Regulatory Affairs
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
The search for new active ingredients against certain diseases or ailments is tedious and does not always end with success. Out of 5,000 to 10,000 hopefuls that are tested in the research laboratories of the pharmaceutical companies, on average only one ends up as a finished drug in the pharmacy. And there is an average of 13.5 years in between.

Search for the "target"
Even before tests are carried out with new substances, the researchers think about the properties of the substance in question and what reaction it should trigger in the body. This can be, for example, lowering blood pressure, blocking a certain messenger substance or releasing a hormone.
To this end, the researchers are looking for a suitable "target", ie a point of attack in the disease process, at which an active ingredient can attach and thus positively influence the disease process. In most cases the target is an enzyme or a receptor (docking point on cells for hormones or other messenger substances). Sometimes the patient is also lacking a certain substance. Then it quickly becomes clear that the drug you are looking for should compensate for this deficiency. A well-known example is insulin in people with diabetes (diabetes mellitus).
Search for the active ingredient
As soon as a target has been determined, the scientists search for an active substance that can act on the chosen point of attack (screening). That usually means: test, test, test. Up to 300,000 different substances are examined for their suitability every day (high-throughput screening = HTS). Of these, about every 200th to 1000th substance actually shows an effect on the selected target, even if sometimes only a very small one. Such a hit is referred to as a "hit".
The test substances are mostly chemically - i.e. synthetically - produced. For some time now, genetically engineered substances have also been gaining in importance. They are obtained with the help of genetically modified cells (such as certain bacteria) and form the basis of biopharmaceuticals (biological drugs).
optimization
In most cases, the "hits" found still need to be optimized. Sometimes, for example, the effectiveness of a substance can be increased if its structure is changed slightly. In these experiments, the scientists often work with computer simulations, with the help of which the effect of a chemical change on the substance can be estimated in advance. If the prognosis is good, the substance is adjusted in real life, i.e. in the laboratory. Their effect on the target is then examined again.
In this way, the researchers gradually improve a new active substance, which usually takes several years.In the best case scenario, they will eventually reach the point at which the substance is ready for the next step: a patent application is filed and then subjected to preclinical studies as a so-called active ingredient candidate.
Preclinical Studies
In the preclinical (preclinical) development phase, the drug candidate is tested in test tubes (e.g. on cell cultures) and on animals. On the one hand, this involves pharmacological issues, for example what happens to the substance in cells or in an entire organism:
- How is it received?
- How is it distributed in the body?
- What reactions does it trigger?
- Will it be modified or dismantled?
- Will he be eliminated?
On the other hand, the scientists are investigating exactly what effect the substance has on the target, how long it lasts and what dose is necessary for it.
Above all, however, preclinical studies serve to answer questions about the toxicity (toxicity) of the drug candidate. Is the substance poisonous? Can it cause cancer? Is it able to change genes? Can it harm an embryo or fetus?
Many drug candidates fail the toxicity tests. Only those substances that pass all safety tests are allowed to enter the next development phase with studies on humans (clinical studies).
Whenever possible, preclinical tests are carried out in test tubes, for example on cell cultures, cell fragments or isolated human organs. However, some questions can only be answered in tests on a living organism - and animal experiments are necessary for this.
Clinical studies
The drug candidate is being tested on humans for the first time in clinical studies. A distinction is made between three study phases that build on one another:
- Phase I: The drug candidate is tested on a few healthy volunteers (test subjects).
- Phase II: This is followed by tests on a few sick people (e.g. on high blood pressure patients if the drug candidate is to become a new antihypertensive drug).
- Phase III: Now the test is carried out on a large number of sick people.
Each study phase must be approved in advance by the responsible bodies: On the one hand, this includes the responsible national authority - depending on the drug candidate, either the Federal Institute for Drugs and Medical Devices (BfArM) or the Paul Ehrlich Institute (PEI). On the other hand, every clinical study needs the permission of an ethics committee (consisting of doctors, lawyers, theologians and laypeople). This procedure is intended to protect the study participants in the best possible way.
