Milk congestion
and Sabine Schrör, medical journalistNicole Wendler holds a PhD in biology in the field of oncology and immunology. As a medical editor, author and proofreader, she works for various publishers, for whom she presents complex and extensive medical issues in a simple, concise and logical manner.
More about the expertsSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.If the milk becomes blocked, the milk does not drain off completely and collects in the milk ducts. This leads to swelling and pain in the affected breast. Read here what you should consider when breastfeeding, for example, to prevent congestion and what you can do to treat acute congestion.

Brief overview
- What is milk congestion? Incomplete drainage of breast milk from the breast of nursing women. Milk congestion can occur during the entire period of breastfeeding, but it usually occurs in the third or fourth week after the birth. If left untreated, the blocked milk may develop into mastitis.
- Causes: lack of milk ejection reflex, mechanical causes (e.g. incorrect application of the child, incorrect sucking, too short or irregular breastfeeding times, clothes that are too tight, bra that are too small), excessive milk production.
- Symptoms: pain, hardening or small, palpable nodules in the affected breast, small, white blisters on the nipple. No fever, general well-being.
- Prevention: Empty the breast completely (breastfeed regularly, express or express excess milk), observe breastfeeding tips (e.g. first place the baby on the last emptied breast, the child's chin points to the affected breast area)
- Treatment: warm breast compresses before breastfeeding, cold breast compresses after breastfeeding, avoid stress
- When to the doctor If the chest pain increases and / or if the affected area is red, warmed and swollen. It is imperative to see a doctor if there are additional symptoms such as fever, general feeling of illness, chills, headache and body aches (suspicion of inflammation of the mammary gland!).
Milk congestion: description
If the milk becomes blocked, the breast milk that has formed in the breast cannot flow out completely. In principle, milk congestion can occur during the entire breastfeeding period. The first signs such as a hardened breast can appear shortly after the milk has come in. Most often, however, the milk does not build up until three to four weeks after the birth.
If left untreated, blocked milk can lead to inflammation of the mammary gland (mastitis). So that it doesn't come to that, you should follow a few tips to prevent milk congestion. You should consult a gynecologist or an experienced midwife in the event of acute congestion.
Milk congestion: what to do?
Milk congestion can be treated with various measures, such as properly placing the child on the breast. The same tips also apply to preventing milk congestion.
Empty chest
It is particularly important to empty the chest regularly to relieve the glandular tissue. You should therefore put your child on regularly (about every six hours). If you have more milk than your child drinks, you should manually rub out the overflowing breast or the individual lumps after breastfeeding. To do this, massage the breast gently in the direction of the wart, ideally under a warm shower. You can also express the excess milk. If you are unsure, you should contact your midwife, she will help you.
Breastfeeding properly
In the event of a blocked milk (and otherwise), pay close attention to the correct breastfeeding method: Always first place your baby on the breast where he last drank during the previous breastfeeding meal. The breast affected by the congestion must be emptied well. The correct position of the child can promote the flow of milk: the baby's chin should point towards the affected area of the breast. This is massaged by the suction movements, and the milk flows off more easily. Sometimes unfamiliar postures are necessary for this. If necessary, seek advice from an experienced midwife.
What else can help with blocked milk?
- Before breastfeeding, place moist, warm compresses (warm washcloths) on the affected side of the breast - this stimulates the flow of milk.
- After breastfeeding, apply cooling compresses (quark wrap / white cabbage wrap for 20 minutes) - this reduces pain.
- Avoid stress during breastfeeding or provide targeted relaxation (for example by means of a relaxation method, neck or back massage).
Oxytocin and alternative medicine
In the past, nasal sprays containing oxytocin were often prescribed to encourage the milk to drain away. However, it has not been proven that drugs containing this hormone additive are both effective and harmless at the same time. That is why they have not been approved in Germany since 2008.
Some women rely on homeopathy and acupuncture for congestion. However, the effectiveness of these alternative healing methods has not been adequately proven scientifically.
