tuberculosis
and Christiane Fux, medical editor Updated onFlorian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian TiefenböckChristiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.
Tuberculosis (TB) is a serious infectious disease caused by bacteria. The pathogens are usually transmitted through droplets in the breath that are inhaled. Therefore, in most cases, tuberculosis affects the lungs first. The pathogens can also attack other organs such as the intestines or bones. Read here what exactly tuberculosis is, how you get infected, how you can recognize it and what treatment options are available.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A18A19A17A16A15
Brief overview
- Description: notifiable bacterial infectious disease. Mainly affects the lungs, but also bones, intestines and other organs
- Infection: mostly via droplet infection via the lungs, but also via the digestive tract or skin injuries. Only one in ten infected people develops symptoms.
- Symptoms: fever, cough, night sweats, weight loss, exhaustion, later bloody expectoration
- Particularly at risk: People with a weak immune system, e.g. HIV patients, people who take immunosuppressants, homeless, malnourished, children, addicts
- Diagnostics: antibody test on the skin, blood tests, x-rays, direct detection of bacteria
- Treatment: antibiotics (treatment is difficult if the bacterial strain is resistant)
- Prognosis: Otherwise healthy patients have a good chance of recovery if the disease is detected early.
Tuberculosis: description
Tuberculosis (Tbc, TB) is caused by rod-shaped bacteria called mycobacteria. They mainly affect the lungs, but sometimes other organs as well.
-
"Treat tuberculosis consistently!"
Three questions for
Dr. med. Markus Frühwein,
Specialist in General Medicine -
1
How common is tuberculosis?
Dr. med. Markus Frühwein
A quarter of all people worldwide are infected with the tuberculosis pathogen. However, only about one in ten actually get sick with symptoms. However, an estimated 1.4 million die from it each year. While tuberculosis is common in Eastern Europe, the western industrial nations are little affected. Around 5,500 people fell ill in Germany in 2017. The incidence rate has thus been at a similar level for years.
-
2
Who is particularly at risk?
Dr. med. Markus Frühwein
Since tuberculosis is much more common in other regions, especially in Africa, Southeast Asia and the Western Pacific, people who were born there are particularly affected in Germany. People who have close contact with patients with infectious tuberculosis are also at risk. As well as those infected with HIV and people with a weak immune system. Other risk factors are drug addiction, homelessness and poverty.
-
3
How long does recovery take?
Dr. med. Markus Frühwein
Tuberculosis can be treated with different combinations of drugs. On average, you should expect six months for standard therapy. However, should complications arise, such as resistant bacterial strains, therapy can take significantly longer. Timely treatment and regular use of the medication, even if it is for a longer period of time, is crucial for success.
-
Dr. med. Markus Frühwein,
Specialist in General MedicineDr. med. Markus Frühwein is a specialist in general medicine, tropical medicine, travel medicine and nutritional medicine and owner of the Dr. Frühwein & Partner in Munich.
In most cases, the body succeeds in fighting the pathogens or in encapsulating them to render them harmless at an early stage. Tuberculosis only actually breaks out in around five to ten percent of those infected. Symptoms are fever, fatigue, night sweats and weight loss. Later, there is a bloody cough and shortness of breath, which points to an "open" tuberculosis. "Open" tuberculosis means that the foci of infection in the lungs are not encapsulated, but open to the bronchi.
In the past, tuberculosis was also referred to as consumption because the sick physically degrade very quickly without effective treatment.
Pulmonary tuberculosis
The lungs are most commonly affected by tuberculosis. After infection with the tuberculosis bacteria, a nodular focus of inflammation forms and the lymph glands swell.
Tuberculosis: incidence
Around ten million people are newly diagnosed with tuberculosis around the world every year. In 2019 alone, 1.4 million patients died directly from TB or as a result of the disease.
Tuberculosis has become rare in Germany. Last year the Robert Koch Institute registered 4,127 cases of illness. That is 14.2 percent less than the year before.