The pharmaceutical manufacturer who developed the drug candidate can conduct the clinical studies themselves. Or he assigns a "Clinical Research Organization" (CRO) to do this. This is a company that specializes in conducting clinical studies.
Phase I studies
Usually 60 to 80 healthy adults who have volunteered for this act as test persons in phase I. After a comprehensive explanation and the consent of the study participants, they are initially only given a small amount of active ingredient.
In up to 30 consecutive tests, the scientists check whether the findings from the examinations in the test tube and on animals can also be transferred to humans - i.e. whether the active ingredient is absorbed, distributed, converted and excreted again as it would in the preclinical Tests determined. In addition, it is investigated how well the test persons tolerate the drug candidate.
Tablet, syringe or ointment?
After successfully completing phase I, so-called galenics come into play: The scientists are now working on the optimal "packaging" for the active ingredient - should it be administered into the vein as a tablet, capsule, suppository, syringe or infusion?
The answer to this question is very important: the dosage form has a major influence on how reliably, how quickly and for how long the active ingredient can fulfill its task in the body. It also affects the type and severity of possible side effects. Some active ingredients are much better tolerated as an injection than when they enter the body in tablet form via the gastrointestinal tract.
In addition, galenical experts check whether and which auxiliary substances should be added to the new preparation. For example, something that improves the taste of the drug or acts as a carrier or preservative.
You can read more about the search for the right "packaging" for a new active ingredient and for suitable auxiliary materials in the article Galenics - Manufacture of pharmaceuticals.
Phase II and Phase III studies
After the healthy subjects in phase I, it is the turn of the sick from phase II to test the drug candidate:
- Phase II: Here the new drug candidate is tested on mostly 100 to 500 patients. The focus is on the effectiveness, optimal dosage and tolerability of the preparation.
- Phase III: The same tests are carried out here as in Phase II, only on significantly more patients (several thousand). In addition, attention is paid to possible interactions with other drugs.
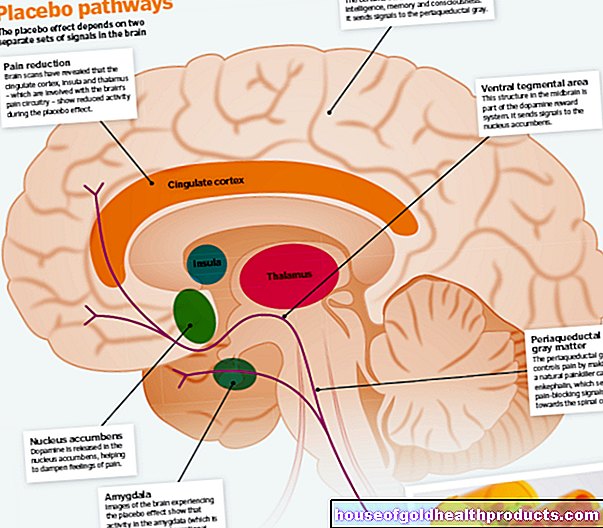
In both phases, different treatments are compared with each other: Only some of the patients receive the new preparation, the rest receive either a usual or familiar standard medication or a placebo - a preparation that looks exactly like the new one but does not contain any active ingredient (dummy drug) . As a rule, neither the patient nor the attending physician know who is getting what. Such "double-blind studies" are designed to prevent the hopes, fears or skeptical attitudes of doctors and patients from influencing the outcome of the treatment.
Granting approval
Even if a new drug has passed all the required studies and tests, it cannot simply be sold. To do this, the pharmaceutical company must first apply for drug approval from the competent authority (see below: Approval options). This carefully checks all study results and, in the best case scenario, grants the manufacturer permission to bring the new drug onto the market.
Phase IV
Even after a drug has been approved, the authorities and the pharmaceutical company keep an eye on the new preparation, for example with regard to rare side effects. These are undesirable effects that occur in less than 1 in 10,000 patients treated and are therefore hardly detectable in the previous study phases (with smaller patient groups). Doctors are required to report any unforeseen side effects of a drug.
If necessary, the licensing authority then requires the manufacturer to point out these newly discovered side effects in the package insert. However, it can also issue restrictions on use: If, for example, rare but severe side effects in the kidney area were discovered, the authorities can order that the drug may no longer be used in people with existing kidney diseases.
