mumps
and Martina Feichter, medical editor and biologistSophie Matzik is a freelance writer for the medical team.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Mumps (parotitis epidemica) is an acute viral infection that typically swells the parotid glands on the sides of the head or neck. Often children fall ill, but more often adolescents and adults - they account for more than half of all mumps illnesses in Germany! Mumps usually heals on its own without complications or long-term effects. Read more about mumps here: symptoms, infection, possible complications, treatment and prognosis.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. B26
Brief overview
- What is mumps? acute, contagious viral infection, also known as "goat peter" or "booby". Mumps is one of the childhood diseases, although in Germany more adolescents and adults are now suffering from it.
- Contagion: mostly via droplet infection or direct saliva contact (kissing), less often via indirect transmission through shared use of cutlery, glasses, etc.
- Symptoms: no or hardly any symptoms in around 40 percent of those infected. Otherwise initially unspecific symptoms such as fatigue, lack of appetite, fever, headache and body aches. Then painful swelling of the parotid gland on the side of the head / neck (one or both sides).
- Possible complications: including meningitis or encephalitis, inner ear inflammation or inflammation of the auditory nerve (possibly with permanent hearing loss), inflammation of the testicles, inflammation of the epididymis, inflammation of the ovaries, inflammation of the breast, inflammation of the pancreas, inflammation of the heart muscles, inflammation of the kidneys, inflammation of the joints, anemia
- Treatment: Relief of symptoms with pain relievers, antipyretic drugs, etc.
- Prognosis: Especially mumps in children is usually harmless. The older the patient, the more likely complications are. Lasting long-term effects such as deafness or infertility are rare.
Mumps: symptoms
Mumps does not trigger symptoms in all infected people: Around four out of ten infected people show no symptoms or only have very mild symptoms. Children under five years of age in particular often only develop symptoms that are similar to a simple cold (flu infection), such as a runny nose.
In other cases, the mumps virus infection is more noticeable:
The first symptoms of mumps are usually unspecific. For example, there may be loss of appetite, fever and headache and body aches. Many patients also complain of a general feeling of illness and feel weak and uncomfortable.
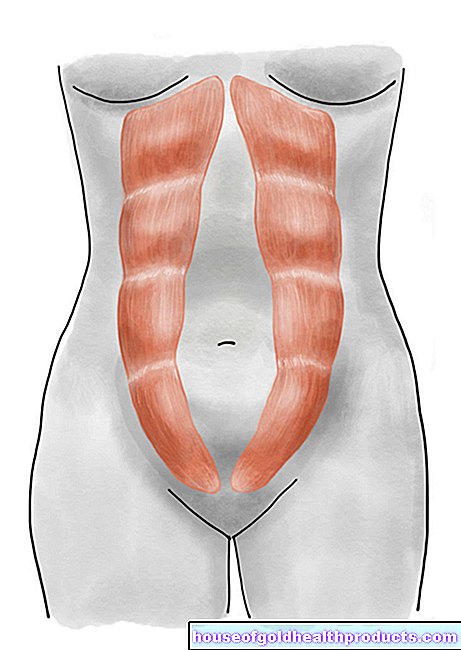
One to two days after the onset of the disease, the typical inflammatory swelling of the parotid glands (parotitis) begins. The paired parotid gland (parotid gland) lies on both sides of the face and extends from the zygomatic arch at the level of the ear to the corner of the jaw. With mumps, both parotid glands usually swell (sometimes one a little earlier than the second). More rarely, only one of the two glands is swollen. The swelling in the cheek and neck area leads to the typical "hamster cheeks" (especially in children). It usually subsides within three to eight days.
The swelling of the glands is often associated with pain: Pressure on the ear canal causes ear pain. Chewing and opening your mouth wide can also be painful. In severe cases, patients can only consume soft or liquid foods such as mashed potatoes, soups or porridge.
In some patients, in addition to the parotid glands, the paired salivary glands in the lower jaw or under the tongue also swell. Adjacent lymph nodes can also enlarge.
This is how you can recognize mumps
Mumps: complications
Mumps in children is very rare in causing complications. In contrast, mumps is much more problematic in adults. In general, the risk of complications from a mumps infection increases with the age of the patient. Such complications arise because the mumps virus spreads in the body and infects other organs.
Involvement of the central nervous system (CNS) is one of the most common complications in mumps. Men are more often affected than women. CNS involvement can manifest itself, for example, as meningitis (meningitis) or encephalitis (encephalitis):
- Symptomatic meningitis develops in one to ten percent of cases. An indication of this is when patients with mumps show signs such as stiff neck, nausea and vomiting, and listlessness or even loss of consciousness. There are no known permanent long-term effects or deaths from mumps meningitis.
- Less than one percent of people with mumps develop encephalitis. This so-called mumps encephalitis can lead to death in individual cases.
CNS involvement in mumps generally lasts seven to ten days. It usually becomes noticeable four to five days after the parotid glands swell. Sometimes it develops before that or is even the only symptom of the mumps infection.
