Myelodysplastic Syndrome
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.The term myelodysplastic syndrome (MDS) covers a group of diseases in which the formation of different types of blood cells is disturbed. Possible symptoms of the disturbed blood balance are anemia, a slight tendency to bleed or an increased susceptibility to infections. The causes of MDS usually remain unexplained. Myelodysplastic syndrome usually only occurs at an advanced age, usually from the age of 60. Here you can read everything you need to know about myelodysplastic syndrome.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D46

Myelodysplastic Syndrome: Description
A myelodysplastic syndrome (MDS, myelodysplasia) comprises a group of diseases that affect the bone marrow and thus blood formation. Normally, different types of blood cells develop in the bone marrow from immature bone marrow cells (blasts), which are responsible for different tasks in the body. These include:
- Red blood cells (erythrocytes): oxygen transport
- White blood cells (leukocytes): part of the immune system
- Platelets (thrombocytes): blood clots
Myelodysplastic syndrome affects several of these cell lines. They are either less educated or their function is limited. It differs which cell types and how severely they are affected. If two of the three rows of cells are affected, it is called bicytopenia, if all three are affected, it is called pancytopenia. That is also the reason why there is no such thing as "the" myelodysplastic syndrome. The term describes a group of different diseases, each of which affects blood formation. In most cases, less functional cells of the affected cell type can be found (cytopenia). The bone marrow, on the other hand, is often interspersed with many immature cells (blasts), the precursor cells of blood cells.
Myelodysplasia is most common in people around the age of 70. Every year around four to five in 100,000 people develop MDS. Myelodysplastic syndrome is one of the most common malignant diseases of the blood. In the over 70s, 20 to 50 out of 100,000 people fall ill. Somewhat more men (56 percent) than women (44 percent) develop a myelodysplastic syndrome. Life expectancy and the course of the disease are determined by various factors. Among other things, the decisive factors are how high the so-called blast fraction is, whether there are complex genetic changes and how severely the blood formation is impaired. A high proportion of blasts indicates a high level of disease activity and thus a less favorable prognosis. Age and previous illnesses also play a role. Overall, the mean survival time for MDS is around 30 months. In individual cases, however, large deviations from this statistical mean value are also possible.
Myelodysplastic Syndrome: Symptoms
Myelodysplastic syndrome causes symptoms in around 80 percent of patients due to the reduced number of certain blood cells, while MDS is discovered by chance in the rest. The disturbed formation of the different cells of the blood has various consequences:
Anemia: production or function of red blood cells is impaired
Anemia occurs in 70 percent of MDS cases, making it the most common symptom of myelodysplasia. In MDS, the normal formation of red blood cells and hemoglobin is disturbed, which causes anemia. Hemoglobin is the red dye in red platelets that helps them move gases. If there is too little of it, there may be signs of a lack of oxygen. Patients feel chronically tired, less efficient and have less ability to concentrate. If you exercise even little, you will be short of breath and feel a rapid pulse (tachycardia). Often those affected are noticeably pale and complain of dizziness when exerting themselves. At the time of diagnosis, about half of the patients have such anemia that a blood transfusion is necessary.
Infections: The formation or function of white blood cells is impaired
A myelodysplastic syndrome leads to repeated infections in around 35 percent of cases. Those affected have a low number of white blood cells (leukopenia). If the number of white blood cells is low, the immune system can no longer respond adequately to pathogens. MDS is therefore often associated with increased infections, some of which are accompanied by fever.
Bleeding tendency: the formation or function of the blood platelets is impaired
If the number of blood platelets is reduced (thrombocytopenia), bleeding may occur more quickly. When injured, the platelets usually help the blood to clot and stop the flow of blood. As a result, about twenty percent of people who have myelodysplastic syndrome bleed easily. This can be seen, for example, in small punctiform hemorrhages under the skin, so-called petechiae.
More symptoms
However, there are symptoms that are not directly related to the reduced number of cells in the individual blood cells. In 20 to 50 percent of cases, for example, the spleen is enlarged (splenomegaly). Their function is, among other things, to sort out defective and obsolete red blood cells. If the number of non-functional red blood cells in myelodysplasia is increased, the spleen must also increase its workload. This becomes visible through an enlargement of the organ. The liver can also be enlarged (hepatomegaly) and cause a dull feeling of pressure in the right upper abdomen. Approximately one in ten patients with MDS develops lymph gland cancer.