Milk congestion: symptoms
A milk blockage can be recognized by the following signs:
- local chest pain
- Hardened breasts, small palpable nodules
- only affected one breast
- no fever (body temperature <38.4 ° C)
- General condition not impaired
- small, white blister on the nipple
Milk congestion: causes
The mammary gland consists of several glandular lobes. This is where the milk-forming vesicles are located. The milk reaches the nipple from the vesicles through interconnected milk ducts. A milk blockage occurs when the milk ducts are blocked or cannot be completely emptied. Then the pressure rises in the milk ducts, the chest becomes tense and painful.
There are three possible reasons for this:
- lack of milk ejection reflex
- mechanical causes (mechanically caused milk congestion)
- excessive milk production
Lack of milk ejection reflex: As soon as the baby is suckling the breast, the maternal organism normally releases the hormone oxytocin, which causes the milk to flow. However, stress and physical strain can impair this so-called milk donation reflex (lactation reflex) - then the milk cannot drain away, but builds up in the milk ducts.
Mechanically caused milk congestion: In most cases, milk congestion is mechanical. Incorrect attachment or sucking of the baby as well as too short or too seldom breastfeeding times are typical mistakes when breastfeeding. They result in the breast not being completely emptied when breastfeeding. Clothes that are too tight or bras that are too small also prevent the milk from flowing out.
Excessive milk production: sometimes demand and supply do not match: the mother's breast produces more milk than the baby needs. There is also an imbalance when the child begins to sleep through the night and no longer needs a meal at night, or when a breastfeeding meal is replaced with porridge. The milk supply is then quickly greater than the actual amount consumed. This can result in a blockage of the milk.
Risk factors
Some women are more prone to breastfeeding problems and therefore have a higher risk of congestion. These include, for example, multiple mothers who are breastfeeding (twins, triplets, etc.) and women who had breast surgery before pregnancy.
Milk congestion: when do you need to see a doctor?
A visit to the gynecologist is advisable if the chest becomes increasingly painful and the affected areas are red, warm and swollen.
A visit to the doctor becomes urgent if the general condition deteriorates, chills, headache, body aches and fever (temperature> 38.4 ° C) are added. This is because these symptoms suggest that the milk blockage has developed into an inflammation of the mammary gland (mastitis).
Milk congestion: what does the doctor do?
You can first treat a blocked milk flow yourself with the help of your midwife. However, if the symptoms do not improve within 24 to 48 hours with the recommended measures, or if the symptoms even worsen, a bacterial inflammation of the mammary gland is suspected. In this case, the doctor will prescribe antibiotics.
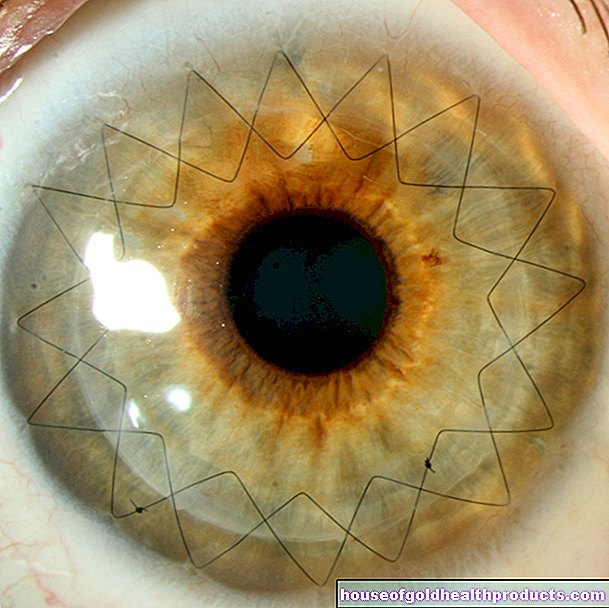
Tags: eyes symptoms alcohol drugs