Hypogonadism
Astrid Leitner studied veterinary medicine in Vienna. After ten years in veterinary practice and the birth of her daughter, she switched - more by chance - to medical journalism. It quickly became clear that her interest in medical topics and her love of writing were the perfect combination for her. Astrid Leitner lives with daughter, dog and cat in Vienna and Upper Austria.
More about the experts All content is checked by medical journalists.Doctors call hypogonadism a deficiency in sex hormones that occurs in both men and women. In adolescents, the hormone deficiency means that puberty does not begin or begins late. Read here about the causes of hypogonadism, the symptoms and how the disease is treated.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E29

Brief overview
- What is hypogonadism? Deficiency of sex hormones (testosterone, estrogen, progesterone)
- Causes & Risk Factors: Disruption of the gonads (testicles, ovaries) or the hypothalamus / pituitary gland; in some cases genetic predisposition
- Symptoms: Depending on gender and when the hormone deficiency occurs (congenital, before or after puberty)
- Diagnostics: physical appearance, blood test
- Treatment: administration of sex hormones, treatment of the underlying disease
- Prevention: No prevention possible
What is hypogonadism?
Hypogonadism is when the gonads (testicles or ovaries) produce too little or no sex hormones. The term "hypo" comes from Latin and means "under", the gonads are the sex glands.
Both sexes can be affected by hypogonadism. In male hypogonadism the testes do not produce enough androgens (testosterone), in female hypogonadism there is a lack of estrogens and gestagens (progesterone).
As a result of the hormone deficiency, sexual development is disturbed, in adults the secondary sexual characteristics (for example pubic hair) recede and those affected become sterile. The symptoms that appear depend on when the sex hormone deficiency occurs.
Sex hormones in women: The female sex hormones estrogen and progesterone as well as a small amount of the male sex hormone testosterone are mainly produced in the ovaries. The sex hormones in women are necessary for female development, the formation of secondary sexual characteristics such as breast, pubic and armpit hair, for the menstrual cycle and the formation of bones.
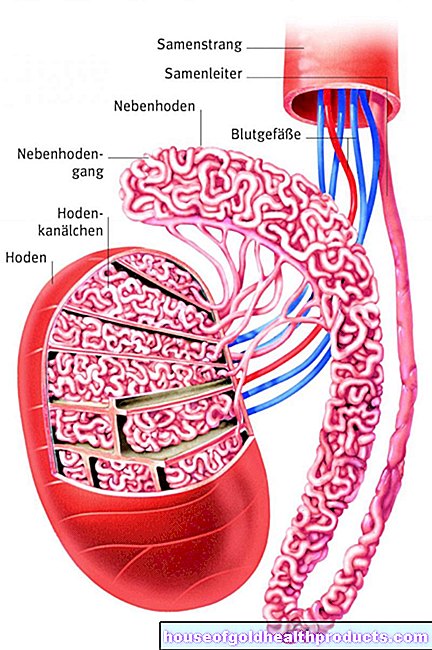
Male sex hormones: Male sex hormones are called androgens, the main one being testosterone. It is mainly formed in the testicles and is necessary for male physical development (e.g. beard growth, pubic hair, growth of the penis and testicles), for sexual function and for reproduction.
Production of sex hormones
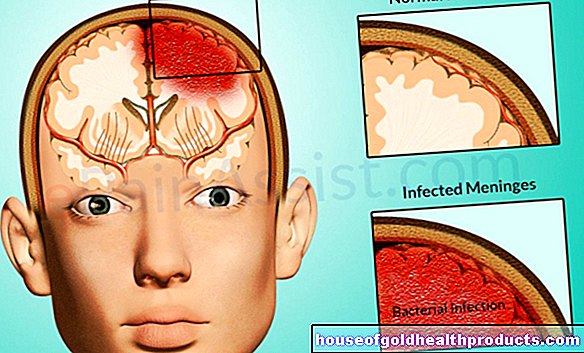
The most important higher-level control center for the production of sex hormones in the gonads is in the brain - in the so-called hypothalamus, an area in the diencephalon. If sex hormones are to be produced, the hypothalamus releases the hormone GnRH (gonadotropin-releasing hormone).
