ganglion
and Carola Felchner, science journalistClemens Gödel is a freelancer for the medical team.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.A ganglion is also called an overleg. A somewhat misleading name: It is not about ossification, but rather a fluid-filled bulging of a joint or tendon covering. Usually it forms in the area of the hand. But it can also occur on the foot or knee. Apart from the fact that a ganglion doesn't look that nice, it usually doesn't cause any symptoms. Read here, among other things, how an excess leg is created, how you can recognize it and how you can get rid of it!

Brief description
- What is a ganglion? A fluid-filled, bag-like cavity on the joint, usually on the hand, less often on the knee, foot or spine
- Symptoms: resilient bulge from a few millimeters to a few centimeters in diameter, possibly pressure pain, restricted mobility or numbness, but often no complaints at all
- Causes: Not exactly known. Connective tissue weakness and risk factors such as joint diseases or increased stress on the joints probably play a role.
- Attending physician: orthopedist or surgeon
- Diagnosis: consultation with the patient, physical examination, possibly imaging procedures and fine needle aspiration
- Treatment: if necessary, only observation and physiotherapy, otherwise surgery or aspiration possible
- Prognosis: mostly favorable course, but ganglia often return
Ganglion: description
Ganglion is the medical term for an excess leg. This name is a relic from a time when it was assumed that it was a bony structure. In fact, a ganglion is a cystic sac, i.e. a fluid-filled cavity that usually arises in joints (arthrogenic).Ganglia are connected to the joint via a kind of socket, which is why they can hardly be moved.
Ganglia occur most frequently on the hand (in around 65 percent of cases): The ganglion occurs here particularly on the back of the hand. Sometimes fingers or wrists are also affected. Less often there is an excess leg on the hips, knees, feet or spine.
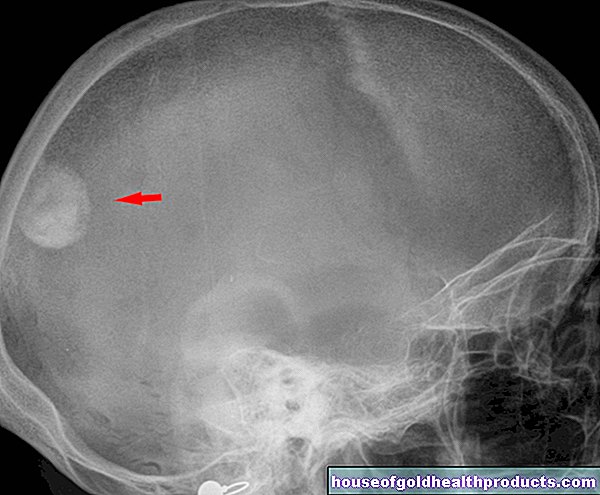
This is what a ganglion looks like
More rarely, a ganglion can also appear on the tendon sheaths (tendinogenic). In this case one speaks of a tendon sheath ganglion. Another special form of the transom is the so-called intraosseous ganglion, which forms in a bone. So it bulges inwards instead of outwards.
In principle, people of all ages can get an over-leg, including children. Most often, however, it occurs between the ages of 20 and 30. Women are affected more often than men. The reasons are her naturally weaker connective tissue and more flexible joint capsules.
Ganglion: symptoms
Those affected usually notice a bump on the wrist or back of the hand, less often on other parts of the body. Several over-legs can also develop.
The "bump" on the wrist or other parts of the body is typically resilient. It has an average diameter of a few millimeters to two centimeters. But there are also ganglia that can grow up to eight centimeters. Some also remain so small that the person concerned does not even notice the protuberance and it is only discovered by chance.
Typically, a ganglion does not cause pain and is otherwise hardly noticeable. Depending on the size and location, however, it can restrict the mobility of joints and muscles or be painful if the person concerned leans on them. The (pressure) pain can also radiate. The ganglion can also hurt when moved or touched.
If an excess leg presses on tendons, it can squeeze them and possibly cause inflammation (tendinitis) due to the permanent strain.
Numbness, tingling, or weakness in the hand can indicate that the ganglion is “pinching off” a nerve. The nerves in so-called ring ligament ganglia are often affected. These are small over-legs on the ring ligaments of the fingers that can make bending and stretching difficult. But the wrist or foot (back) are also susceptible to pinched nerve tracts and vessels. The pressure on vessels can cause bleeding. In addition, infections can spread in the fluid-filled space of the ganglion.