Not only CNS involvement, but also the other complications of mumps infection can occur in people who do not show the typical mumps symptoms (as described above).
The mumps viruses can also cause inflammation of the inner ear (labyrinthitis) or inflammation of the auditory nerve (acoustic neuritis). In rare cases, those affected have permanent hearing loss (inner ear hearing loss).
A frequent complication of mumps in male adolescents and men is inflammation of the testicles (orchitis) at 15 to 30 percent. This mumps orchitis affects only one testicle, but sometimes both. Afterwards, fertility may be impaired. But testicular inflammation rarely leads to complete infertility. Inflammation of the epididymis (epididymitis) is also a possible consequence of a mumps infection.
Mumps in women is associated with breast inflammation (mastitis) in up to three out of ten cases. Inflammation of the ovaries (oophoritis) is much less common: up to five percent of adult women with mumps develop it.
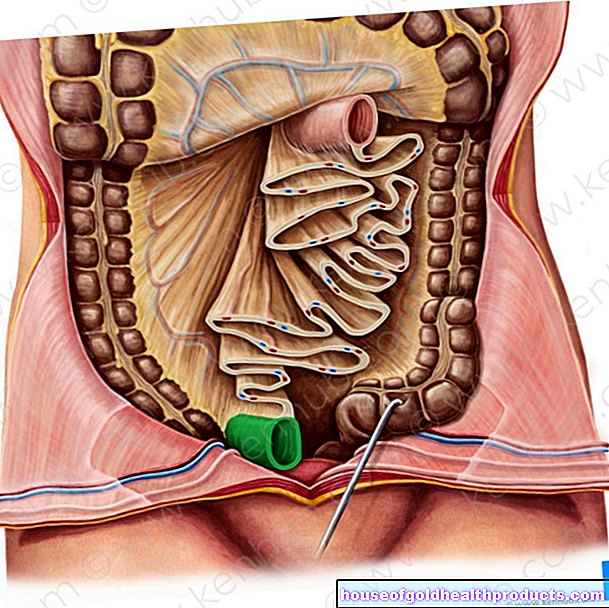
Sometimes mumps viruses cause inflammation of the pancreas (pancreatitis). This develops in about four percent of patients with mumps. Symptoms such as severe abdominal pain, nausea, and vomiting suggest pancreatitis.
Other possible complications of mumps are inflammation of the joints (arthritis), inflammation of the kidneys (nephritis), anemia, and inflammation of the heart muscle (myocarditis).
If people with mumps develop symptoms that are not classically associated with the disease, it is important to call a doctor. They could indicate a serious complication. The earlier the right therapy is started, the better and faster the recovery will be.
Mumps: pregnancy
Many women fear that an infection with the mumps virus can spread to the unborn child during pregnancy. According to the current state of knowledge, a mumps infection during pregnancy neither increases the risk of child malformations nor of a miscarriage. So the unborn baby is not at risk.
Mumps: contagion
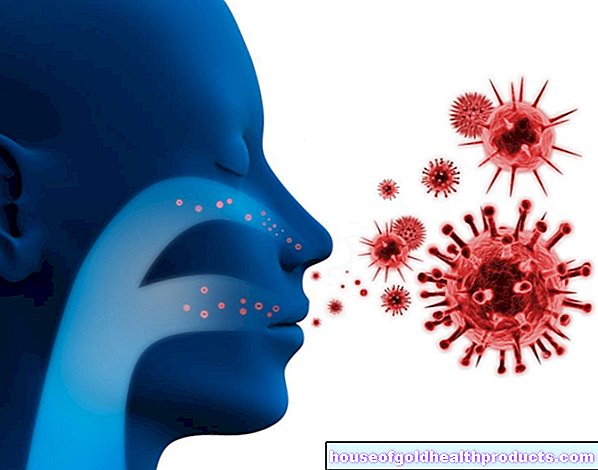
The mumps virus (paromyxovirus parotitis) belongs to the group of so-called paramyxoviruses, which also include measles viruses, for example. Infection occurs mainly via droplet infection: infected people distribute tiny droplets of saliva that contain the mumps virus into the surrounding air when they cough, sneeze or speak. Other people can become infected by inhaling these droplets of saliva.
Infection with mumps is also possible through direct contact with saliva, e.g. when kissing.
An indirect virus transmission occurs less often, i.e. via objects that are contaminated with infectious saliva. This can happen, for example, when a healthy person uses the same cutlery or glass as the infected person. However, mumps viruses on surfaces and objects only remain infectious for a few hours.
Anyone who has ever had mumps will usually never get it again. Infection with the virus generally results in lifelong immunity.
How long is mumps contagious?
Two days before to four days after the onset of the disease, patients are most contagious. In total, infected people can pass the mumps virus on to other people seven days before and up to nine days after the typical swelling of the parotid glands.
