Bedsores
and Sabine Schrör, medical journalistMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts
Sabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.Pressure ulcer is the medical name for a pressure sore. Colloquially, one also speaks of bedsores. The cause is constant, strong pressure that can damage the skin and the underlying tissue down to the bone. Bedridden people and wheelchair users are particularly prone to pressure ulcers. However, with careful prophylaxis, pressure ulcers can be avoided. Here you can read everything you need to know about the development, treatment, prophylaxis, diagnosis and course of pressure ulcers.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. L89
Brief overview
- What is pressure ulcer? Pressure sore that occurs particularly in places where bones are close to the surface of the skin (buttocks, elbows, heels, ankles, etc.). Mainly affected are largely immobile, bedridden patients and wheelchair users.
- Cause: persistent, strong pressure that compresses the blood vessels. Affected tissue is poorly supplied with blood, acidic metabolic products are no longer removed and gradually destroy skin, tissue and bones.
- Risk factors: Long, motionless sitting or lying down, thin, less elastic skin, diabetes, reduced sensitivity to pain, low body fat percentage, incontinence, certain medications, obesity, lack of care, malnutrition / malnutrition, existing skin diseases and irritations.
- Treatment: moist wound dressings and regular cleaning. Removal of dead tissue. If the pressure ulcer is very advanced, surgical intervention may be necessary. It is also important to eliminate the cause of the pressure sores, for example with pressure-relieving aids (anti-decubitus mattresses or seat cushions), regular repositioning, etc.
- Possible complications: The wound can become infected and lead to complications such as bone marrow and bone inflammation, pneumonia, bone abscesses or blood poisoning.
- Prophylaxis: anti-decubitus aids (foam mattresses, gel or air cushions, sheepskin pads, special seat cushions for wheelchair users, etc.), regular repositioning and mobilization of bedridden patients, frequent changes of clothes and bed linen, skin care, a balanced diet, adequate hydration, etc.
- Course and prognosis: Lengthy healing process even with optimal treatment. Increased risk of relapse after successfully treated pressure ulcers. Doctors therefore recommend careful prophylaxis and treatment of pressure sores as early as possible.
Pressure ulcers: description
A pressure sore (decubitus, decubitus ulcer) is locally limited damage to the skin, the underlying tissue and, in extreme cases, the bone. It manifests itself in the form of a wound of varying depths that is permanently open (e.g. on the buttocks, tailbone or heels). Bedridden people are particularly affected. Experts estimate that around one in ten to thirtieth hospital patients develop a pressure ulcer. In nursing homes it is even 45 percent. Wheelchair users also have an increased risk of pressure ulcers, especially in the buttocks area.
Pressure sores are very painful. They can also become infected. The first sign of this is an unpleasant, putrid smell from the wound. Pressure sores can also affect mental well-being. Because they restrict patients in their daily life. The persistent, painful wounds can even lead to depression.
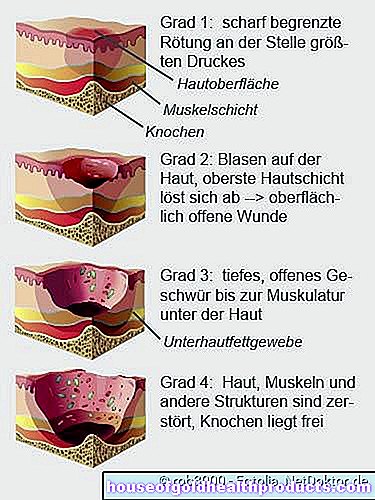
Pressure ulcers: graduation
A pressure ulcer changes the skin. Depending on how strong the changes are, a distinction is made between different degrees of severity:
- Decubitus grade 1 (stage I): In the initial phase, the affected area of the skin turns red and is sharply defined from its surroundings. The redness persists even after the pressure subsides. The area may be hardened and warmer than the surrounding skin, but the skin is still intact.
