Anosmia
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Doctors speak of anosmia when someone has lost their sense of smell. Often the loss of smell is only temporary, for example with a cold or sinus infection. Sometimes anosmia has more serious causes and is permanent. Read more about what can cause the odor disorder, why the sense of taste is often impaired and how smell training can help against odor loss.

Brief overview
- What is anosmia? Loss of smell. Like the partial loss of olfactory ability (hyposmia), anosmia is one of the olfactory disorders (dysosmia).
- Frequency: Anosmia affects an estimated five percent of German citizens. The frequency of this olfactory disorder increases with age.
- Causes: e.g. viral respiratory infections such as colds with rhinitis, sinusitis or COVID-19, allergic rhinitis, atrophic rhinitis (a form of chronic runny nose), nasal polyps, curvature of the septum, drugs, pollutants and toxins, Parkinson's disease, Alzheimer's disease, multiple sclerosis, head trauma, brain tumor Etc.
- Diagnosis: Doctor-patient conversation, ENT-medical examination, smell tests, possibly further examinations
- Treatment: depending on the cause, e.g. with medication (such as cortisone), surgery (e.g. for nasal polyps), smell training; Treatment of underlying diseases
Anosmia: causes
Depending on where the cause of the disturbed odor perception is to be found, doctors divide olfactory disorders such as anosmia into sinunasal and non-sinunasal:
Sinunasal olfactory disorder
Sinunasal is an anosmia or other odor disorder if the cause is a disease or change in the nose and / or the paranasal sinuses. The function of the olfactory mucosa in the upper nasal passage is impaired due to inflammation and / or the path of the inhaled air to the olfactory mucosa is more or less blocked.
Most often, inflammatory diseases are the reason for a sinus nasal olfactory disorder, especially chronic inflammation of the nasal mucosa and the paranasal sinuses (chronic rhinitis, chronic sinusitis or a combination of chronic rhinosinusitis). But even with a normal cold or a cold as part of an influenza (flu), most of those affected can smell less (hyposmia) or nothing at all (anosmia) - even if only temporarily.
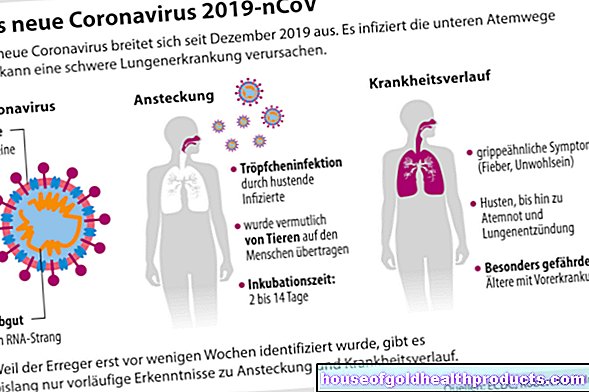
A loss of smell is also typical for the coronavirus infection Covid-19. The anosmia often occurs here as an early symptom. How exactly it comes about is not yet fully understood. Presumably, however, several factors are involved, such as swelling of the nasal mucosa (sinunasal cause), damage to the olfactory mucosa and disruption of the olfactory signaling pathway in the brain (non-sinunasal causes, see below).
Another possible cause of a sinus nasal olfactory disorder is allergic runny nose: If the nasal mucous membrane becomes inflamed and swollen as a result of hay fever or a house dust allergy, those affected can only smell limited or nothing at all.
An olfactory disorder due to a swollen mucous membrane in the nose and sinuses can also occur as a side effect of medication. Various toxins and irritants such as carbon monoxide, ozone or cigarette smoke can also trigger a cold (toxic-irritative rhinitis), which can impair smelling.
In other cases, the anosmia occurs in connection with something called atrophic rhinitis. With this form of chronic runny nose, the mucous membrane becomes thinner and hardened. This often happens in the elderly and those who suffer from granulomatosis with polyangiitis (Wegener's disease). Even after sinus surgery and prolonged bacterial infections of the nasal mucosa, atrophic rhinitis with subsequent anosmia can develop.
Often a loss of smell (anosmia) or a decrease in smell (hyposmia) is also caused by nasal polyps or a strong curvature of the nasal septum (septal deviation). The inhaled air can then hardly or not at all penetrate to the olfactory mucous membrane. In addition, nasal polyps and curvature of the septum can promote sinusitis if they obstruct access to the sinuses. Such inflammatory processes can also affect smell.
The path of the air we breathe to the olfactory epithelium can also be blocked by tumors in the nose or paranasal sinuses.
Non-sinonasal olfactory disorder
Non-sinunasal is the term used for olfactory disorders that are caused by damage to the olfactory system itself (olfactory mucous membrane, olfactory tract).
Very often it is a post-infectious olfactory disorder. This is a persistent olfactory disorder following a temporary infection of the (upper) respiratory tract, with no symptom-free interval between the end of the infection and the noticing of the olfactory disorder. In addition, up to 25 percent of those affected perceive odors changed (parosmia) or report odor hallucinations (phantosmia). Post-infectious olfactory disorders are probably mainly caused by direct damage to the olfactory mucous membrane (olfactory epithelium).
A distinction must be made between post-infectious olfactory disorders and olfactory disorders in the context of a viral infection of the upper respiratory tract (see above). They usually disappear again as soon as the infection has healed.
Other possible causes of a non-sinonasal olfactory disorder are:
- Traumatic brain injury: If you fall or hit the head, olfactory nerves can tear off in whole or in part. Or bruises or bleeding occur in areas of the brain that are responsible for perceiving and processing odor stimuli. The partial or complete loss of the sense of smell (hyposmia or anosmia) occurs suddenly in such traumatic brain injuries.
- Toxins and pollutants: They can acutely and chronically damage the olfactory mucous membrane and thus cause a non-sinus olfactory disorder (for example in the form of anosmia). Possible triggers are formaldehyde, tobacco smoke, pesticide, carbon monoxide, and cocaine. In the same way, radiation therapy can cause a loss of smell (anosmia) or partial loss of smell (hyposmia) in cancer patients.
- Various underlying diseases: In nerve diseases such as Alzheimer's, Parkinson's and multiple sclerosis, the sense of smell can be disturbed or destroyed if nerve cells die in areas of the brain that are important for smelling. In Parkinson's disease, hyposmia or anosmia is even an important early symptom. Other underlying diseases with possible olfactory disorders are epilepsy, schizophrenia, myasthenia gravis, depression, type 2 diabetes, hypothyroidism, liver and kidney diseases.
- Medicines: Some medicines can cause a non-sinonasal olfactory disorder as a side effect. These include antibiotics (e.g. amicacin), methotrexate (used in higher doses as a cancer drug), antihypertensive agents (e.g. nifedipine) and pain relievers (e.g. morphine).
- Operations, infections and tumors inside the skull: Surgical interventions and tumors within the skull as well as infections of the central nervous system can disrupt the olfactory signaling pathway and thus cause a non-sinunasal olfactory disorder.
- Hereditary factors: olfactory disorders such as anosmia can also be congenital. For example, in some people the olfactory bulb (a certain region of the brain) is underdeveloped or completely absent. This is the case with Kallmann syndrome, in which the gonads (testicles or ovaries) are also underdeveloped. More common, however, is the isolated congenital anosmia, i.e. a congenital loss of smell without further symptoms or signs of disease.
- Age: With increasing age, the ability to smell naturally decreases. However, Parkinson's or Alzheimer's should always be considered as a possible cause in older people with a loss of smell.
If no cause for an olfactory disorder can be found, doctors diagnose an "idiopathic olfactory disorder". It is therefore a diagnosis of exclusion.
Anosmia: symptoms
Loss of smell is the central feature of anosmia. Strictly speaking, doctors differentiate between functional and complete anosmia:
- functional anosmia: The sense of smell is so severely restricted that it can no longer be used meaningfully in everyday life - even if a few smells are occasionally, weakly or briefly perceptible. However, this residual olfactory ability is insignificant.
- Complete anosmia: Here the sense of smell is completely gone, which means that no residual olfactory ability can be detected.
Whether functional or complete anosmia - the everyday experience of those affected is simply: "I can no longer smell", so no longer ask your own nose whether the milk is sour, the T-shirt from the day before smells like sweat or the perfume gift from Partner is a direct hit or a flop.
In addition, many people with anosmia have problems with their sense of taste: Most of them can taste salty, sour, sweet and bitter normally, but cannot distinguish between certain aromas. This not only requires the taste receptors, but also the odor receptors on the tongue - an aroma only unfolds in its entirety when they work together.
Anosmia: Consequences
As indicated above, anosmia can significantly reduce the quality of life. Loss of smell and the inability to distinguish between different flavors can reduce the enjoyment of eating and drinking. Even the familiar smell of your own partner or child, the smell of lilac, the clean smell of fresh laundry - all deleted from your own everyday experience.
With the loss of smell, not only the enriching function of smelling is lost, but also its warning function: For example, people with anosmia cannot smell if the food is burning on the stove, food is spoiled or the gas heater has a leak.
Likewise, those affected cannot notice if they smell sweat themselves or smell it in the bathroom or kitchen. The knowledge that other people, in contrast to themselves, can very well notice this, can put anosmia sufferers under great psychological stress.
Anosmia: Therapy
Whether and how a disturbed sense of smell can be restored depends on its cause.
A temporary odor disorder in acute rhinitis (acute rhinitis) and / or acute sinusitis (acute sinusitis) - the combination of both is called acute rhinosinusitis - does not require any special therapy. General treatment measures such as drinking a lot and inhaling are usually sufficient.
Chronic rhinosinusitis without nasal polyps in adults is treated with local cortisone preparations (spray) and saltwater nasal rinses. The cortisone has an anti-inflammatory effect; nasal irrigation helps loosen stuck mucus. If bacteria are involved, the doctor sometimes prescribes antibiotics.
It is best to use the cortisone spray "overhead". If you inject the spray into both nostrils in an upright position, only a small amount of the active ingredient reaches its destination. When used upside down, however, more cortisone reaches the olfactory mucosa in the nasal cavity.
If the hyposmia or anosmia is due to chronic rhinosinusitis with nasal polyps, cortisone preparations are usually used in adults - locally (as a spray) and systemically (as tablets or capsules). Some smaller studies also attribute a certain effectiveness to so-called leukotriene receptor antagonists (such as montelukast). These drugs improve airway permeability and were originally developed for asthma patients. But they can also be taken against olfactory disorders in chronic rhinosinusitis with nasal polyps.
Nasal polyps themselves are very often surgically removed. This improves nasal breathing and - if the polyps have blocked the entrance to the sinuses - the risk of repeated sinus infections. Both can improve a disturbed sense of smell. If you have a tumor in your nose or sinuses that blocks the air you breathe from reaching the olfactory epithelium, you will also usually have an operation. The same is true if a crooked nasal septum obstructing the flow of air causes hyposmia or anosmia.
If an olfactory disorder is based on an allergic runny nose, local cortisone preparations are the most promising therapeutic option. Regardless of whether and how severely the affected person's sense of smell is impaired, the allergy can be treated as required (e.g. avoid allergens as much as possible, possibly hyposensitization).
If a runny nose caused by toxins and irritants (toxic-irritative rhinitis) leads to an impairment of smell or a loss of smell, it is important to avoid the triggering substances as far as possible.
There are no general therapeutic guidelines for anosmia or other olfactory disorder caused by other forms of cold (such as cold of unknown cause = idiopathic rhinitis). Instead, individual treatment attempts are recommended in such cases.
If medication triggers the loss of smell, the attending physician can check whether the preparation can be discontinued. Then the olfactory disorder usually also disappears. If discontinuation is not possible, the dosage can sometimes be reduced. That can at least improve the smell.
Under no circumstances should you discontinue prescribed medication on your own or reduce the dosage! Always discuss this with your doctor first.
Smell disorders as a result of head trauma can be tried to be treated with zinc gluconate - alone or in combination with systemic cortisone preparations (such as cortisone tablets). Alternatively or in addition, patients can take part in structured smell training (see below). In any case, it is important to start treatment as soon as possible after the injury.
Structured olfactory training is also recommended for patients with post-infectious olfactory disorders. If possible, training should be started within the first year after the onset of the olfactory disorder. If necessary, drug treatment can (additionally) be attempted, for example with cortisone.
If underlying diseases such as Alzheimer's disease, multiple sclerosis or brain tumors are behind the (partial) loss of the sense of smell, their specialist treatment is in the foreground.
Treatment is not possible for congenital and age-related anosmia.
Smell training
As mentioned, experts recommend structured olfactory training, especially for post-infectious olfactory disorders. This can also be useful for olfactory disorders after a traumatic brain injury.
The exact structure of the training can vary and will be discussed with the patient on a case-by-case basis. For example, the patient can sniff so-called smell training pens twice a day for several weeks, each of which contains a specific fragrance (e.g. lemon, clove, rose, eucalyptus). This targeted training of the sense of smell can be supported by linking every smell with pictures or words. While sniffing the lemon pen, you can, for example, look at the picture of a lemon and / or pronounce the word lemon in your mind or out loud. This way, the smell impression is better memorized.
Smell training pens are used in a similar way to diagnose olfactory disorders (see below). As an alternative to such pens, some people use vials of pure essential oils for smelling training.
You can also use your memory to train your sense of smell. For example, try to remember exactly the scent of freshly baked cinnamon stars or freshly ground coffee. Or think about what the air smells like when a heavy downpour breaks out on a hot summer's day.
Tips for everyday life
- Smoke alarms in your own four walls are always important - but especially if you suffer from anosmia and are therefore unable to detect any burning smell early on.
- If you are cooking or heating with gas, you should be extra careful and keep the pipes in good condition. If necessary, install a gas detector.
- Do you still have at least part of your olfactory ability? Then the food can be tastier and more enjoyable if you add concentrated flavorings to the food.
- Store your groceries properly. If necessary, make a note of the date of purchase and the date it was opened (e.g. for cans or milk cartons). Use the food within the recommended time. Also remember: In addition to smell and taste, the consistency and color of some foods can also indicate spoilage.
- Some people with anosmia stick to fixed schedules for personal hygiene, changing linen, and cleaning the bathroom and kitchen. Your own nose cannot indicate when it is time for such activities. The fixed plans give those affected security in terms of their own cleanliness and that of their home - often a great psychological relief.
Anosmia: examinations & diagnosis
anamnese
In order to clarify a olfactory disorder, the doctor will first take your medical history (anamnesis). To do this, he asks about your symptoms and possible causes of an odor disorder. Possible questions are, for example:
- How long have you been unable to smell anything?
- Did you suddenly lose your sense of smell or did the olfactory disorder develop slowly?
- Is the odor loss complete or can you still perceive individual, faint smells?
- Do you have any other symptoms, such as problems with taste?
- Do you have an upper respiratory infection that may be related to the olfactory disorder?
- Did you have a head injury or surgery before you lost your sense of smell?
- Do you suffer from previous illnesses, such as chronic sinusitis or an allergy?
- Are you taking any medication, and if so, what are they?
- Are you exposed to chemicals or vapors in everyday life (e.g. at work)?
Physical examination
The anamnesis is followed by an ENT examination, including a nasoscopy (rhinoscopy). When carefully examining the nose, nasopharynx, paranasal sinuses and olfactory fissures (the region in the upper nasal passage where the olfactory mucosa is located), the doctor pays attention to signs of swelling, inflammation as well as nasal polyps and discharge.
He may also ask you to breathe through each nostril in turn while holding the other with your hand. In this way it can be seen whether the air flow is being obstructed on one side.
Smell test method
There are various subjective and objective (apparatus) methods with which the olfactory ability can be tested. The patient must actively participate in the subjective process. Small children and dementia patients are generally unable to do this. Objective testing is therefore more useful for clarifying an olfactory disorder.
Here are some test procedures in detail:
Sniffin 'sticks
"Sniffin" sticks "are felt-tip pens filled with a fragrance. They are the preferred test method for clarifying olfactory disorders because they are easy to carry out and various test variants are possible.
For example, an identification test can be carried out with the olfactory pens. This tests the patient's ability to recognize and differentiate between different scents. To do this, the doctor holds 12 or 16 different "sniffin" sticks "one after the other under both nostrils. The patient should try to identify the respective fragrance with the aid of a selection card on which all fragrances are indicated.
A threshold test can also be carried out using "Sniffin" Sticks, which provides information about the patient's olfactory threshold the patient can just barely perceive.
UPSIT
UPSIT stands for University of Pennsylvania Smell Identification Test. In this process, 40 different fragrances, packaged in microcapsules, are applied to paper. As soon as you rub a capsule with a pen, the respective scent is released. Have the patient try to identify him using a list of four terms.
CCCRC
The test of the Connecticut Chemosensory Clinical Research Center (CCCRC) combines an identification test and a threshold test: In the identification test, the patient has to recognize and name ten different fragrances that are presented to him in glass or plastic vials. In addition, the olfactory threshold is tested with differently concentrated butanol solutions.
Measurement of the olfactory potential
While all previously mentioned test procedures are subjective, the measurement of the olfactory potential provides objective test results - the patient does not need to cooperate. Tiny electrodes are first attached to the olfactory mucous membrane. They measure the electrical potentials that arise in the olfactory sensory cells when scent molecules dock and are then passed on to the olfactory center in the brain via nerve tracts.
As test substances, the doctor holds various pure fragrances in front of the patient's nose one after the other, for example rose scent (chemical: phenylethyl alcohol). It usually only triggers a weak excitation of the olfactory nerves. In contrast to hydrogen sulfide, for example, with its intense odor of rotten eggs.
The measurement of the olfactory potential is very complex. That is why it is only carried out in specialized clinics and doctor's offices.
Other investigations
In certain cases, further examinations may be indicated. For example, if a brain tumor is suspected to be causing the anosmia, computed tomography (CT) or magnetic resonance imaging (MRI) of the skull can clarify the situation. If the doctor suspects Alzheimer's dementia behind the loss of smell, CT or MRI can be used to find out whether brain matter has actually already been lost.
Anosmia: course & prognosis
Basically: olfactory disorders such as anosmia are not easy to treat, and the olfactory ability cannot always be normalized again. The chances of success are generally better in younger patients and non-smokers than in the elderly and smokers. Exact forecasts are not possible, only general information:
Anosmia or hyposmia in the context of an acute viral infection of the (upper) respiratory tract such as inflammation of the nasal mucous membrane (runny nose) or sinus infection is usually not a cause for concern. The olfactory disorder is usually temporary and gets better after the infection has healed. In the case of long-term inflammation, however, the sense of smell can be permanently restricted or completely lost because the olfactory epithelium is progressively destroyed or remodeled.
If the sense of smell is gone or impaired because the flow of breathing air is obstructed by a curvature of the septum, polyps or tumors in the nose or sinuses, an operation can solve the problem - but not always. Some patients may not smell the way they used to, even after the procedure. At least the operation can reduce the olfactory disorder somewhat.
If drugs, toxins or pollutants are the trigger of an olfactory disorder, the olfactory ability can improve again after discontinuation of these substances (e.g. after completion of chemotherapy). However, irreversible damage with a permanent olfactory disorder is also possible, for example when acids have destroyed the basal layer of the olfactory epithelium.
In about two thirds of all patients with post-infectious olfactory disorders, the sense of smell improves spontaneously within one to two years. For the rest of the population, the limited olfactory ability or loss of smell remains permanent. In general, the following applies: the younger a patient is and the shorter the duration of the disorder, the higher the chances of improvement.
Anosmia or other olfactory disorder resulting from a skull injury is less likely. Only in about one to two out of ten patients does the olfactory ability partially return. The probability of an improvement in the first year is highest. However, even years after the injury, patients can spontaneously regain their sense of smell; however, that rarely happens. Among other things, the following are favorable for the prognosis:
- high residual olfactory ability
- female gender
- youthful age
- Non-smoker
- no side differences in the olfactory function
- Smell disorder has not been around for that long
In the case of olfactory disorders in the context of underlying diseases such as Parkinson's, Alzheimer's or diabetes, it cannot be predicted whether and to what extent the olfactory ability will improve again through treatment of the underlying disease.
The natural age-related decline in the sense of smell can neither be stopped nor remedied. Nothing can be done about a congenital anosmia either.
Tags: skin care Diseases magazine







.jpg)