Tuberculosis test
Updated onFlorian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian Tiefenböck All content is checked by medical journalists.The Mendel-Mantoux tuberculosis test is an important part of tuberculosis diagnosis. There has also been a rapid tuberculosis test since 2010. However, a test alone is not enough to reliably diagnose the disease. The patient's medical history and various examinations are also decisive. Read more about the tuberculosis test here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A18A19A17A16A15

Tuberculin skin test (THT)
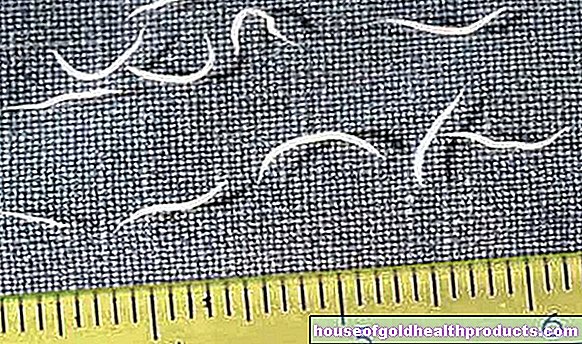
In the Mendel-Mantoux tuberculin test, a small amount of the pathogen's protein (tuberculin) is injected into the skin on the inside of the forearm. A result can be read after three days at the latest: a hardening (with reddening of the skin) has formed at the puncture site. Depending on the transverse diameter of the induration (not the reddening!) And the patient's individual factors, this tuberculosis test is rated as positive or negative:
- Hardening ≥ 5 mm: If the hardening is at least five millimeters in diameter, the test is considered positive in people with a conspicuous X-ray image (shadows, fluid accumulation), immunodeficiency or HIV infection. This parameter is also considered a positive result for people who have or have had close contact with tuberculosis patients.
- Hardening ≥ 10 mm: In the elderly, homeless, drug addicts, diabetics, people with kidney weakness or similar pre-existing diseases, the test is positive if the hardening is at least ten millimeters in diameter. The same applies to people who come from countries with a particularly high number of people infected with TB.
- Hardening ≥ 15 mm: Hardening with a diameter of at least 15 millimeters indicates a fresh tuberculosis infection that must be treated (in people without a special risk). However, it takes an average of eight weeks for the tuberculosis test to work after an infection.
The tuberculin skin test also shows a positive result in vaccinated persons within five to ten years after being vaccinated against TB. This vaccination has not been recommended in Germany since 1998, but it can play a role in young people with a migration background. But even with them, a hardening of more than 15 millimeters in diameter signals a tuberculosis infection.
Negative test result: tuberculosis cannot be excluded with certainty
If injecting tuberculin does not cause skin changes, the test for tuberculosis is negative. But even then, the doctor cannot safely rule out tuberculosis. Because in the first eight weeks after a TB infection, the test may still be negative if the infected person has not produced any antibodies by then. In addition, even with severe courses (such as miliary tuberculosis), the test result is false negative in about half of the cases. Such false negative tuberculosis tests also occur despite an infection in:
- congenital or acquired immune deficiency such as AIDS
- Treatment with drugs that suppress the immune system (immunosuppression)
- Malignant tumors of the lymphatic system (Hodgkin's disease, non-Hodgkin's lymphoma)
- Sarcoid (a disease of the organic connective tissue)
- virus infections such as rubella, measles, chickenpox, flu
- Live vaccinations (for chickenpox, measles, mumps, rubella, yellow fever) for about six weeks afterwards
- very old age
If the doctor suspects a false negative result, the German Central Committee for Combating Tuberculosis recommends performing an interferon gamma test (IGRA).
Interferon gamma test
The Interferon-Gamma-Test (English Interferon-Gamma-Release-Assay, IGRA) is a blood test for the diagnosis of tuberculosis. Synthetic proteins, which are similar to those of tuberculosis bacteria, are added to a patient's blood sample. If the patient actually has tuberculosis, certain immune cells in his blood (T lymphocytes) increasingly release the messenger substance interferon gamma in response to the added foreign proteins. This can then be proven.
Compared to the tuberculin skin test, the IGRA has a higher specificity, which means that it is more likely to detect patients who do not suffer from tuberculosis - so it provides fewer false-positive results. For example, the interferon gamma test - in contrast to the tuberculin skin test - does not give false positive results in people who have recently been vaccinated against tuberculosis. In addition, it gives a result earlier with fresh infections (with the tuberculin skin test, as mentioned above, it takes about eight weeks). However, the interferon gamma test is relatively expensive.
Rapid tuberculosis test
Rapid tests for tuberculosis diagnosis have been developed in recent years. The aim of the research on faster test procedures was and still is to be able to initiate the correct treatment as early as possible.
Xpert MTB / RIF
In this tuberculosis test, the sputum of patients is examined for genetic material of the pathogen Mycobacterium tuberculosis. The so-called polymerase chain reaction (PCR) is used: Individual snippets of eruption from the sample can be reproduced and ultimately determined.
At the same time, the Xpert MTB / RIF rapid test is used to determine whether the tuberculosis strain found is resistant to the antibiotic rifampicin. For this purpose, pathogen genes in which the ability to resist rifampicin is stored are searched for.
The specialty of this tuberculosis test is its simplicity and speed. The results are available after about two hours. The test is recommended by the WHO and scientists hope that this method will replace time-consuming bacteriological tests. In these, the pathogens have to be grown on special nutrient media, which is time-consuming - it can take up to three months until a result is available.
A further development of this rapid tuberculosis test (Xpert Ultra) is also recommended by the WHO - as is another rapid test called the Truenat Assay.
Point of criticism
In 2010, the rapid tuberculosis test achieved very good results in a study. The World Health Organization then decided at the end of 2011 to invest almost 26 million euros in this tuberculosis test by 2015. This should improve the diagnosis of tuberculosis in African and Asian countries and reduce the incidence of the disease.
However, a study from Africa published in 2013 showed that the test had little effect on the incidence of TB. Affected people are treated more quickly, but based on experience, doctors began treatment early on, even without this rapid test. The actual benefit of this rapid tuberculosis test, especially with regard to possible rifampicin resistance, is now being examined in further studies.
Rapid antibody tests
In the past few years, several over-the-counter tuberculosis tests have come onto the market that are supposed to detect a tuberculosis infection even faster. To do this, a small amount of blood is tested for antibodies to tuberculosis. Antibodies are proteins of the immune system and are formed when the attacker is infected.
In these rapid tests, a patient's blood is dripped onto a cassette with a thin paper (membrane). On this there are other proteins that bind to tuberculosis antibodies. If such antibodies are found in the blood of the person being examined, two colored stripes usually appear on the paper after about 15 minutes. This means that the test is usually positive (depending on how it is carried out).
Criticisms
Manufacturers as well as experts (e.g. from the German Central Committee for Combating Tuberculosis), however, point out the limited usefulness of these tuberculosis tests. Only in the case of an active tuberculosis infection can one corroborate the suspicion. Particularly low-bacteria TB diseases are not recognized.
In addition, rapid antibody tests in patients who are receiving antibiotics (for other reasons) can produce false negative results. In addition, they are usually restricted to one or a few types of tuberculosis pathogen. As a result, these tuberculosis tests give false negative results for infections with other mycobacteria. A negative test result of a rapid antibody test does not rule out tuberculosis.
Conclusion
If an infection is suspected, experts continue to recommend known methods of clinical tuberculosis diagnosis, such as the tuberculin skin test, direct detection of bacteria or the interferon gamma test. They still see no benefit in routinely using one of the rapid tuberculosis tests.
Tags: smoking alternative medicine travel medicine