Even infected people who show no symptoms of the disease themselves can transmit the mumps virus to other people!
Mumps: incubation period
If you have become infected with the mumps virus, it will take some time for the first symptoms to appear (if any). This so-called incubation period can in principle be 12 to 25 days. Usually, however, 16 to 18 days pass between infection and the onset of the disease.
Mumps: examinations and diagnosis
In most cases, Peter’s disease can be easily recognized by the symptoms - especially the typical inflammatory swelling of the parotid glands (if this occurs). Because the disease has now become rare, the doctor should also carry out laboratory tests to be on the safe side. This is especially true if the patient is actually vaccinated against mumps (the vaccination protection could wear off over time).
Specific antibodies against the mumps virus can be detected in the blood of people infected with mumps. Specific IgM antibodies are usually found in an acute infection. They are already detectable in the first days of the disease. Your level will also remain elevated for a few weeks.
However, the test for specific IgM can also give a false positive result. Conversely, IgM antibodies against the pathogen can often not be detected in patients with mumps despite being vaccinated. In such cases, direct virus detection is therefore also recommended: To do this, the urine or a throat swab is examined for genetic material of mumps viruses. A second blood test can also be useful ten to 14 days after the first: A comparison of the blood levels of other specific antibodies against mumps viruses (IgG) can bring clarity - the IgG level in the second sample is more than four times that of the first Sample increased, this suggests a mumps infection.
Further investigations
If the disease is severe or complicated, further examinations are usually necessary. If, for example, there is a suspicion of involvement of the central nervous system, the doctor can take a sample of the cerebral and spinal cord fluid for direct detection of the pathogen (cerebrospinal fluid puncture). In the laboratory, one looks for fragments of the genetic material of the mumps virus in the CSF sample.
If a patient shows signs of inflammation of the pancreas or testicular inflammation, an ultrasound examination (sonography) can be useful for clarification. An ultrasound scan can also help diagnose inflammation of the ovaries as a result of mumps infection.
Mumps is notifiable
Mumps has been notifiable in Germany since 2013. Doctors must report suspected illnesses, proven illnesses and deaths from mumps to the responsible health authority, stating the patient's name.
If the patient visits or works in a community facility (such as a school, kindergarten), the facility management must be informed of the infection (by the person concerned or - in the case of children - by the parents). The management must then report the mumps infection to the health department.
Mumps: treatment
There is no causal (antiviral) therapy for mumps. However, the disease can be treated symptomatically, i.e. the symptoms can be alleviated:
Pouches help against the painfully swollen parotid glands. Most patients find cooling compresses pleasant. But some also prefer warm envelopes. You should try this out in individual cases. In the case of severe ear pain, the doctor can recommend a suitable pain reliever.
Patients with swallowing difficulties and pain when chewing should only consume light, pulpy or liquid foods such as mashed potatoes, milk porridge or soups. Acidic foods and juices are unsuitable during the illness. They stimulate the salivary glands to release more secretions. This can make the symptoms worse.
If you have a fever, bed rest and adequate hydration are advisable. For a high fever, you can make cold calf compresses and possibly take antipyretic medication (after consulting your doctor).
If mumps is associated with complications, these are also treated. For example, strict bed rest is recommended if you have testicular inflammation. In addition, the testicles should be elevated and cooled. In severe cases, the doctor will prescribe an anti-inflammatory drug. In the case of inflammation of the pancreas, the patient must be treated in the hospital. He is often given temporary artificial feeding and given anti-inflammatory medication. Appropriate treatment in hospital is also necessary for meningitis and meningitis.
Mumps: disease course and prognosis
Usually the prognosis for mumps is good. The infection is usually harmless, especially in children. With increasing age, however, the complications increase and these can sometimes have long-term consequences:
For example, testicular inflammation caused by mumps can reduce fertility. In rare cases, boys or men are completely sterile afterwards (sterility).
A temporary deafness in the area of high-frequency sounds is observed in about four percent of mumps patients. About one in 20,000 mumps cases causes lifelong deafness in one ear.
Mumps-related encephalitis is very rarely fatal: around 1.5 percent of patients with mumps encephalitis die.
When someone is allowed to visit or work in a community facility (school, day-care center, etc.) after suffering from mumps, the responsible health department or the treating doctor decides.
Mumps: vaccination
A vaccination can prevent mumps. It is recommended for all children: Within the first two years of life, the offspring should receive two doses of vaccine.Missed or forgotten vaccinations should be made up as soon as possible and before the 18th birthday. Vaccination is also recommended for adults in certain cases.
The purpose of the mumps vaccination is not just to protect yourself from infection. Those who are vaccinated cannot infect anyone else with mumps - especially not people who cannot be vaccinated against mumps (such as pregnant women or people with immunodeficiency).
You can find out more about recommendations for mumps vaccination, how the vaccine is administered and what side effects can occur in the article Mumps vaccination.
Additional information
- RKI guide "Mumps" from the Robert Koch Institute