Reporting requirement
Doctors must report every patient suffering from tuberculosis and who needs treatment to the responsible health department by name. There is also an obligation to notify patients who suffer from pulmonary tuberculosis requiring treatment but who refuse or discontinue therapy.
Tuberculosis - this is how you get infected
For a long time, tuberculosis was considered to be almost eradicated in the western industrialized countries. In recent years the disease has become more common again due to immigration of sick people, for example from Eastern European countries.
How do the bacteria get into the body?
The transmission of tuberculosis occurs in different ways:
- Breathing air infection: The vast majority of patients become infected because they have been coughed or sneezed on by patients with "open" tuberculosis. The patients expel tiny droplets of secretion that contain bacteria, which healthy people can inhale and then fall ill themselves.
- Infection via the digestive tract: The bacteria can also enter the body via the digestive tract. The causative agent of bovine tuberculosis, Mycobacterium bovis, can be transmitted to humans through raw milk from sick cows, for example.
- Infection through the skin: Another route of transmission is skin injuries. The tuberculosis pathogen can enter the body through them.
How contagious is tuberculosis?
Compared to other infectious diseases such as the flu, TB is not very contagious. The disease actually breaks out in only one in ten infected people. Whether you get sick yourself after contact with an infected person depends primarily on two factors:
- how much pathogen the sick person has secreted
- how powerful your own immune system is
The incubation period for tuberculosis - the time between infection and the outbreak of the disease - can be weeks to months.
Tuberculosis: symptoms
There are different signs of tuberculosis: Depending on the stage of the disease a patient is and which organs have been infected by the bacteria, different symptoms appear.
Latent tuberculosis
In many cases, there are no symptoms of tuberculosis: the person's body manages to keep the bacteria in check so that there are no symptoms. Doctors refer to this as latent tuberculosis.
Closed tuberculosis
In people with good body defenses, the immune cells form a kind of capsule around the foci of inflammation caused by the tuberculosis bacteria. Nodular structures, so-called granulomas or tubercles, develop. The pathogens can still be active in these tubercles, but do not cause any damage in the body. Later on, the tubercles increasingly scarred and calcified. You can often see them on x-rays years later. Doctors refer to this form of progression as closed tuberculosis.
Primary tuberculosis
In around five to ten percent of patients, the body's immune system fails to successfully encapsulate the pathogen. Then foci of inflammation form in the lungs and the nearby lymph nodes, which enlarge. This condition is known as primary tuberculosis. However, the process is slow: this stage usually begins within two years of infection.
Often the sufferers do not notice this form of tuberculosis either. However, various complaints can also occur, such as:
- fever
- cough
- night sweats
- Loss of appetite
- Weight loss
- fatigue
- exhaustion
Open tuberculosis
If the infection spreads in the body, cavities, so-called caverns, form in the lung tissue. They are filled with dead cells and active tuberculosis bacteria (necrosis, cheese formation). If these cavities break through to the bronchi, it is called open tuberculosis.
Then typical tuberculosis symptoms appear: the patient coughs up phlegm, which can also be bloody. The pathogens then often find their way into the air in large numbers.
Patients with open tuberculosis are highly contagious!
Progressive pulmonary tuberculosis
Post-primary tuberculosis
Tuberculosis pathogens can persist in the body for a long time without causing symptoms. However, the disease can break out for the first time or again many years after the initial infection. Then one speaks of post-primary tuberculosis.
In about 80 percent of cases, this affects the lungs. Sometimes the pathogens are also distributed via the bloodstream. The smallest inflammations develop in other organs, so-called "minimal lesions". It usually affects the pleura, lymph nodes, bones and joints. But the digestive tract, skin and genital organs can also be affected.
Tuberculosis outside of the lung tissue
Even if they are mostly located in the lungs - tuberculosis pathogens can also infect organs and tissues in the rest of the body. The symptoms are very different.
Lung root: There are a particularly large number of lymph nodes where the bronchi enter the lungs (lung root, lung hilus). If they are attacked by tuberculosis bacteria, they swell and compress the adjacent airways. The lung tissue behind it is cut off from the air supply and collapses. If the lung area that is no longer ventilated is large, the patient will noticeably suffer from shortness of breath.
Pleura: With tuberculosis of the pleura (pleurisy tuberculosa), those affected usually have pain when breathing. With "wet" pleurisy, fluid collects around the lungs, which can compress the lungs so hard that it causes shortness of breath.
Miliary tuberculosis: Miliary tuberculosis is a TB infection that affects not only the lungs but also the meninges, liver, spleen, kidneys and eyes. In the process, small, granule-sized foci of inflammation are formed, distributed throughout the entire organ. They are reminiscent of millet grains, in Latin milium. This form of TB is rare in Germany. It more often affects children or people with a weakened immune system.
Miliary tuberculosis
The symptoms of tuberculosis in this form of the disease are non-specific. This means that they can also occur in many other diseases and are not typical of tuberculosis. These include fever, headache, a stiff neck and visual disturbances.
Intestinal tuberculosis: Patients contract intestinal tuberculosis mainly through the consumption of infected raw cow's milk. In addition to flu-like symptoms, there are symptoms that are reminiscent of a chronic inflammatory bowel disease: diarrhea, abdominal pain and weight loss. Often there is also blood in the stool. As the disease progresses, peritonitis or a dangerous intestinal obstruction can develop.
Skin tuberculosis: An infection of the skin with tuberculosis pathogens can manifest itself in different ways. Flat, reddish-brown skin changes occur most frequently. These are often hardened and clearly palpable. However, the patient is in no pain. Doctors also speak of this disease picture Lupus vulgaris.
Tuberculosis of the urinary tract: If the urinary tract is infected with tuberculosis, inflamed nodules form in the kidneys, ureters and the bladder, which can scar and calcify. Sufferers experience pain when urinating and in the flanks. You may find blood or pus in the urine. The nodules can also block the urinary tract, causing the urine to build up. The urinary organs can suffer permanent damage as a result.
Tuberculosis of the genital organs: In women, a tuberculosis infection of the genital organs usually migrates from the fallopian tubes into the uterus. Then the menstrual period often stops and the woman can become sterile.
In men, the epididymis can be attacked by tuberculosis bacteria. These then swell painfully and are reddened. The disease can lead to infertility.
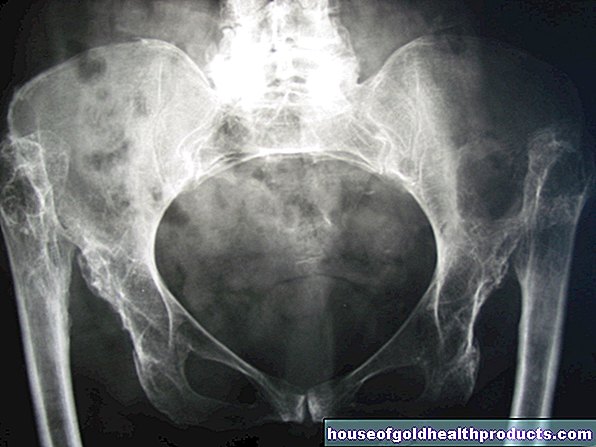
Bone and joint tuberculosis (spondylitis tuberculosa): Bone and joint tuberculosis manifests itself in swelling and pain in the joints, but especially in the thoracic and lumbar spine. The patients feel very sick.
If the inflammatory process of this tuberculosis continues untreated, abscesses form. Nerve failures with symptoms of paralysis occur in the affected areas. Often a hunched back forms. In extreme cases, the spine kinks backwards. However, thanks to good treatment options, these severe TB symptoms have now become very rare.