- Grade 2 pressure ulcers (stage II): Grade 2 pressure ulcers have blisters on the skin. Sometimes the top layer of skin is already peeling off. An open wound is created, but it is still superficial.
- Decubitus grade 3 (stage III): With decubitus grade 3, the pressure sore extends to the muscles under the skin. You can see a deep, open ulcer. Under the healthy skin around the edge of the pressure ulcer there are sometimes "pockets" that emanate from the ulcer.
- Pressure ulcer grade 4 (stage IV): In a stage IV pressure ulcer, exposed bones are visible. Skin, muscles, bones and other structures such as joints or tendons are destroyed.
Where pressure ulcers form particularly easily
Some parts of the body are particularly sensitive to pressure, so that pressure ulcers can develop there quickly. Areas at risk are where there are protruding bones directly under the skin without being protected by fat or muscle tissue. Examples of this are the buttocks, the large rolling hills (trochanters) on the outside of the thighs, ankles and heels.
In the supine position, pressure ulcers are most common on the buttocks, over the tailbone, and on the heels. When lying on the side, the rolling hills of the thighs and the ankles are usually affected. Decubitus ulcers rarely develop on the ears, back of the head, shoulder blades or toes.
Generally, pressure sores form less often in the side or prone position. Longer operations in the prone position are an exception, as pressure sores can develop on the knees, face (forehead and chin), toes or in the pubic bone area.
Pressure ulcers: complications
If a pressure sore is not treated quickly, it will spread to deeper tissue layers. The tissue dies (necrosis) and must be surgically removed. The wound can also become infected. If the infected ulcer already extends into the bone, the pathogens can also spread there. Inflammation of the bones (ostitis) and inflammation of the bone marrow (osteomyelitis) may develop.If the germs spread even further in the body, this can trigger pneumonia, bone abscesses or blood poisoning (sepsis).
Deficiency symptoms can also be the result of pressure ulcers if they spread over a large area on the skin. Because then the affected person permanently loses important minerals and proteins through the open wound.
Pressure ulcers: development
A pressure ulcer occurs when the tissue is permanently exposed to excessive pressure. Then the small blood vessels are compressed and the cells are no longer adequately supplied with oxygen and nutrients, so that they die.
In addition, the blood can no longer drain through the veins. As a result, acidic metabolic products collect in the tissue. In healthy people, the resulting pressure pain triggers a reflex movement that takes the pressure off the affected part of the body. The tissue is then better supplied with blood again.
This is different in older people and patients with impaired pain perception: in them, this movement reflex is often weakened. So the pressure remains and the tissue becomes acidic. As a result, the arterial blood vessels are widened to give the tissue more blood. You can tell when the skin turns red. The widened vessels release fluid and proteins to the adjacent tissue, from which water retention (edema) and bubbles form. The tissue is increasingly destroyed - a pressure ulcer has developed.
Pressure ulcers: risk factors
Various factors favor the development of pressure ulcers:
- Lying or sitting for long periods of time: Pressure ulcers mainly develop in people who lie or sit more or less motionless for a long period of time. Often the pressure sores occur in elderly patients who are bedridden due to an acute or chronic illness. Patients in wheelchairs also belong to the risk group.
- Thin, inelastic skin: The skin of older people is often dry, slack and inelastic. This makes it particularly sensitive to shear forces (shifting of the layers of tissue against each other). If the patients slide restlessly in bed, the resulting friction can seriously damage the thin skin and promote the development of pressure sores.
- Diabetes: Diabetics are particularly prone to pressure ulcers: Over time, diabetes damages the nerves, so that diabetics can no longer perceive touch, pressure and pain as well. With a corresponding delay, they register increased pressure on the skin and tissue.
- reduced sensitivity to pain
- low body fat percentage
- Incontinence: Leads to moist skin on the anus or vagina. The skin softens, which promotes pressure sores.
- certain medications, for example pain relievers
- Obesity: Increases the pressure on the skin and tissue when lying or sitting.