Myelodysplastic Syndrome: Causes and Risk Factors
In healthy people, the so-called stem cells of the blood go through various stages of maturation and division in the bone marrow. At the end of these processes, red blood cells, white blood cells and platelets are formed. In patients with MDS, the stem cells of the bone marrow are degenerate and normal blood formation (hematopoiesis) is disrupted. The pathologically altered stem cells produce masses of functionless cells. These die off quickly or are sorted out in the spleen. Of the three rows of cells in the blood (red blood cells, white blood cells, platelets), one, two or all three can be degenerate. If all three rows of cells are degenerate, it is called pancytopenia. In some patients who have myelodysplastic syndrome, the immature stem cells multiply massively and uncontrollably over time. The MDS then turns into acute leukemia. This is why a myelodysplastic syndrome is also called pre-leukemia.
The reasons for this degeneration of blood formation have not been clarified in over 90 percent of cases (primary myelodysplastic syndrome). In ten percent of those affected, however, triggers can be found more or less reliably (secondary myelodysplastic syndrome). Most of the time, there are chromosome changes in the genetic make-up in this case. The more chromosome changes there are, the more serious the clinical picture. The triggers include:
- Previous chemotherapy with cell toxins (cytostatics)
- Radiation (for example, to treat cancer or in nuclear power accidents)
- Radioiodine therapy (for hyperthyroidism or thyroid cancer)
- Benzene and other solvents
Myelodysplastic Syndrome: Investigations and Diagnosis
The right person to contact if you suspect a myelodysplastic syndrome is a specialist in internal medicine who specializes in blood disorders or cancer (hematologist, hemato-oncologist). At the doctor's appointment, the doctor first inquires about your current symptoms and any previous illnesses (anamnesis). If you suspect myelodysplastic syndrome, the doctor could ask you the following questions, for example:
- Have you been tired and exhausted lately, or have you noticed a drop in performance?
- Do you get out of breath easily even with little physical exertion?
- Do you have frequent palpitations or dizziness?
- Have you been suffering from infections lately?
- Are you prone to punctiform skin hemorrhages (petechiae) and increased nosebleeds?
- Have you had radiation or chemotherapy in the past?
After the anamnesis, the physical examination follows. The doctor primarily checks whether the liver or spleen is enlarged and whether the lymph nodes are swollen. Since a myelodysplastic syndrome is primarily a blood disease, a blood test is essential. It also serves, among other things, to clarify possible other causes for the symptoms.In addition to the blood, the bone marrow is also examined if myelodysplastic syndrome is suspected.
Myelodysplastic syndrome: blood test
The first indication of a myelodysplastic syndrome is a blood test. The sample examined typically contains fewer blood cells than in a healthy person. The different cell types can be affected in different combinations or alone. Most of the time the red blood cells are decreased (anemia). Unlike in iron deficiency anemia, the iron content in these cells is not changed or even increased. In addition, the white blood cells and platelets may be decreased (leukopenia and thrombocytopenia). However, sometimes the white blood cells are also increased.
A myelodysplastic syndrome can affect the size and hemoglobin content of the blood cells in addition to a change in the number of cells. The red blood cells can be enlarged (macrocytic) or reduced (microcytic), have a changed shape and a decreased (hypochromic) or increased hemoglobin content (hyperchromic). The blood count is used to assess whether there are more immature blood precursor cells. This is also an indication of impaired blood formation. In order to clarify other possible causes for the symptoms, the iron storage level ferritin and the cell decay parameter LDH are also determined in the blood. Vitamin B12, folic acid and erythropoietin are involved in blood formation and are therefore often also checked.
