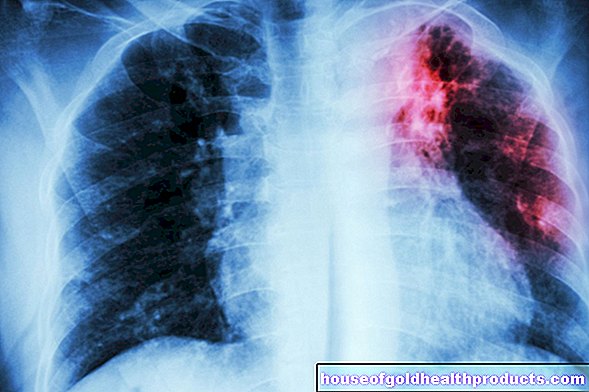
With the spread of resistance, bacterial diseases that had lost their horror since the drug was developed are once again threatening. These include tuberculosis and syphilis, but also common infectious diseases such as wound infections or pneumonia.
Source: André Kling et al ..: Multianalyte antibiotic detection on an electrochemical microfluidic platform, 2016 Anal. Chem., 88, 10036-10043. DOI: 10.1021 / acs.analchem.6b02294
Tags: vaccinations parasites news