Dental fistula
Tanja Unterberger studied journalism and communication science in Vienna. In 2015 she started her work as a medical editor at in Austria. In addition to writing specialist texts, magazine articles and news, the journalist also has experience in podcasting and video production.
More about the experts All content is checked by medical journalists.A tooth fistula is often caused by bacterial inflammation of the tooth root. Initially, a fistula in the mouth does not cause any noticeable symptoms. Over time, those affected feel a feeling of pressure on the tooth and slight pain. In addition, the gums are unnaturally reddened. Tooth fistulas do not usually heal on their own and require treatment by the dentist. You can find out more about causes, symptoms and treatment here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K04

Brief overview
- Description: Connection between a cavity filled with pus, e.g. triggered by an inflamed tooth root, and the oral cavity
- Symptoms: At first there is a slight swelling and reddening of the gums as well as a feeling of pressure on the tooth; Over time, the pain increases until the pus drains into the oral cavity via the tooth fistula.
- Causes: The cause of tooth fistulas is usually an inflammation of the tooth, tooth root or tooth root tip.
- Prognosis: With timely treatment, the chances of recovery are good. If left untreated, a dental fistula can lead to tooth loss and damage to the jawbone in the long term.
- Treatment: as early as possible; Treatment with antibiotics; Removal of the inflamed root tip, possibly pulling the affected tooth; The fistula is opened by a minor surgical procedure
- Diagnosis: Talk to the doctor (anamnesis), physical examination (e.g. inspection of the teeth and oral cavity, cold test on the affected tooth, X-ray)
- Prevention: Careful, daily dental hygiene; Quit smoking, regular checkups at the dentist, healthy lifestyle
What is a tooth fistula?
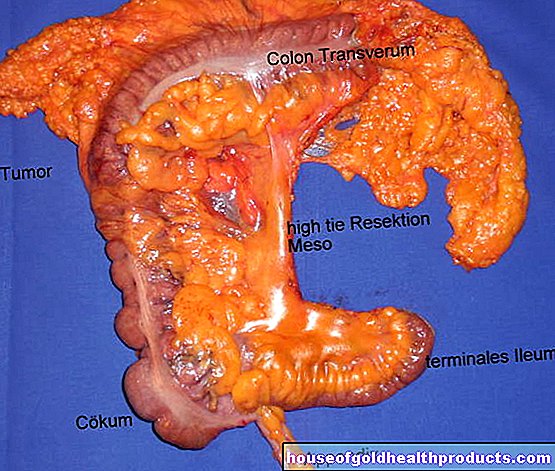
Dental fistulas are unnatural, tube-like passages or connections between a cavity filled with pus and the mucous membranes in the oral cavity (e.g. gums). Fistulas are used to allow fluids such as pus that has accumulated in the tissue cavities due to the inflammation to flow through or drain. The principle is comparable to a drainage channel.
Fistulas on the tooth or gum usually develop due to a bacterial infection at the tooth root or the tip of the tooth. The tooth is usually damaged by caries, which means that bacteria and other pathogens penetrate the tooth root and multiply.
This creates inflammation in the tissue. As it progresses, a pocket of pus forms. When the pressure is increased, the dental fistula opens and the purulent secretion then flows from the focus of the infection (fistula base) via the fistula canal into the oral cavity.
Fistulas do not only occur in the mouth, but everywhere on the human body. Examples are anal fistulas, intestinal fistulas or vaginal fistulas.
How do dental fistulas, tooth abscesses and aphthae differ from one another?
Dental fistulas, abscesses and aphthae differ in cause and structure. Aphthae are painful but mostly harmless damage to the oral mucosa. They develop as a result of a strong immune system reaction that causes tissues to die. Triggers are, for example, illnesses, injuries or stress. Aphthae usually heal on their own within a few weeks.
Fistulas and abscesses are usually triggered by bacteria that invade the tissues of the mouth, multiply there and cause inflammation. While the resulting pus in a fistula often empties itself if the pressure is too high, in an abscess the focus of inflammation is encapsulated by the surrounding tissue. An abscess must always be opened surgically.
Both dental fistulas and abscesses on the tooth, if left untreated, sometimes lead to complications such as tooth loss or inflammation of the jawbone. In rare cases there is a risk of life-threatening blood poisoning (sepsis). The risk is when a fistula becomes clogged, encapsulated, and becomes an abscess. If this is not treated in time, the pathogens from the accumulation of pus in the abscess may spread through the bloodstream in the body and cause blood poisoning.
While abscesses and aphthae generally form in the entire oral cavity, for example on the roof of the mouth or on the tongue, dental fistulas usually only develop on the gums above individual teeth.
How do you recognize a fistula in the mouth?
A tooth fistula usually occurs on only one tooth in the lower or upper jaw. The symptoms are very mild at the beginning. Often, those affected initially only feel swelling on the gums and a feeling of pressure or tension on the tooth. Above the tooth on the oral mucosa, a small, blister-like elevation forms, which fills with pus. The inflamed area is unnaturally red and sometimes tender to the touch.
If too much pus accumulates and the pressure in the tooth fistula becomes too great, it will eventually burst and the pus will empty into the oral cavity via the fistula duct. Usually the pain diminishes for a short time. However, the fistula itself does not go away and fills again with pus after a short time.
The more the inflammation progresses, the more the pain usually increases. Even gently touching the affected area with the tongue is often perceived as painful by people with a tooth fistula. Those affected often perceive a throbbing on the tooth.
Since the symptoms usually decrease again when the fistula bursts, those affected often do not consult a dentist for several weeks or even months. Some sufferers have a tooth fistula for years before going to the dentist.
In order to accelerate healing and avoid consequential damage, you should consult a dentist as soon as possible if you have symptoms.
Why do you get a tooth fistula?
The most common cause of a tooth fistula in the oral cavity is bacterial inflammation of the tooth root, more precisely the tip of the tooth root. The bacteria (especially streptococci and staphylococci) usually get to the tooth root when the tooth has already been damaged, for example by caries. If the inflammation is left untreated for a long time, a dental fistula will eventually form above the inflamed tooth.
Gum pockets, which are formed by inflammation of the gums (gingivitis), are also possible triggers for dental fistulas. These occur, for example, when the teeth are not carefully brushed and as a result more bacteria accumulate on the gums. A bacterial inflammation of the teeth holding apparatus (periodontitis) is also a possible trigger for dental fistulas in the mouth.
Smoking, poor nutrition (for example a lot of sugar) and poor dental hygiene also increase the risk of dental fistulas and at the same time slow down healing. Other risk factors are: inflammation of the oral mucosa, tooth inflammation, a weakened immune system and injuries to the mouth and throat.
Who is affected?
Tooth fistulas, which are caused by infections in teeth, tooth roots and tooth supporting structures, mainly affect people between the ages of 20 and 40. However, dental fistulas occur at any age, including children and adolescents.
In addition, people with previous illnesses (such as diabetes mellitus, bronchial asthma) or immunocompromised people (e.g. after a stem cell transplant or chemotherapy) as well as heavy smokers and alcoholic people are more often affected by infections in the oral cavity.
How dangerous are fistulas in the mouth?
With early treatment, the chances of recovery from dental fistulas are good. However, those affected usually do not see a dentist until the symptoms worsen. This delays healing.
If patients do not seek medical treatment, the inflammation may progress further. The open wound becomes infected again and again with bacteria. The inflammation spreads and may also damage the jawbone.
In rare cases, a fistula becomes blocked, encapsulated, and becomes an abscess. Then there is a risk that the bacteria from the accumulation of pus in the abscess will spread over the blood in the body and cause blood poisoning (sepsis). This is especially true for abscesses that are not treated or not treated in time.
Sepsis is life-threatening for those affected because, in severe cases, it leads to the failure of vital organs such as the heart or kidneys. Patients need medical treatment in a hospital as soon as possible, usually in an intensive care unit.
Dental fistulas sometimes reappear despite treatment. Then a new treatment at the dentist is necessary.
As long as the inflammation is not completely healed, there is still a risk that fistulas will recur.