Tuberculosis: causes and risk factors
With a share of over 95 percent Mycobacterium tuberculosis the most common causative agent of tuberculosis in humans (the rest is attributable to others Myobacterium-Species). The disease mainly breaks out in people with a weakened immune system. This includes:
- HIV-infected, AIDS patients
- chronically ill (e.g. diabetics)
- Patients in whom the immune system is suppressed by drugs (e.g. after a transplant)
- Drug addicts, smokers and alcoholics
- elderly
- Patients with kidney failure
- homeless people
- Malnourished
- Infants and children under four years of age
Migrants from countries with poor health care are comparatively likely to suffer from tuberculosis. The risk of infection is particularly high in the confined spaces of refugee accommodation. TB is also more common among prison inmates than the rest of the population. In both groups, therefore, special attention is paid to the possible spread of TB from the medical side.
Tuberculosis: diagnosis and examination
The signs of TB are not very characteristic (unspecific). About 15 percent of the time, there are no symptoms at all. The infection is therefore usually discovered by chance, for example during a check-up at the family doctor or specialist in internal medicine.
Medical history
Taking the medical history (anamnesis) is the first step in the event of a suspected TB. The doctor asks the patient about any symptoms, for example:
- Do you have a low temperature?
- Do you sweat profusely at night?
- Have you lost a lot of weight lately?
Other circumstances that make tuberculosis more likely and should therefore be discussed in the anamnesis include:
- previous tuberculosis infection (in this case dormant TB bacteria may have been reactivated)
- known TB cases in the immediate vicinity, i.e. among relatives and friends or at work (especially in the medical field)
- Travel to countries with a higher prevalence of tuberculosis
- Previous illnesses or the use of drugs that weaken the immune system and thereby promote tuberculosis infection
Physical examination
Since tuberculosis occurs in the lungs in most cases, the doctor will examine it by listening and tapping it. Signs of consumption can also be found in other parts of the body, such as skin changes or pounding pain over the side ribs or kidneys.
If a doctor suspects a tuberculosis infection based on the medical history and physical examination, a number of other examination options are available for clarification.
Tuberculosis: test method
There are special tests that help diagnose tuberculosis.
Tuberculin skin test (THT)
In the Mendel-Mantoux tuberculin test, the doctor injects a small amount of the pathogen's protein (tuberculin) under the patient's skin. Since the immune system of infected people has usually produced special antibodies against the pathogen after a few weeks, a reddened hardening forms at the puncture site in people infected with tuberculosis.
However, the test does not provide proof for or against an infection. If it occurs too early (less than six weeks) after the infection or if the immune system is weakened, not enough antibodies are (yet) available. The tuberculosis skin test is negative despite the infection. Even in older people or people with weakened immune systems, the tuberculin skin test can be negative despite infection.
IGRA (interferon gamma release assay)
This test examines the patient's blood. If the person is infected with tuberculosis, special immune cells produce interferon gamma, which can be detected during this examination.
The test is more accurate than the skin test. At the moment, however, doctors are primarily using it in addition to the tuberculin skin test (THT), especially in the case of a positive skin test or people with weakened immune systems. If both the skin test and the IGRA test are negative, consumption is very unlikely.
You can read more about the tuberculin skin test and IGRA as well as rapid tests for tuberculosis diagnostics in the article Tuberculosis Test.
Direct pathogen detection
If, for example, shadows appear in the lung tissue in the X-ray image (see below) and the above-mentioned TB tests are positive, the tuberculosis bacteria must be detected directly. Sputum, gastric juice, urine, menstrual blood and cerebral fluid are examined. In some cases, doctors also take tissue samples from the lungs or lymph nodes (biopsies). If tuberculosis pathogens are actually found in the samples, a test is carried out at the same time to determine whether the bacterial strain in question is resistant to certain antibiotics.