GnRH in turn stimulates the second control center, the pituitary gland, to release the hormones LH (luteinizing hormone) and FSH (follicle-stimulating hormone). These two hormones, also known as gonadotropins, in turn act on the gonads and stimulate them to produce sex hormones. The so-called Leydig cells in the testes then produce testosterone, while the ovaries produce estrogens and progesterone.
If there are enough sex hormones in the body, the hypothalamus and pituitary gland stop the release of GnRH, FSH and LH, so that fewer or no more hormones are produced. Doctors speak of a "negative feedback".
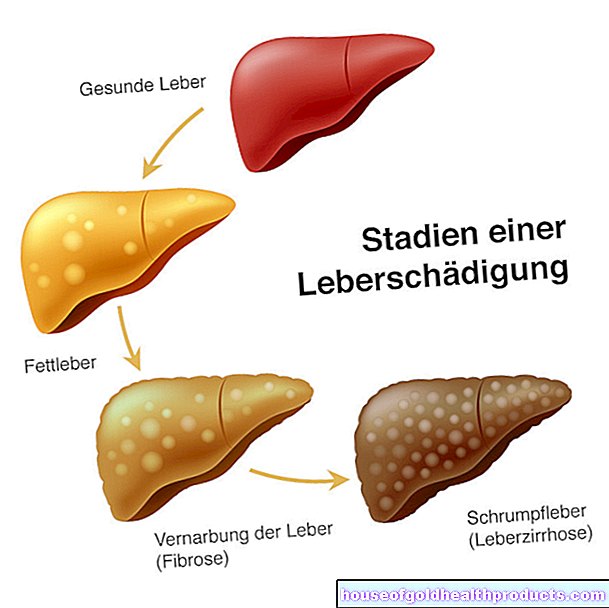
There are several reasons why there are not enough sex hormones in the body. The disruption of hormone production can either be in the gonads themselves or in the control centers in the brain. Depending on the location of the disorder, a distinction is made between primary and secondary hypogonadism.
Primary hypogonadism
In primary hypogonadism, the cause of the hormone deficiency lies directly in the gonads. This is the case when the testicles (for example in Klinefelter syndrome) or the ovaries (for example in Turner syndrome) are missing or inoperable from birth. The same applies if they are removed because of a tumor or damaged as a result of an accident so that they can no longer produce enough sex hormones. Typical of primary hypogonadism is a low level of sex hormone combined with high LH and FSH levels. Doctors also speak of hypergonadotropic hypogonadism.
Secondary hypogonadism
In secondary hypogonadism, the testes or ovaries function as expected. The lack of sex hormones is caused by a malfunction in the hormone control centers of the brain. The causes of the hormone deficiency are either in the pituitary gland or in the hypothalamus. Both the sex hormone levels and the GnRH, LH and FSH values are decreased. Doctors speak of hypogonadotropic or central hypogonadism.
Functional hypogonadism
Functional hypogonadism develops either with age or as a result of another underlying disease. In functional or mixed hypogonadism, both the gonads and the hormonal control centers in the brain can be damaged.
Age hypogonadism (late-onset hypogonadism): The testosterone level in healthy men gradually decreases somewhat with age. Over time, the body loses the ability to properly regulate hormones and less testosterone is made. If the testosterone level is below the normal values for healthy men, one speaks of age hypogonadism. In the 40- to 79-year-old group, up to 12.8 percent of all men have low testosterone levels and symptoms of hypogonadism. However, testosterone production does not usually come to a complete standstill.
In contrast, the female body increasingly ceases to produce sex hormones such as estrogen with the menopause. This results in a natural hypergonadotropic hypogonadism.