- Insufficient care: Long lying in diapers that have not been changed softens the skin, leads to irritation and thus promotes pressure ulcers.
- Malnutrition / malnutrition: It dries out the skin. In addition, those affected lack pressure-cushioning fat deposits. Both of these pave the way for pressure sores.
- existing skin diseases and irritations
Pressure ulcers: treatment
The earlier a pressure ulcer is detected, the better it can be treated. Basically, the therapy is divided into two areas: local and causal therapy.
Local therapy
Local therapy aims to treat the pressure sore and support it to heal. In the case of a first-degree pressure ulcer, it is usually sufficient to carefully care for the affected skin area and to relieve the pressure.
Pressure sores in advanced stages must be cleared of dead tissue (debridement). This is done either surgically with a scalpel (surgical debridement), with the help of enzymes (enzymatic debridement) or with fly larvae (biosurgical debridement, maggot therapy). The wound is then disinfected, covered with moist wound dressings and cleaned regularly.
Sometimes technical procedures such as the vacuum sealing method are also used as part of local therapy.
Causal therapy
A pressure ulcer can only be treated successfully if its cause is eliminated: the pressure. For lying patients, for example, a special bedsore mattress or a special bed is recommended. In addition, the patient should be repositioned regularly. Seat cushions are advisable for wheelchair users. You can read more about this below in the section Pressure ulcers: prophylaxis.
Proper nutrition also plays an important role: a diet high in protein, vitamins and minerals allows the skin to recover better and prevents malnutrition. Sometimes a special food is also given.
Painkillers help relieve the pain associated with pressure ulcers. In addition, special movement exercises promote blood circulation and prevent the patient from always lying on the same spot.
The effective treatment of concomitant diseases, including those of a psychological nature, is also part of causal therapy. For example, depression can threaten the success of the treatment.
Pressure ulcer: surgery
Grade 1 to 3 pressure ulcers (stages I to III) usually do not need to be surgically removed. However, it is different with pressure ulcers grade 4 (stage IV): Here, surgical intervention is almost always necessary. The surgeon cuts out the pressure sore. Sometimes part of the bone has to be removed as well.
Plastic surgery may be necessary for very large pressure sores. Then the surgeon transplants skin and soft tissue from other areas of the body onto the damaged area.
Photos can help to understand the success of the treatment. So don't be surprised if medical staff take regular photos of the wound.
Pressure ulcers: prophylaxis
Doctors and nursing staff regularly assess the individual risk of pressure ulcers in each patient. For this purpose, documentation sheets are used, for example the so-called Braden scale. Certain risk factors such as the patient's level of physical activity, mobility and ability to react to pressure-related complaints are each awarded between one and four points.
At the end of the scale, all points are added. A value of 18 points and more means no risk of pressure ulcers. The lower the number, the higher the risk. If the score is less than nine, the patient is at very high risk of developing a pressure sore.
Based on the result, individual measures for pressure ulcer prophylaxis are taken. Examples:
Anti-decubitus aids
Anti-decubitus aids reduce the pressure on vulnerable areas of the skin by distributing it more evenly. These systems have proven themselves:
- Soft storage systems such as foam mattresses, gel pads or air cushions distribute the body weight and thus the pressure over a larger area.
- Alternating pressure systems (alternating pressure mattresses) consist of differently arranged air cushions that are alternately inflated with air. Some systems are equipped with software that detects when the pressure becomes too strong at certain points. The system then automatically causes a shift by releasing the air from the corresponding chambers and filling other chambers.
- Micro-stimulation systems (MiS) are a type of electrically controlled bedsore prophylaxis mattresses. With their own small movements, they encourage the patient's own movement. This stimulates the blood circulation in the tissue, which prevents pressure sores or supports the wound healing of existing ulcers.
Sheepskins are also well suited as a pressure-relieving pad. However, they give off a lot of heat and are therefore not always perceived as pleasant.
Special anti-decubitus seat cushions are suitable for wheelchair users. These reduce the pressure on the buttocks.