The direct pathogen detection is meaningful, but complex and time-consuming. It can take up to twelve weeks to get results.
roentgen
A chest x-ray (chest x-ray) can reveal possible foci of inflammation. In primary tuberculosis, these appear as round shadows. When the hilar lymph nodes are infected, the shadow resembles a chimney. In the case of miliar tuberculosis, on the other hand, the doctor can recognize many small dots.
In addition, if you have tuberculosis, you can see accumulations of fluid on the x-ray, for example if the pleura is affected.
If a fresh tuberculosis infection is suspected and the x-ray is normal, a new image is taken after three months at the earliest. This is how the course of tuberculosis can be assessed.
CT (computed tomography)
If nothing or only a little can be seen on an X-ray, the doctor will order a computed tomography (CT) scan. It delivers much more detailed images than an X-ray machine. In this way, foci of tuberculosis can be detected that are hidden, for example, by the collarbone. CT images are also helpful for inflammation elsewhere in the body (extrapulmonary tuberculosis).
Blood test
Through a comprehensive blood test, the doctor checks values, the change of which speaks for the disease of a certain organ. In addition, certain blood values such as CRP and white blood cells (leukocytes) may be increased, which is a general sign of inflammation in the body.
Tuberculosis: treatment
Active tuberculosis always needs treatment. Speak for an active TB:
- Illness-related cavity (cavern) in the airways
- Focus of inflammation (seen as a shadow in the lungs)
- Enlargement of an old (already known) focus with reactivated TB
- Pathogen detection
Inpatient treatment and quarantine
Particular caution is required with open tuberculosis. The patients are usually admitted to the hospital as an inpatient and isolated. Nursing staff and contact persons wear protective clothing (gloves, gown, nose and mouth protection) when dealing with the patient - this is particularly important in the case of overt tuberculosis. If effective treatment for tuberculosis has been initiated, isolation can usually be lifted after three weeks. Afterwards, the person concerned can also receive further care at home (outpatient).
Medication
Standard drugs for tuberculosis are certain antibiotics. In individual cases, however, the attending physician may also prescribe other medications.
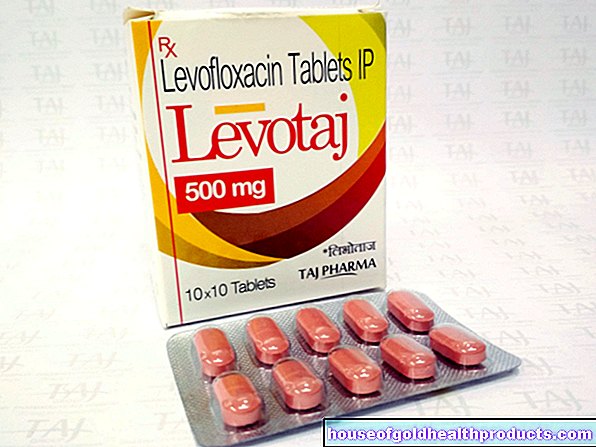
Antibiotics
Tuberculosis is mainly treated with antibiotics, which have proven to be particularly effective in treating the disease. They are called anti-tuberculotics. At the beginning of therapy, four drugs are prescribed simultaneously for the first two months as standard:
- Isoniazid
- Rifampicin
- Pyrazinamide
- Ethambutol
- alternatively: streptomycin
Then two antituberculotics, usually rifampicin and isoniazid, are given for an additional four months. For example, if the patient has a disease such as HIV that weakens the immune system, or if they have relapses, the duration of treatment is extended.
The treatment of complicated tuberculosis can take longer than a year. Since the medication can have side effects, the doctor regularly checks the patient's important blood values and organ functions. He particularly focuses on the liver, kidneys, nerves, ears and eyes. He also pays attention to skin changes.
cortisone
If meninges, pericardium, peritoneum or adrenal glands are inflamed in tuberculosis patients, doctors initially also administer corticosteroids ("cortisone"). They are supposed to curb an excessive inflammatory process.