Ganglion: causes and risk factors
The exact causes of a ganglion are not yet known. Several factors are likely to play a role in the development of an excess leg. This could be, for example, a weak connective tissue:
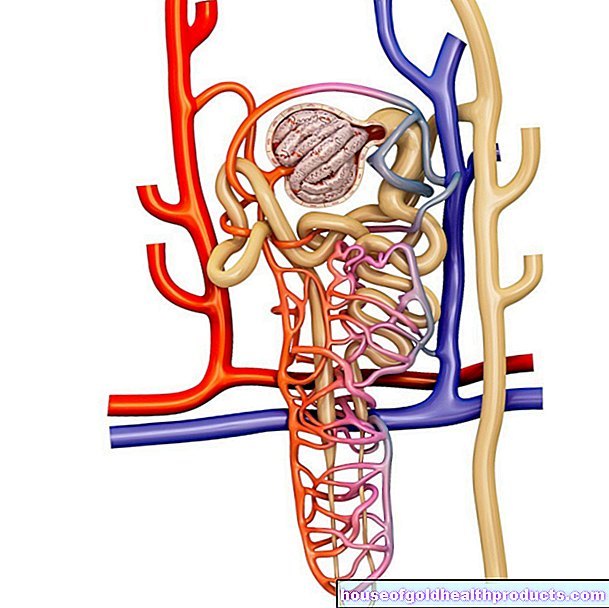
There is (solid) connective tissue around the joints, the so-called joint capsule. This holds the joint in position and ensures that it only moves in the desired direction. In the joint, a soft layer of connective tissue (synovial membrane) lines the joint cavity like wallpaper. In the joint cavity there is bile-like fluid ("synovial fluid"), without which the bony parts of the joints would rub against each other.
If the connective tissue is weak, in connection with overstressing the joint, synovial fluid can leak out of the joint cavity and collect in the surrounding soft tissue. This is how a ganglion arises, experts suspect.
Risk factors for ganglia
Risk factors for a ganglion include:
- increased stress on the joints as a result of repeated minor injuries to the capsule and ligamentous apparatus
- Disorders of the biomechanics of the joint or tendon
- Joint diseases and rheumatic diseases (such as osteoarthritis, lupus erythematosus, gout)
About ten percent of the patients had previously injured themselves in the area of the ganglion. In addition, in a ganglion, the connective tissue cells (fibroblasts) probably stimulate the production of synovial fluid. Their components hyaluronic acid and so-called mucopolysaccharides form a viscous liquid, which then accumulates in the upper leg.
In addition, damage to the tissue caused by wear and tear probably also plays a role in the development of a ganglion.
Ganglion: examinations and diagnosis
If you suspect a ganglion, see an orthopedic surgeon or surgeon. He can possibly rule out underlying diseases such as osteoarthritis as a trigger of the knob. The best thing to do is to contact a doctor who specializes in the affected body region, for example a hand surgeon for an excess leg on the hand.
To clarify the suspected ganglion, the doctor usually proceeds as follows:
Survey of the medical history: In a conversation with the patient, the doctor inquires about the exact complaints as well as possible injuries and underlying or previous illnesses. Possible questions from the doctor in this anamnesis interview are, for example:
- When did you first notice the swelling?
- Does the swelling affect the mobility of the affected part of the body or is it painful?
- Have you ever injured yourself in the affected area?
- Have you ever had similar "knobs" before?
- Is there similar swelling elsewhere?
Physical Exam: After this, the doctor will examine the swelling to assess it more precisely. A ganglion feels resilient, similar to a solid rubber ball. Because it is anchored to the joint or the tendon sheath, it can only be moved a little. In contrast to highly inflammatory processes, the affected region is neither overheated nor reddened. The doctor may take a few photos for documentation.
In addition, he will check the blood circulation, motor skills and sensitivity in the area of the affected body region. For example, it can detect movement restrictions caused by the ganglion, circulatory disorders and nerve damage. It is also possible to “shine through” the swelling (transillumination): By shining through the ganglion from the side with a light source, the doctor can determine whether the inside is fluid (indicating a ganglion, cyst) or solid.
Imaging: Imaging techniques are unusual for ganglia. They are only used when the case is unclear and, for example, there is a suspicion of a malignant process or arthritis. Even if the doctor suspects a “hidden” ganglion, ultrasound and magnetic resonance imaging (MRI) can confirm or refute this suspicion.
Fine needle aspiration: For diagnostic and therapeutic purposes, the doctor can use ultrasound guidance to pierce a very thin, hollow needle into the ganglion in order to extract fluid from the inside. This mostly viscous but clear liquid is then examined by a pathologist in the laboratory. In this way, inflammation or malignant processes can be ruled out. The drainage of fluid from the ganglion causes it to visibly shrink. In most cases this is not a permanent solution.
Ganglion: treatment
If a ganglion does not cause any symptoms, it does not necessarily have to be treated. Some ganglia also disappear on their own after a while.
However, many sufferers perceive an over-leg as cosmetically annoying or it causes them discomfort (e.g. pain with certain movements, limited mobility). Then treatment is advisable. Basically, there are three ways you can treat an excess leg: conservative treatment, aspiration and surgery. Which method is used in each individual case depends on several factors, such as the location of the ganglion. The patient's wishes are also taken into account when planning ganglion therapy.
The so-called Bible or hammer therapy is not recommended! This brute (self-therapy) method was often used for ganglia in the past. One tries to smash the upper leg with a Bible or a hammer. Hence the name "Bible cyst" for ganglia. In the worst case, bones break.
Conservative treatment
A ganglion that does not affect the person affected can initially only be observed. The fuselage may recede spontaneously or on its own with the help of physiotherapy. Immobilization can prevent it from getting bigger. It is also important to avoid incorrect loading of the affected joint. After around three months of conservative treatment, the doctor discusses with the patient in most cases how the therapy should be continued.
aspiration
Aspiration, as the doctor may have already used to make a diagnosis, can also be used therapeutically. In this form of ganglion treatment, the doctor pierces the upper leg with a fine hollow needle and sucks off the fluid it contains (needle puncture). Usually, however, new fluid accumulates within a short period of time (ganglion recurrence).
Therefore, after aspiration, the doctor sometimes injects corticosteroids (cortisone) into the "emptied" ganglion. It is supposed to prevent renewed swelling.
Another possibility is to inject the enzyme hyaluronidase into the ganglion. It breaks down the main component of the contained liquid (hyaluronic acid). The doctor then sucks off the liquid by means of aspiration.
surgery
The surgical removal of a ganglion is very promising if it is carried out by an experienced specialist. The surgeon removes the upper leg and tries to close the joint so that no more fluid escapes. A ganglion operation can in principle be carried out openly (via a larger skin incision) or minimally invasive (arthroscopic). As a rule, only local or regional anesthesia is required for the over-leg operation.
In some cases, such as a ganglion finger, a ganglion wrist or a ganglion foot or a ganglion foot, a so-called tourniquet can be applied during the procedure. It reduces the flow of blood to the affected area and thus the risk of major bleeding. During the procedure, care must be taken to ensure that the ganglion is removed completely (without residue) and that important surrounding structures such as vessels, nerves or tendons remain unharmed.
After the operation, the operated area should first be spared and immobilized. The patient may need to wear a splint for a period of time. Accompanying physical therapy can help prevent the joint from stiffening.
Ganglion surgery complications
Complications occur in every tenth open operation. Arthroscopic interventions and aspiration procedures, on the other hand, cause problems much less frequently with four and two percent respectively. In particular, vascular (bleeding) and nerve injuries (numbness, paralysis) are more common in open operations. There is also the risk of infections, wound healing disorders and the development of Sudeck's disease (a chronic pain syndrome). In addition, as after every operation, a (small) scar remains.
Ganglion: disease course and prognosis
A ganglion is a benign protuberance with a favorable course. It can recede spontaneously, but it can also enlarge. Usually it doesn't cause any discomfort. Depending on the location, however, it can cause (pressure) pain or numbness or limit the mobility of the affected joint.
If a ganglion has been treated successfully, there is a risk of relapse (relapse): a new ganglion can form in the same or in a different location. Surgery seems to be the most sustainable on an excess leg: only around every fifth patient has a cystic protuberance in the same place after an open operation. With a minimally invasive operation, the risk of relapse is even lower. However, after aspiration treatment, half of the patients develop an overleg again.
In order to prevent relapses, risk factors for ganglia should be reduced and the muscles relaxed and loosened again and again during the day. This prevents overloading, which can favor a ganglion.
Tags: desire to have children palliative medicine drugs