Myelodysplastic Syndrome: Bone Marrow Puncture
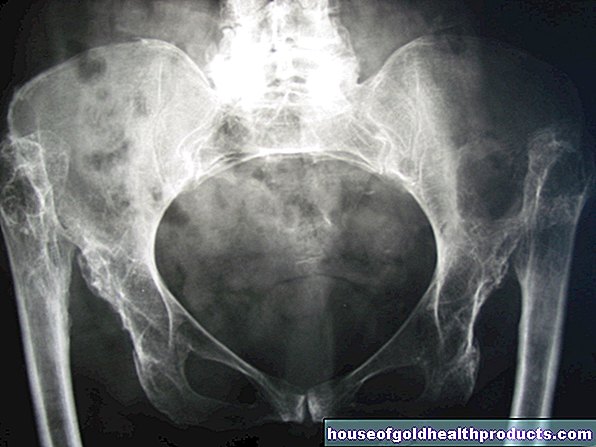
If an abnormal blood test suggests myelodysplastic syndrome, a bone marrow biopsy can confirm the suspected diagnosis. Because in MDS, too, more and more immature precursors (blasts) of normal blood formation can be found in the bone marrow. During this examination, the patient is usually given sedative or light sleep medication. General anesthesia is usually performed on children. Then an area in the iliac crest or in the sternum is disinfected and covered with sterile cloths. To prevent the patient from developing pain during the biopsy, a local anesthetic is injected under the skin. The doctor can then use a needle to remove cells and tissue from the bone marrow. Then cells and tissues are examined in the laboratory. For the subsequent therapy of the myelodysplastic syndrome it is important to prove whether and how the genetic material of the bone marrow cells has been changed. This is achieved with a chromosome or gene analysis.
Myelodysplastic Syndrome: Treatment
A myelodysplastic syndrome is determined and classified according to the appearance and nature of the bone marrow and blood cells under a microscope. Depending on the microscopic changes in the blood-forming cells, the World Health Organization (WHO) differentiates between two types of myelodysplasia, each of which requires different therapeutic measures: the high-risk MDS and the low-risk MDS. The criteria for this classification include the type and proportion of changed cells in the blood and bone marrow. MDS is treated in specialized departments of a hospital or, particularly recommended, a university clinic.
Myelodysplastic Syndrome: Treatment of Low Risk MDS
In the case of low-risk MDS, "supportive therapy" is used, which refers to supportive treatment of the disease. One tries to replace the loss of function without being able to cure the disease. Myelodysplastic syndrome may require the following supportive measures:
- Transfusion of red and white blood cells or platelets
- Medicines that bind iron in the blood (iron chelators). This is necessary because the repeated blood transfusions cause iron overload in the body.
- Early administration of antibiotics for any unclear infection
- Vaccination against pneumococci and annual flu vaccination
- Avoid using non-steroidal pain relievers or cortisone
Myelodysplastic Syndrome: Growth Factors
A myelodysplastic syndrome leads to a lower cell concentration of certain types of cells in the blood. In order for the body to produce more new cells of this type of cell, blood formation can be stimulated by certain drugs. The hormone erythropoietin (also known as EPO in sports doping) or valproic acid can be administered to produce more red blood cells. For the other cell rows there are also stimulators that stimulate the formation of new cells.
Myelodysplastic Syndrome: Immunomodulators
Myelodysplastic syndrome also affects the cells of the immune system. In certain cases, drugs that suppress or modulate the immune system can help. In the long term, this means that patients will have to have fewer blood transfusions. This therapy can also cause the number of platelets in the blood to rise again.
Myelodysplastic Syndrome: Treatment of High Risk MDS
There are several options for treating myelodysplastic syndrome in the high-risk group, including changing the DNA metabolism (e.g. with azacytidine or decitabine), intensive chemotherapy or an "allogeneic stem cell transplant". Stem cell transplantation is the only treatment option that can potentially cure the disease. All cells in the patient's bone marrow are destroyed by radiation and chemotherapy. Since a person cannot live without blood formation, donor stem cells have to be implanted by another person. These divide and start blood formation again. However, it is not always easy to find a donor who is genetically similar enough to qualify as a donor.
In principle, the possibility of a stem cell transplant should be examined in all patients with high-risk MDS before, for example, interfering with the DNA metabolism. If a stem cell transplant is not possible, the other methods of treatment are used.
Myelodysplastic syndrome: disease course and prognosis
Overall, the prognosis for MDS is rather poor. Particularly unfavorable factors are a high proportion of blasts in the blood, complex chromosomal changes, a high level of cell decay in the blood test, older age, previous illnesses and a reduced general condition.
Depending on the risk group, the diagnosis of "myelodysplastic syndrome" differs between life expectancy and the course of the disease. Patients at high risk survive an average of five months. However, with high-risk MDS, there is sometimes the possibility of stem cell therapy and thus a potential chance of a cure. If there is a type of disease with a low risk, life expectancy can increase to an average of 68 months. Over 60 percent die of infections, bleeding or a sudden acute myeloid leukemia (AML). These complications are a direct consequence of myelodysplastic syndrome.
Tags: Baby Child anatomy prevention
.jpg)