Other diseases: Functional hypogonadism also occurs together with other diseases such as metabolic syndrome, obesity, chronic inflammation or depression. Excessive exercise or malnutrition can also trigger symptoms of hypogonadism. It is also possible that certain drugs, such as cortisone, interfere with the production of sex hormones.
causes
Causes of Primary Hypogonadism
There are many reasons for a deficiency in sex hormones. They can either be innate or develop in the course of life.
Congenital hormone deficiency
The most common genetic diseases that lead to a lack of sex hormones are Klinefelter syndrome (in men) and Turner syndrome (in women).
In both diseases, congenital chromosome changes lead to malformations of the gonads, which mean that they do not produce sex hormones. The gender-specific development to be expected does not occur in those affected.
Acquired hormone deficiency
Primary hypogonadism often only sets in over time. There are different causes for the hormone deficiency:
- Inflammation or injury that leads to the destruction of testicular or ovarian tissue
- Tumors of the testes or ovaries
- Surgical removal of testicles or ovaries (for example because of a tumor)
- Viral diseases (especially mumps in men)
- Damage to tissue from radiation or chemotherapy
Causes of Secondary Hypogonadism
In secondary hypogonadism, the gonads are intact and the hormone production is disrupted either in the hypothalamus or in the pituitary gland.
The causes of such damage can be:
- Benign pituitary adenoma (prolactinoma)
- Direct damage to the pituitary gland from traumatic brain injuries, drugs such as phenothiazine or risperidone, chronic kidney failure or hypothyroidism
- Congenital diseases such as Kallmann syndrome
Symptoms
The symptoms of hypogonadism depend not only on gender, but also on when the disease occurs.
How is hypogonadism expressed in men?
Pre-puberty hypogonadism:
- If testosterone is partially or completely absent in childhood, puberty develops delayed, incompletely or not at all (pubertas tarda).
- The primary and secondary sexual characteristics are underdeveloped (small testicles, underdeveloped penis, little body hair)
Post-puberty hypogonadism:
- Decrease in sexual desire, decreased sexual activity
- Erectile dysfunction
- infertility
- Armpit and pubic hair decrease
- Decreased beard growth
- Gynecomastia (enlargement of the mammary gland, female fat distribution)
- Loss of muscle mass and strength
- Decrease in bone density (osteoporosis)
- Increase in blood sugar (diabetes mellitus)
- Hot flashes
- Mood swings
- Exhaustion and aggressiveness
- sleep disorders
- depression
- Decreased mental performance
- Signs of age hypogonadism: sexual dysfunction, obesity, decreased vitality
How is hypogonadism expressed in women?
Pre-puberty hypogonadism:
- If the female sex hormones are already missing in childhood, puberty does not occur (pubertas tarda).
- Girls don't get their periods (primary amenorrhea).
Post-puberty hypogonadism:
- Menstrual cycle disorders
- Missing periods (secondary amenorrhea)
- infertility
- osteoporosis
Delayed puberty
If the first physical changes such as breast development or pubic hair have not yet occurred in girls by the age of 13.5 years, this is referred to as delayed or delayed puberty. The absence of the first menstrual period (menarche) up to the age of 15 also indicates this. Pubertas tarda is also used when it takes more than five years from the first signs of puberty to menarche or when the development of puberty has stopped for more than 18 months.
In boys, one speaks of puberty tarda if at the age of 14 no secondary sexual characteristics (e.g. the beginning of a beard growth and the onset of pubic hair) are visible, puberty lasts longer than five years, or puberty development has stopped for more than 18 months.
Delayed puberty is caused by a lack of sex hormones in both girls and boys. In many cases it is just a harmless familial delay in maturation (constitutional puberty tarda). Malnutrition or diseases such as anorexia are also possible causes.