In extreme cases, the authority can also withdraw the approval of a drug entirely if, over time, unacceptable risks have emerged from its use. Sometimes the manufacturer then voluntarily withdraws such a product from the market.
Doctors also use logs to record how the new drug is doing in everyday life for their patients. The manufacturer uses the results of such observations for use, for example, to improve the dosage or dosage form of the preparation.
Sometimes everyday practice also shows that the active ingredient helps against other diseases. The manufacturer then usually continues research in this direction - with new phase II and III studies. If successful, he can also apply for approval for this new indication.
Approval options
In principle, a pharmaceutical company can apply for approval for a new drug either for the entire EU or only for a single member state:
Centralized approval process
The drug approval is applied for here directly at the European Medicines Agency (EMA). The approval authorities of the EU member states also participate in the subsequent test. If the application is approved, the preparation can be sold anywhere in the EU. This approval process takes an average of one and a half years and is mandatory for some drugs (e.g. for biotechnologically manufactured preparations and for cancer drugs with new active ingredients).
National approval process
The application for approval is submitted to national authorities and therefore only in the country concerned. In Germany, the Federal Institute for Drugs and Medical Devices (BfArM) and the Paul Ehrlich Institute (PEI) are responsible for this. The BfArM takes care of the majority of human pharmaceuticals, the PEI takes care of sera, vaccines, test allergens, test sera and test antigens, blood and blood products, tissues and drugs for gene therapy and cell therapy.
Drug approval in several EU countries
In addition, there are two other options if a pharmaceutical company wants to obtain approval in several EU countries:
- Decentralized procedure: In a "Decentralized Procedure" (DCP), a pharmaceutical company can apply for national approval for a new drug in several countries of the European Economic Area at the same time.
- Mutual Recognition Procedure: If a drug already has a national approval in a country of the European Economic Area, this can be recognized by other member states within the framework of the "Mutual Recognition Procedure" (MRP).
The application for approval for a new drug is very expensive for pharmaceutical companies. For example, processing an application for approval for a completely new active ingredient at the EMA costs around 260,000 euros in the simplest case.
Standard approval
Some drugs are released for sale via a standard approval: These are not newly developed preparations, but those whose manufacture is based on certain monographs stipulated by the legislator. In addition, these medicinal products must not pose any danger to humans or animals. In a monograph (e.g. for paracetamol suppositories 250 mg), among other things, the composition and dosage of the preparation in question is precisely defined - as is the area of application.
If all these requirements are complied with, the manufacturer does not have to apply for its own, individual drug approval. This enables him to bring drugs to the market at a very affordable price. Standard approvals exist for charcoal tablets (250 mg), atropine eye drops and solutions in various concentrations, as well as paracetamol suppositories and acetylsalicylic acid tablets in various dosages.
Pharmacists, for example, are also allowed to prepare and then sell a saline solution according to the instructions in the relevant pharmacopoeia monograph. However, you must indicate the use of such a standard approval to the approval authority and the responsible state authority.
Other ways of getting drug approvals
In the EU, in addition to the conventional approval procedure, there are also options for making a new drug available earlier than usual. These are not just quick approvals. Rather, attempts are being made in various ways to ensure that those affected can benefit from active ingredients even without traditional drug approval. Experts speak of so-called adaptive pathways:
Compassionate use programs
Here, very specific patients receive drugs that are actually still in clinical trials. The prerequisite is that there is no longer any other treatment option and the patient cannot participate in a corresponding study on this drug. These exemptions must be applied for separately for each individual patient.
Conditional approval for medicinal products
This is, so to speak, a rapid approval. The strict effectiveness and safety tests do not have to be present to the extent that is otherwise customary. However, certain conditions apply:
- The conditional drug approval is limited in time.
- The manufacturer must provide the missing documents that are necessary for regular drug approval
The conditional approval is used, for example, in pandemics in order to quickly provide a suitable drug against the infectious disease.
Approval under exceptional circumstances
This special route exists, for example, for rare diseases. Since there are very few sick people, it is not possible for the pharmaceutical company to submit the otherwise necessary amount of data for examination. With this drug approval, however, the manufacturer usually has to check annually whether there are new data and findings.
Accelerated drug approval (accelerated assessment)
The approval documents are checked and evaluated more quickly by the responsible EMA committee - instead of the usual 210 in 150 days. This path is possible if there is a promising active ingredient against a disease that could not be treated properly up to now.
Priority medicines (PRIME)
In such cases where a need is still unmet, the EMA and the drug manufacturer can work together very early on - even during the first tests. In this way, the experts can evaluate efficacy and safety at an early stage and initiate further procedures more quickly if the drug proves to be promising.
Continuous review (rolling review)
In the case of urgently needed drugs and vaccines, the EMA can - as already noted - "conditionally" approve the active ingredients or work with the manufacturers at an early stage before final approval. In important cases, the so-called rolling review process begins before these approvals. The experts evaluate existing data before the manufacturer can submit all the documents otherwise relevant for approval. In addition, they continuously check all new results obtained from further studies.
For example, the EMA applied the rolling review process to the conditional approval of the viral drug remdesivir during the coronavirus pandemic. As part of the approval process for corona vaccines, the experts also checked the results that were already available and then obtained during the ongoing phase III studies.
Medicines for children
New drugs usually go through several studies before they are allowed to hit the market. For a long time, however, one group of patients received less attention in research: children and adolescents. For the treatment of minors, the dosage of a drug that has been tested in adults was often simply reduced.
Since 2007, however, every new drug in the EU has had to be tested on minors in phase II and III studies if it is to be used later in this age group. Tests on children or adolescents are often only started once the phase II studies on adults have been successfully completed. A separate group of experts from the European Medicines Agency EMA, the Pediatric Committee, decides on the details.
The admission tests on minors make sense because the bodies of children and adolescents often react differently to a drug than that of adults. Effectiveness and tolerability can therefore be different. The dosage must therefore usually be adjusted for minors. In many cases, a different form of administration is required for medication for children - such as drops or a powder instead of the large tablets that adult patients receive.
Herbal medicines
When developing new herbal medicinal products (phytotherapeutic agents), the proof of efficacy, as prescribed in the form of clinical studies, is difficult:
While chemical drugs usually contain no more than one or two pure substances, each plant produces a mixture of active substances. Most of the time, this mix also varies in different parts of the plant. For example, the nettle herb can affect the kidneys, whereas the nettle root can affect the hormone metabolism of the prostate. In addition, these active ingredient mixtures vary greatly depending on the origin and preparation of the plant, which also influences the effectiveness.
In 1978, a group of experts, the so-called Commission E, was set up to clarify such questions. These contain the information known at the time about the composition, effects and possible side effects of the various medicinal plants.
Because the monographs of Commission E have not been updated since 1994, the monographs of the "Committee on Herbal Medicinal Products" (HMPC) are used instead. This is the European Medicines Agency's committee responsible for herbal medicines. He takes care of the scientific evaluation of such drugs.
A distinction must be made between traditional herbal medicinal products and modern herbal medicinal products: instead of approval, registration is required. More on this in the next section.
Registration instead of admission
Traditional herbal medicinal products as well as homeopathic preparations are exempt from the licensing requirement as "special therapies" medicinal products. Instead, you need to register:
For this - as with the approval of "normal" medicinal products - proof of the harmlessness and the appropriate pharmaceutical quality of the homeopathic or traditional herbal medicinal product must be submitted.
In the case of traditional herbal medicinal products, the pharmacological effect or effectiveness must also be plausibly demonstrated - using what is known as traditional evidence. This means that the manufacturer must use bibliographical information to prove, among other things, that the traditional herbal medicinal product has been used medically in the EU for at least 30 years, including at least 15 years.
Clinical studies to prove the effectiveness, as prescribed by the classic drug approval, are, however, neither necessary for homeopathic nor for traditional herbal medicines so that a company can sell them.
In contrast to traditional drugs in conventional medicine, alternative remedies usually lack extensive scientific evidence of their effectiveness, especially since no complex drug approval procedure is required.
Tags: palliative medicine teenager alternative medicine