Imipramine
Benjamin Clanner-Engelshofen is a freelance writer in the medical department. He studied biochemistry and pharmacy in Munich and Cambridge / Boston (USA) and noticed early on that he particularly enjoyed the interface between medicine and science. That is why he went on to study human medicine.
More about the experts All content is checked by medical journalists.The active ingredient imipramine is an antidepressant and belongs to the class of tricyclic antidepressants. It was the first antidepressant that worked reliably and served as a precursor for numerous other active ingredients against depression. Here you can read everything you need to know about the effects and use of imipramine, interactions and side effects.
This is how imipramine works
In the brain, the nerve cells communicate with each other via chemical messengers (neurotransmitters). During this process of signal transmission, a nerve cell releases a neurotransmitter that is perceived by the next nerve cell via certain docking points (receptors). The messenger substance is then taken up again in the original cell. There are a number of different messenger substances. Some only transmit excitatory signals (such as norepinephrine), others inhibitory signals (such as GABA). Some neurotransmitters can have both inhibitory and excitatory effects (such as dopamine). Aside from these general functions, some neurotransmitters are also linked to certain higher-level functions. For example, serotonin is also known as the “happiness hormone”.
Depression as a clinical picture is very complex and not yet fully understood by experts. One of the theories for their emergence is the “monoamine deficiency hypothesis” (the term monoamine stands for chemical messenger substances): In experiments (on animals, for example) it can be observed that depressive symptoms are associated with a deficiency in certain neurotransmitters such as serotonin, norepinephrine and dopamine can be correlated. This does not necessarily mean that this neurotransmitter deficiency is the cause of depression. However, we know from experience that increasing these messenger substances with drugs often leads to an alleviation of the mental illness.
Imipramine serves this purpose: it increases the concentration of the neurotransmitters serotonin and norepinephrine by preventing the nerve cells from taking up these messenger substances again. Imipramine also acts on a number of other messenger substances.
Imipramine and equally effective antidepressants (antidepressants of the imipramine type) are considered to be drive-neutral, that is, they have neither drive-increasing nor depressant or calming effects on the patient. In this respect, they differ from antidepressants of the desipramine type (drive-enhancing; for inhibited-depressed patients) and antidepressants of the amitriptyline type (depressive-calming; for anxious-aroused patients).
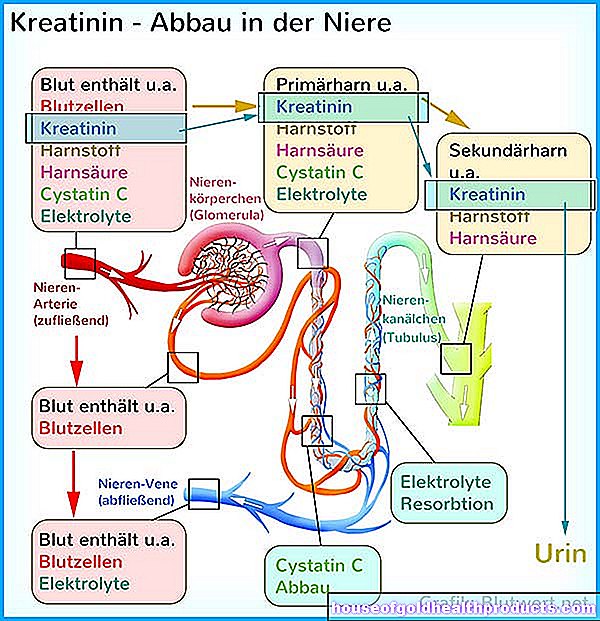
Imipramine uptake, breakdown and excretion
Imipramine is absorbed into the blood via the intestines and immediately transported to the liver. A large part of the active ingredient (one to three quarters) is already broken down there. Some of the conversion products are still antidepressant. The degradation substances are excreted in the urine via the kidneys. After just half a day, only half the amount of active ingredient is left in the body.
When is imipramine used?
The active ingredient imipramine is approved for:
- Treatment of depression (usually in addition to psychotherapy)
- Treatment of night terrors and bed-wetting in children over five years of age
Outside of the approved areas of application ("off-label" application), the active ingredient is also used against anxiety and phobias.
The use in depression usually extends over a longer period of time, whereby the doctor should regularly check whether the use of the antidepressant is still necessary.
This is how imipramine is used
The antidepressant imipramine is taken as a tablet with a glass of water with or without meals. Treatment is usually started with 25 milligrams of imipramine twice a day, and the dosage is then slowly increased until it is optimally effective ("creeping dosage"). Usual daily doses are between 50 and 150 milligrams of imipramine (rarely up to 300 milligrams), which are divided equally into two with three doses in the morning, possibly at noon and in the evening. To stop treatment, the imipramine dose should be tapered, i.e. reduced slowly and gradually.
What are the side effects of imipramine?
Imipramine side effects in more than one in ten patients are drowsiness, tremors, dizziness, dry mouth, nasal congestion, sweating, hot flashes, constipation, low blood pressure (especially when getting up from a lying or sitting position), racing heart, and weight gain.
Often there are also tiredness, sleep disorders, restlessness, confusion, paresthesia, headaches, problems urinating, palpitations and cardiac arrhythmias, nausea, feeling thirsty, vomiting, loss of appetite, skin reactions and sexual dysfunction.
Many side effects become more pronounced at the beginning of treatment with imipramine and decrease or go away as the treatment progresses.
What should be considered when taking imipramine?
If other depressant or sedative drugs (allergy drugs, pain relievers, drugs for epilepsy or psychiatric diseases) are taken or alcohol or drugs are consumed during treatment with imipramine, this can lead to an intensified depressant effect. This also applies to the simultaneous use of drugs that have an inhibiting effect on urine excretion and secretion (dry eyes, dry mouth), such as certain Parkinson's drugs and anti-allergy drugs.
As a rule, other antidepressants should not be combined with imipramine, as this can lead to serious side effects. Certain blood pressure medication (clonidine, alpha-methyldopa) should also not be taken together with the active ingredient imipramine.
Some medicines increase the number of liver enzymes that break down imipramine. This can greatly weaken its effect. Such drugs are, for example, sleeping pills (barbiturates), anti-epilepsy drugs and hormonal contraceptives (such as “the pill”). A doctor should therefore carefully weigh the benefits and risks against each other before using such drugs and imipramine at the same time.
Nicotine can also make imipramine less effective.
In patients being treated with anticoagulants, blood coagulation should be checked closely at the start of imipramine therapy and, if necessary, the dosage of the anticoagulant adjusted.
Imipramine use may increase existing thoughts of suicide. Patients at risk should therefore be closely monitored, especially in the first few weeks of treatment.
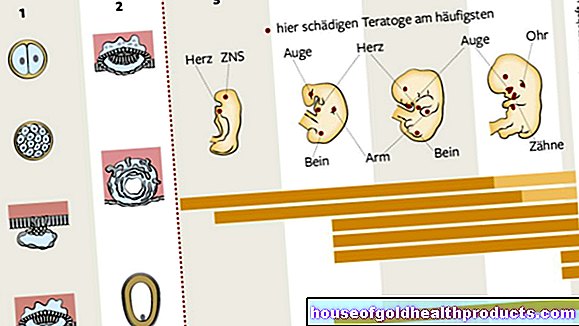
Pregnant women, breastfeeding women and children under 18 years of age (for uses other than night terrors and bed-wetting) must not take imipramine. In children and adolescents as well as elderly patients, a lower dosage should usually be selected.
How to get imipramine medication
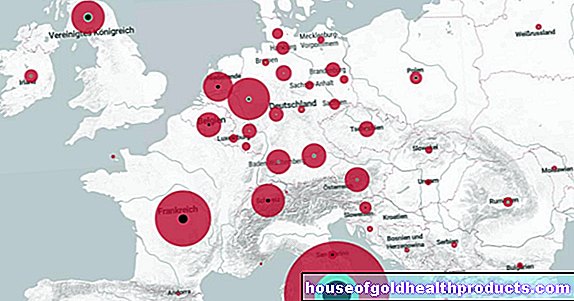
In Germany, drugs with the active ingredient imipramine are only available on prescription in any dosage and pack size.
How long has imipramine been known?
The antidepressant imipramine was originally intended to be a new neuroleptic (active ingredient against psychoses and delusions) from the pharmaceutical company Geigy (now Novartis). In this regard, however, it was found to be ineffective in clinical studies. Instead, the psychiatrist Roland Kuhn observed in 1957 that imipramine was suitable for treating depression. Medicines containing this active ingredient were introduced as antidepressants in 1958.
Tags: pregnancy birth womenshealth home remedies