In addition, there may be primary (girls with Ullrich-Turner syndrome, boys with Klinefelter syndrome) or secondary hypogonadism (Kallmann syndrome).
Pubertas tarda manifests itself through the delayed onset of puberty or through an unusually slow development of puberty. In severe cases there is no puberty at all. In girls, breast growth and menstruation are delayed; in boys, the growth of testicles and penis is delayed.
Pubic and armpit hair growth is delayed in both sexes.
Bone growth also lags behind; those affected are usually smaller than healthy peers. The delayed development of puberty often results in psychological problems.
diagnosis
Contact persons for a possible sex hormone deficiency are the pediatrician, gynecologist or urologist, depending on the age and gender of the patient. An examination by an internist who specializes in hormonal disorders is also possible.
In a detailed discussion, the doctor asks about the existing complaints. This often gives the first indications of hypogonadism. This is followed by a physical exam. The doctor pays particular attention to physical characteristics of the hormone deficiency, such as changes in secondary sexual characteristics.
The doctor also asks whether there are other illnesses such as diabetes or eating disorders and whether the person concerned is taking medication such as cortisone.
If the suspicion of hypogonadism is confirmed, the doctor will carry out a blood test. It determines the levels of sex hormones (testosterone, estrogen, progesterone) and the gonadotropins LH and FSH.
The testosterone determination is usually carried out in the morning between 7:00 a.m. and 11:00 a.m., as the testosterone value is highest at this time. By determining LH and FSH, the doctor differentiates whether it is primary or secondary hypogonadism.
Since general illnesses can also lead to temporary changes in hormone levels, the diagnosis of hypogonadism is only clear when the values are below the normal range in two examinations 30 days apart.
If there is a suspicion of a genetic cause of the hormone deficiency, the doctor will carry out appropriate genetic tests. Structural changes such as tumors on the testicles or ovaries are detected using ultrasound.
treatment
Treatment depends on the cause of the hormone deficiency. If there is an underlying disease such as a tumor, this is treated.
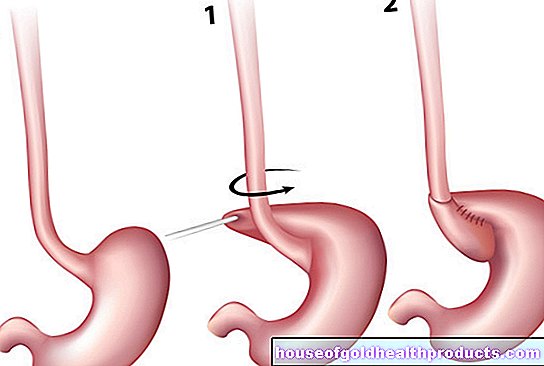
Treatment through hormone replacement
The treatment of hypogonadism in men is testosterone. Various preparations are available for this, which are either injected under the skin (depot injection) or applied as a plaster. For men who want to have children, the doctor prescribes therapy with GnRH, LH or FSH. Testosterone therapy is usually permanent.
The doctor often treats female hypogonadism with estrogen or estrogen-progestagen combination preparations. In this form of hormone replacement therapy, the drugs compensate for the hormone deficiency that occurs during menopause.
Treatment of puberty tarda
In both sexes, the doctor also relies on hormone replacement therapy so that the secondary sexual characteristics develop and puberty sets in. Affected boys are given testosterone. In girls, low-dose estrogen therapy is started; after about a year, additional progestins are administered. Sometimes those affected have to replace the hormones for life in order to prevent side effects of the hormone deficiency such as bone loss (osteoporosis).
forecast
The prognosis depends mainly on the cause of the hormone deficiency. However, hypogonadism can usually be treated well and has no impact on life expectancy.
prevention
There are no special measures to prevent hypogonadism. A healthy lifestyle can help keep hormones in balance. These include a balanced diet, avoidance of nicotine and alcohol, and regular exercise.
Tags: therapies desire to have children anatomy



.jpg)