Meningioma
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.The meningioma is a mostly benign tumor of the meninges. It grows slowly and often causes symptoms such as seizures or headaches late in the day. The tumor forms mainly in women around 50 years of age. It can be treated well with surgery and radiation therapy, but in many cases it returns after a few years. Here you can read everything you need to know about meningioma.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D43C71D33

Meningioma: description
Meningiomas are tumors of the soft meninges. With a share of around 25 percent, they are among the most common neoplasms in the central nervous system. Most adults around the age of five develop a meningioma. Only two percent of these tumors are diagnosed in children and adolescents. Women are affected twice as often as men.
Most meningioma is benign and grows slowly over several years. It is rarely malignant and grows faster. The tumor is usually well demarcated from the neighboring brain structures and does not grow into other tissues. It can grow flat or knotty and sometimes calcify. Often the skull bone is thickened over the tumor.
In over 90 percent of cases, a meningioma grows in the skull (intracranial). There it is mostly found on the meninges that separate the two hemispheres from each other. More rarely, it grows in the sphenoid sinus or in several places. However, it can also form on the meninges of the spinal cord in the spinal canal. Depending on where the tumor is located, it can cause different symptoms.
Meningioma classification
The World Health Organization (WHO) divides meningiomas into three different degrees of severity:
- Grade I: meningioma
- Grade II: atypical meningioma
- Grade III: anaplastic meningioma
Both treatment and prognosis are influenced by this classification.
Grade I meningioma makes up over 85 percent of all meningiomas. It is benign and can usually be completely removed by surgery.
About ten percent of meningiomas are atypical (grade II). They can grow a little faster and often return even after a successful operation (relapse).
The anaplastic meningioma (grade III) is rather rare with a share of two to three percent. It is classified as malignant and can spread to distant organs (metastasis).
Meningioma: symptoms
It can sometimes take several years for a meningioma to cause symptoms. This is because the tumor usually grows very slowly. Only when it displaces neighboring structures such as nerves or important brain regions do the first signs of disease appear.
Meningioma symptoms are rather unspecific and can also occur in other diseases.If the tumor is in the center of movement, individual muscle groups, for example on the arms or legs, can be paralyzed. On the other hand, if it grows in the olfactory trough, odor disorders occur. Some sufferers gradually smell less and less over a longer period of time, which many do not even notice.
Meningioma can also irritate the meninges and cause a seizure. Some patients have headaches. In general, changes in personality, fatigue, visual and language problems are also conceivable. The malignant cells very rarely grow into the bones and the scalp overlying them. Then you can possibly feel it.
Often a meningioma grows so slowly that the brain can adapt to this new formation and there are no symptoms at all. Then it is sometimes discovered accidentally during an imaging exam.
Meningioma: causes and risk factors
A meningioma forms from the cover cells of the soft meninges. The soft meninges cover the brain. The hard meninges and the skull connect to the outside.
A meningioma occurs when one of the cover cells begins to grow in an uncontrolled manner. Why this happens is not yet fully understood. However, people who have had to undergo radiation therapy for another malignant disease are at a higher risk for the disease. In addition, the hereditary disease neurofibromatosis type 2 is associated with the formation of meningioma. It is not uncommon for this disease to have multiple meningiomas.
Meningioma: examinations and diagnosis
If a meningioma causes symptoms, a specialist in neurology (neurologist) is the right contact. He first inquires about the complaints and their temporal course as well as any previous and underlying illnesses (taking the medical history = anamnesis). As part of a neurological examination, he examines individual nerves, the sense of smell and the eyes. This is followed by further investigations.
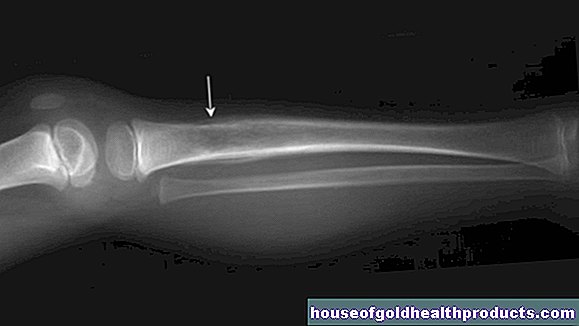
Images of the head or spinal canal must be made. The first thing that is usually done is a computed tomography (CT) scan. Some patients are given a contrast medium in a vein for the exam. In the CT, calcified structures and swelling of the surrounding brain tissue can be seen well. The contrast agent accumulates in the meningioma so that it becomes visible as a light structure in the image. A magnetic resonance imaging (MRI) scan can also be used to visualize the tumor very well. Both procedures allow the doctor to determine the exact size and location of the neoplasm.
An X-ray examination of the blood vessels (angiography) in the head can also be informative. This enables doctors to find out which vessels are connected to the tumor and must be considered during a subsequent operation. You can also see in this examination whether the tumor obstructs certain vessels and thereby restricts the blood flow.
Meningioma: treatment
Not every meningioma needs to be treated right away. If the tumor is small and does not cause any symptoms, it can be observed first. To do this, the radiologist makes images using CT or MRI at regular intervals and checks whether the tumor is growing.
When to treat a meningioma depends on a number of factors. It all depends on where the tumor is, how big it is and how aggressively it grows. In addition, the physical condition of the person concerned is taken into account.
Meningioma surgery
Surgery is the most suitable form of therapy for this type of brain tumor. The surgeon opens the skull bone with a saw and tries to remove the tumor as completely as possible. If the tumor is supplied by many or larger vessels, these can be closed before the operation (embolization). This avoids major blood loss during the operation. Since many important structures in the brain are located next to each other in a very small space, meningioma surgery is sometimes difficult and involves certain risks. Nerves, blood vessels and other brain structures can be injured, which can leave permanent damage. To prevent this from happening, sometimes the tumor cannot be completely removed. It is then destroyed by subsequent radiation therapy.
Meningioma: radiation therapy
The tumor should be irradiated if surgery cannot completely remove it or if there are malignant cells in the tissue being examined. This improves the patient's prognosis. In certain cases, meningiomas are irradiated without prior surgery.
Meningioma: disease course and prognosis
The course of the disease and the prognosis very much depend on the WHO grade of the tumor and whether it can be completely removed. After a complete surgical removal, the tumor returns in about one in five patients within ten years, and after an incomplete operation in more than one in two. This number can be almost halved by radiotherapy after the procedure.
A malignant meningioma has a much worse prognosis than benign forms. Despite surgery and radiation therapy, it returns in up to 80 percent of cases. For this reason, the success of therapy in meningiomas should be checked regularly.
Tags: baby toddler magazine anatomy