Rearrangement and mobilization
Bedridden patients must be repositioned regularly - even if they are lying on an anti-decubitus mattress. In addition, the patients should be mobilized with the help of specific movement exercises. This also includes mental mobility as a central requirement for physical movement. Reading, listening to the radio, hobbies, conversations - all of these stimulate the mind and also keep the body fit.
Skin care
Careful skin care keeps the skin healthy and thus lowers the risk of pressure ulcers. Proper skin care means with a view to pressure ulcer prophylaxis:
- Wash the skin with water that is as cool as possible.
- For the most part, avoid using washing additives or prefer liquid, active washing substances.
- Use oil bath additives on very dry and chapped skin.
- Use care products adapted to the patient's skin type, such as creams and lotions (e.g. water-in-oil products for normal to dry skin; oil-in-water products for oily skin).
Right nutrition
A pressure ulcer cannot be prevented through diet, but the risk of developing it can be reduced. Experts recommend a wholesome, varied diet. In the case of existing pressure sores, sufficient vitamins and minerals must be supplied to promote wound healing. In addition, patients at risk should drink plenty to avoid drying out the skin.
Further measures
The following measures also help to reduce the risk of pressure ulcers:
- Frequent changes of clothes and bed linen in patients who sweat profusely or are incontinent. This prevents the skin from becoming soft due to moisture.
- Use breathable incontinence garments
- Place buttons and seams on bedding and bed linen in such a way that they do not press on the vulnerable areas of skin
- Therapy of underlying and concomitant diseases (diabetes, depression, etc.)
Those who care for bedridden relatives at home can learn how pressure ulcers can be effectively prevented in special courses on pressure ulcer prophylaxis. The course content includes information about suitable positioning and repositioning techniques as well as tips for suitable aids and care measures.
Pressure ulcers: examinations and diagnosis
A pressure ulcer can be seen with the naked eye. For this reason, the areas of the body that are particularly susceptible to pressure ulcers should be regularly inspected in people at risk. If possible, you should show the patient how they can examine their skin themselves. For example, you can look at your own buttocks with the help of a mirror. The partner or friends can also be involved in order to regularly examine the relevant parts of the body. In clinics and nursing homes, the nursing staff carry out this important task.
Finger test
A pressure ulcer can be identified at an early stage with the so-called finger test. To do this, press the already reddened, suspicious skin area with your finger. If the skin is not noticeably paler immediately after letting go, it is already a stage I (grade 1) pressure sore.
Smear, blood sample, x-ray
In order to be able to detect an infection in the wound, the doctor usually takes a tissue sample from the affected area. It is examined for germs in the laboratory. Fever, chills, and an unpleasant, putrid smell from the wound can also indicate an infection. In addition, the patient's blood can be examined for pathogens.
If the pressure ulcer is very advanced, an X-ray is also advisable. This can be used to determine whether the pressure ulcer has already penetrated the bone.
Pressure ulcers: disease course and prognosis
How long it takes for a patient to develop a pressure ulcer depends on many factors. In addition to the patient's age, nutritional status and the cause of being bedridden also play a major role. Some people develop a pressure ulcer within a few hours. This can happen if the skin has been damaged by other diseases or if the metabolism is disturbed (for example in the case of diabetes).
An advanced pressure ulcer heals only slowly, even with optimal treatment. Sometimes it takes months for the pressure sore to go away completely. That is why it is so important to pay attention to careful pressure ulcer prophylaxis and to react quickly in an emergency.
But even after a pressure sore has healed, patients have an increased risk of developing another pressure ulcer in the affected area (relapse). Therefore, you should check the affected area of skin particularly intensively and carefully protect it from pressure. This prevents another pressure ulcer from forming.
Additional information
Guidelines:
- Guideline "Cross-sectional specific pressure ulcer treatment and prevention" of the German-speaking Medical Society for Paraplegia e.V.
- Guideline "Prevention and Treatment of Pressure Ulcers" of the National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance