Creutzfeldt-Jakob disease
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the experts All content is checked by medical journalists.Creutzfeldt-Jakob disease (CJD) is a fatal disease of the nervous system. Patients suffer from rapidly progressing dementia, movement disorders, or muscle twitching. So far there is no therapy. Read more about the symptoms, diagnosis and therapy of Creutzfeldt-Jakob disease here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A81
Creutzfeldt-Jakob disease: description
Creutzfeldt-Jakob disease was first described in 1920 by the neurologists Creutzfeld and Jakob. It is one of the so-called transmissible, spongy brain diseases (Transmissible Spongiform Encephalopathies, TSE). In these diseases, the brain tissue loosens up like a sponge and the brain gradually loses its function.
Creutzfeldt-Jakob disease can come in different forms. These include:
- Sporadic CJD (develops spontaneously for no apparent reason, is most common with 80 to 90 percent of cases)
- Familial CJD (hereditary)
- Transferred CJD (for example the new variant of Creutzfeldt-Jakob disease (vCJD))
Transmissible spongiform encephalopathies are known not only in humans but also in the animal kingdom. What they have in common is that they easily jump over species boundaries, for example being transferred from a sheep to a cattle or from a cattle to humans. The TSE "scrapie" has been known in sheep for around 200 years. In the 1990s, there were many cattle with bovine spongiform encephalopathy (BSE), particularly in the UK. As a result of this epidemic, the new variant of Creutzfeldt-Jakob disease has appeared in humans since 1996. To date, 219 cases of vCJD have been reported worldwide, 175 of which came from the UK. So far, no case of vCJD has been reported in Germany.
In Germany around 100 people develop sporadic CJD every year. This number has remained the same for years and is easy to determine, since both suspected Creutzfeldt-Jakob disease and death from it must be reported to the health department. Family-related cases of CJD are excluded from this.
Creutzfeldt-Jakob disease: symptoms
Creutzfeldt-Jakob disease manifests itself in a so-called encephalopathy - a collective term for diseases of the brain. It shows itself mainly through the following symptoms:
- Psychological abnormalities (e.g. depression, hallucinations, delusions, apathy, personality changes)
- Rapidly progressing dementia (with confusion, altered perception, difficulty concentrating)
- Uncoordinated movements (ataxia)
- Involuntary muscle twitching (myoclonia)
- Sensory disturbances
- Balance disorders
- Uncontrollable muscle movements (chorea)
- Muscle stiffness (rigor)
- Visual disturbances
The most important symptom of the sporadic Creutzfeldt-Jakob disease is dementia. In vCJD, the psychological abnormalities predominate, the dementia only occurs later in the course of the disease.
Creutzfeldt-Jakob disease: causes and risk factors
Creutzfeldt-Jakob disease: prions as a trigger
Creutzfeldt-Jakob disease is caused by so-called prions. Prions are infectious protein particles that withstand most disinfection processes. They are also immune to extreme heat or radioactive radiation. Basically, prions are “mere proteins” and their structure is much simpler than the bacteria, viruses, fungi or parasites that cause most infectious diseases. Prions have only been known as pathogens for a few years and have not yet been fully researched. Scientists suspect that prions are formed when a normal protein is misfolded and takes on a new structure. This protein in turn causes other proteins to form defective structures as well. In this way, many misfolded proteins accumulate in the body and are mainly deposited in nerve cells. The nerve cells are damaged and perish, resulting in a spongy loosening of the brain.
Creutzfeldt-Jakob disease: origin of prions
Different prions are responsible for the development of Creutzfeldt-Jakob disease. In sporadic CJD, nothing is known about the exact mechanism of prion formation.
The familial Creutzfeldt-Jakob disease arises due to incorrect genetic information. A mutation in the genome causes proteins to be assembled incorrectly and prions to form. Over 30 different mutations are known to date. They are all inherited as an autosomal dominant trait. This means that this genetic information prevails over another and only one parent has to carry the faulty gene in order for the child to become ill too.
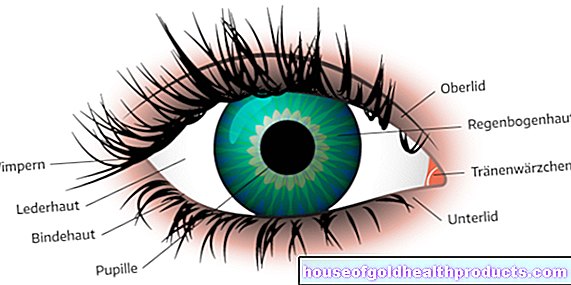
Creutzfeldt-Jakob disease is transmitted in different ways. It can, for example, be transferred to a patient during operations through contaminated neurosurgical surgical instruments or blood transfusions. Infection is also possible through a corneal transplant in the eye or a transplant of hard meninges (dura mater) if the donor suffered from Creutzfeldt-Jakob disease. In the past, growth hormones from the pituitary gland of cadavers were used for therapy. The Creutzfeldt-Jakob disease could also be transmitted.
A few years ago there was a custom among tribes in New Guinea to ritually ate the brains of the dead. As a result, the disease (Kuru disease) spread there strongly. And the new variant of Creutzfeldt-Jakob disease is also a transferred form. Most likely, the cause is beef contaminated with BSE pathogens that was eaten by patients.
Creutzfeldt-Jakob disease: BSE
Everything you need to know about Creutzfeldt-Jakob disease: BSE can be found in the article BSE.
Creutzfeldt-Jakob disease: how can you protect yourself?
To protect yourself from Creutzfeldt-Jakob disease, you should avoid using beef products made from nerve tissue, such as beef brain. In addition, the feeding of animal meal to farmed animal species has been banned in order to exclude as far as possible that risk material enters the human food chain. Milk and dairy products are risk-free. Since the outbreak of the BSE epidemic in the 1990s, there has been a BSE test for slaughtered cattle in Germany. This test has been abolished for healthy cattle since 2015. There is currently no vaccination against the disease.
Creutzfeldt-Jakob disease: examinations and diagnosis
The doctor makes the diagnosis of Creutzfeldt-Jakob disease primarily on the basis of clinical symptoms. Before the physical examination, the doctor will ask you the following questions, among others, in order to record your medical history (anamnesis):
- What day is today?
- Where are you?
- Are you content?
- Did a relative of yours suffer from Creutzfeldt-Jakob disease?
- Did you have a cornea transplant?
Creutzfeldt-Jakob disease: investigation
Your doctor will then examine you physically and test the functioning of the nervous system. This includes coordination exercises or force measurements as well as the examination of reflexes and sensation of touch.
Nerve fluid (cerebrospinal fluid) is often obtained with a lumbar puncture. This flows around the brain and spinal cord and can contain clues to possible causes of the disease. Under local anesthesia, the doctor inserts a cannula into the lower back of the seated patient and pushes it forward to the so-called spinal canal, in which the spinal cord is surrounded by liquor.If the patient suffers from Creutzfeldt-Jakob disease, there are often high concentrations of certain proteins such as the proteins “14-3-3” or “tau”. This is not the case with the vCJK.
In addition, the doctor can record the brain waves with an electroencephalography (EEG). To do this, electrodes are attached to the patient's head. A device records the electrical activity in the brain. In Creutzfeldt-Jakob disease, specific changes appear in the EEG from around twelve weeks after the onset of the disease. These changes rarely occur in vCJD.
Magnetic resonance imaging (MRI) is used to show the spongy loosening and shrinking of the brain. Changes that indicate possible protein deposits can also be seen in certain areas of the brain (often in the basal ganglia).
Creutzfeldt-Jakob disease: autopsy
Creutzfeldt-Jakob disease can only be confirmed with certainty after the patient's death. To do this, the pathologist takes tissue samples from the brain and examines them under the microscope after the protein deposits in the nerve cells have been stained with dyes. In about a third of patients, prions are also found in the spleen and muscles.
Creutzfeldt-Jakob disease: treatment
So far, there is no therapy that addresses the causes of Creutzfeldt-Jacob disease. That is why the doctor treats the individual symptoms in a targeted manner as part of what is known as symptomatic therapy. Research is currently underway into drugs that can cure the disease.
The doctor can prescribe anticonvulsants for muscle twitching. These drugs are also used in seizure therapy. In Creutzfeldt-Jakob disease, the active ingredients clonazepam and valproic acid are mainly used. Antidepressants are also used for depression, so-called neuroleptics for hallucinations and restlessness.
Creutzfeldt-Jakob disease: disease course and prognosis
Creutzfeldt-Jakob disease is incurable and always ends fatally after a short time. How long it takes after infection until the disease breaks out (incubation period) has not yet been conclusively clarified. It is believed that it could take years to decades.
The course differs depending on which form of Creutzfeldt-Jakob disease the patient suffers. The sporadic form usually occurs between the ages of 60 and 70 and progresses rapidly. It usually leads to death within six months. Family-related Creutzfeldt-Jakob disease progresses somewhat more slowly and begins around the age of 50. Patients develop vCJD much earlier, before the age of 30. The new variant of Creutzfeldt-Jakob disease lasts longer and ends fatally after around twelve to 14 months.
Tags: desire to have children travel medicine tcm