How do you treat a tooth fistula?
The dentist usually treats a dental fistula with antibiotics to stop the bacteria from spreading. Those affected take these as tablets every day. The doctor determines the dosage and use, depending on how far the inflammation has progressed.
In order to specifically combat the inflammation and avoid antibiotic resistance, it is sometimes necessary to have the pathogen determined in a laboratory (antibiogram).
If the cause of the tooth fistula is an inflamed tooth root, the doctor removes the affected part of the root tip (root tip resection). In some cases it is necessary to completely remove the tooth to stop the inflammation.
Depending on how far the inflammation has progressed, where it is and how big the accumulation of pus is, the doctor opens the tooth fistula with a scalpel. He numbs the affected area with a locally effective anesthetic (local anesthesia) and opens the fistula through a small incision.
This causes the pus to drain into the oral cavity; if necessary, the doctor sucks off any pus that remains in the wound with a small suction device. Even after this procedure, the doctor usually prescribes antibiotics to speed up healing and reduce the risk of re-inflammation.
If the inflammation is localized, the cause of the inflammation has been eliminated and there are no other risk factors (e.g. immunodeficiency), the doctor sometimes dispenses with antibiotics.
Often these measures are enough for a tooth fistula to heal. In some cases, however, dental fistulas return despite treatment (for example on a root-treated tooth or after a tooth has been extracted). Then a new visit to the dentist is necessary.
Under no circumstances should you prick or squeeze out a tooth fistula yourself. This may make the inflammation worse and delay healing.
Although the cause of a tooth fistula cannot be remedied with simple home remedies, in some cases it is possible to alleviate the symptoms to a certain extent. Rinsing with chamomile tea helps some patients with dental fistulas. Clove oil, which is applied to the closed fistula with a cotton swab, is also said to help against the symptoms.
The effect of these home remedies has not been adequately proven scientifically. Before using these, please ask your dentist for advice.
After the treatment of the dental fistula, it is necessary for those affected to have the healing process checked regularly by the dentist until the symptoms have subsided. In this way, those affected reduce the risk of complications and prevent re-inflammation.
How does the doctor make a diagnosis?
In the event of toothache and symptoms in the mouth area, the dentist is the first point of contact. He first conducts a detailed conversation with the person concerned (anamnesis). The doctor asks, for example, how long the symptoms have existed and whether the person has pain or other symptoms (e.g. fever).
Then he examines the tooth and mouth area. To do this, he examines the teeth and the mouth for visual abnormalities such as swelling, unnatural reddening, discoloration or injuries.
He then usually carries out a cold test. Using this test, the doctor can quickly determine whether the tooth root or the tooth nerve is still intact, damaged or has already died. To do this, the doctor touches the affected tooth with a cotton swab that he has previously cooled with a cold spray. If the nerve is still intact, those affected are sensitive to the cold. With a dead nerve, patients no longer feel the cold.
The dentist then takes x-rays of the jaw. He can then tell how far the inflammation has progressed and whether the jawbone has already been attacked.
If there are complications such as inflammation of the jawbone, the dentist may refer you to an oral surgeon or an oral and maxillofacial surgeon. If necessary, the doctor will carry out further examinations such as an ultrasound examination (sonography), computed tomography (CT) or magnetic resonance tomography (MRT) in order to assess the spread of the inflammation and possible damage to the jawbone.
How do you prevent a tooth fistula?
To prevent a tooth fistula, dentists recommend that any inflammation of the tooth or the tooth root be treated as soon as possible. It is best for those affected to contact a dentist at the first symptoms such as feeling of pressure, swelling and / or slight pain.
Preventive measures also ensure that a fistula does not develop in the first place. Please note the following:
- Maintain thorough, daily oral and dental hygiene.
- Use dental floss to clean hard-to-reach areas and spaces between your teeth.
- Have your teeth checked by the dentist at least once, ideally twice a year.
- Have your dentist professionally clean your teeth at least once a year.
- Strengthen your immune system: eat a balanced diet, exercise regularly, avoid stress and maintain your social contacts.