Cough suppressants
In the case of open pulmonary tuberculosis, the doctor also gives cough suppressant medication. This also protects the environment as the patient spreads fewer pathogens in the air.
surgery
In some cases, drug therapy for tuberculosis is inadequate or does not work at all. This is the case, for example, with very large foci of inflammation. Surgery can also be useful for bacterial strains that are resistant to drugs. Surgeons try to remove the tubercular foci of inflammation.
Accompanying measures
Anyone who suffers from tuberculosis should avoid anything that can worsen the course of the disease. This includes the consumption of alcohol and tobacco products. In addition to tuberculosis, doctors also treat other diseases that may be present that could worsen tuberculosis.
Treatment of latent tuberculosis
Latent tuberculosis is also often treated with antibiotics to prevent it from progressing to active tuberculosis (chemopreventive treatment). This is useful, for example, if the risk that the latent infection will turn into an active one is very high. This is the case, for example, with HIV-infected people and people with a drug-suppressed immune system.
People usually take the antibiotic isoniazid every day for nine months. If there is an isoniazid intolerance or resistance, other antibiotics must be used. For example, rifampicin can alternatively be given for four months.
Measures for contact persons
If a patient is diagnosed with tuberculosis, contact persons are usually immediately isolated. Only when three independent samples of the sputum are free of pathogens will you be released from isolation as a contact person.
After unprotected contact with an infected person, preventive treatment with the antituberculotic drug isoniazid (chemoprophylaxis) can also be useful - especially for young children, because they are particularly susceptible and can also develop severe disease. This chemoprophylaxis usually lasts three to six months if the TB skin tests are negative. If their test result is positive, preventive treatment is given for nine months.
Tuberculosis: disease course and prognosis
If a patient is treated correctly and on time, tuberculosis is usually curable. However, there are some factors that make it difficult to treat tuberculosis.
- Weak patients: If the patient suffers from chronic diseases or has a weakened immune system, the chances of a cure for tuberculosis decrease. In severe cases, lung bleeding, lung collapse or blood poisoning (sepsis) with severe organ damage can occur.
- Galloping consumption: Particularly dangerous is the rapid death of the inflamed areas of the lungs, the so-called "galloping consumption". The lung tissue becomes yellowish and crumbly, which is why experts also call this process cheese formation. If the dead material liquefies (melted), the TB cooker can scatter.
- Resistant pathogens: In Germany, around twelve percent of tuberculosis cases are currently caused by pathogens that are resistant to at least one anti-tuberculosis drug. In about two percent of the cases, the bacteria are even resistant to several drugs (multi-resistance). With such a complicated TB, doctors then have to fall back on reserve funds. Treatment lasts one and a half to two years.
- Lack of therapy compliance: Because of the long duration of treatment and the side effects of some drugs, some patients do not adhere to their therapy plan. For the success of the therapy, however, it is crucial that the patient takes the prescribed medication regularly and permanently. Otherwise the pathogens will not be killed sufficiently and it will be easier for them to develop resistance to the drugs.
Tuberculosis: vaccination
There used to be a vaccination against tuberculosis in Germany with a weakened mycobacteria strain that was injected into the skin. Since 1998, the vaccination has not been recommended by the Standing Vaccination Commission (STIKO) - on the one hand, because the risk of infection in this country is very low, and on the other hand, because the vaccination is only effective to a limited extent and can also cause severe side effects.
In which cases and in which countries the vaccination is still recommended and how the vaccine works can be found in the article Tuberculosis - Vaccination.
Additional information
Guidelines
- Schaberg et al .: S2k guideline of the German Central Committee for Combating Tuberculosis e.V. on behalf of the German Society for Pneumology and Respiratory Medicine e.V .: "Tuberculosis in Adulthood" in: Pneumologie, Zeitschrift für Pneumologie und Ventilationmedizin, Thieme Verlag, 2017; 71: 325-397


.jpg)