Epididymitis
Clemens Gödel is a freelancer for the medical team.
More about the experts All content is checked by medical journalists.Inflammation of the epididymis (epididymitis) is a painful inflammation of the epididymis. It absolutely needs to be treated. Postponed inflammation can lead to infertility. The treatment of epididymitis, which usually lasts several weeks, includes bed rest, painkillers and possibly antibiotics. Read everything you need to know about the symptoms, diagnosis and treatment of epididymis here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. N45
Epididymis: description
Inflammation of the epididymis (epididymitis) occurs in most cases as a side effect of bacterial inflammation of the prostate or urinary tract. It rarely occurs in isolation as the sole inflammation of the epididymis, as the pathogens spread along the spermatic duct. Epididymitis usually only occurs after puberty.
The epididymis can be acute or chronic.
Testicles and epididymides
The epididymis, like the penis and testicles, is one of the male's external sexual organs. The testicles and epididymis are located together in the scrotum (scrotum). The testes produce semen and sex hormones. At the upper pole of the testicle, the fresh semen is passed into the epididymis and stored there. The spermatic duct emerges from the epididymis and then flows into the urethra in the area of the prostate gland.
Although the testes and epididymis are close together and closely connected, inflammation of the testicles (orchitis) is not the same as inflammation of the epididymis (epididymitis). The latter is much more common. However, in some cases, the inflammation affects both testicles and epididymis. In this case it is called epididymorchitis.
Epididymitis: symptoms
The symptoms of epididymitis are similar to those of testicular inflammation (orchitis): Usually a painful, sometimes palpable swelling of the scrotum occurs relatively suddenly, which doctors call "acute scrotum". The surrounding skin shows typical signs of inflammation such as overheating and reddening. The epididymal pain can radiate to the groin and lower abdomen. Concomitant symptoms include fever of up to 40 ° C as well as vomiting and nausea.
Chronic epididymitis can also be characterized by painless swelling. The epididymitis caused by chlamydia can be relatively asymptomatic.
Epididymitis: causes and risk factors
The most common causes of epididymitis include bacterial inflammation of the urinary tract and the prostate. As a rule, the pathogens get from the urethra or the prostate via the spermatic duct to the epididymis. One then speaks of an "ascending (ascending) infection".
Men with voiding disorders of the urinary bladder, malformations in the urogenital area and a permanent urinary catheter therefore have a particularly high risk of developing the disease. In children, malformations of the lower urinary tract are primarily responsible for the bacteria getting into the epididymis in the first place. In some cases, testicular torsion, that is, twisting of the testicles, leads to inflammation of the epididymis. In many cases, however, the epididymis is not inflamed in isolation, but rather together with the neighboring sections of the seminal and urinary tract.
Which pathogens trigger the inflammation?
Testicular inflammation is usually triggered by viruses - but not epididymitis. The cause here are usually bacteria. In sexually active men under 35, it is often Chlamydia trachomatis (more rarely Neisseria gonorrhea). In men over 35 years of age, intestinal bacteria such as Escherichia coli, enterococci, Klebsiella or Pseudomonas aeruginosa as well as staphylococci are responsible for epididymitis.
Epididymitis occurs more rarely as a result of the spread of bacteria via the bloodstream (especially pneumococci and meningococci), as part of a tuberculosis disease or as a result of trauma: if urine flows into the seminal tract, it can cause chemical irritation of the epididymis, which also happens causes an inflammatory process.
Other possible causes
The less common viral inflammation of the epididymis is usually caused by the mumps virus. In this case, the testicle is often also affected, whereby the epididymis can precede the testicular inflammation. Before puberty, adenoviruses and enteroviruses can also trigger a so-called post-infectious epididymitis that begins after infection.
Autoimmune processes are also a possible cause of epididymitis.
Fungi (Candida, Coccoidioides, Histoplasma etc.) and worms (Schistosoma, Wucherichia or Echinococcus) are rare causes of epididymitis in Germany.
In addition, there have been isolated descriptions of epididymitis caused by drugs such as amiodarone (used to treat cardiac arrhythmias).
Epididymis: examinations and diagnosis
If epididymitis is suspected, you should contact a urologist. The doctor will first talk to you in detail about your symptoms and any underlying illnesses (anamnesis. Possible questions are, for example:
- How long have the complaints existed?
- Did the symptoms start suddenly?
- Do you have penile discharge or painful urination?
- Are you already familiar with diseases of the urinary tract (including urinary tract infections)?
- Do you have sexual intercourse?
Epididymis: Physical Exam
This is followed by the physical examination. The doctor will first examine the scrotum for recognizable signs of inflammation (overheating, reddening) and check whether the epididymis is swollen.
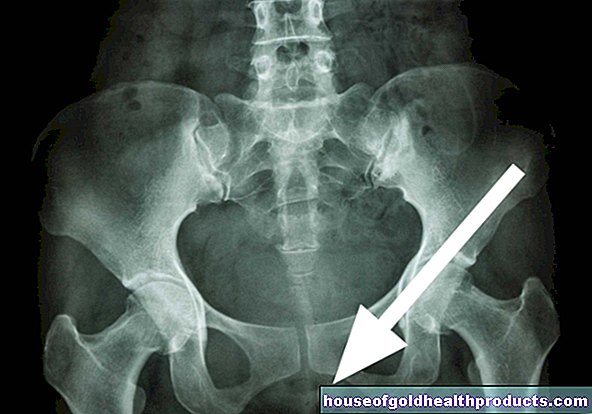
Then the doctor lifts the scrotum. If the symptoms are reduced as a result (Prehn's sign positive), this speaks for epididymitis. In the case of testicular inflammation and testicular torsion (twisting of the testicle around its own axis), on the other hand, the symptoms are not improved by lifting the scrotum. This distinction is very important because testicular torsion is an emergency that must be operated on within a few hours. With testicular torsion, however, inflammation of the epididymis can also occur as a side effect. So if testicular torsion cannot be ruled out in the examination, surgical exposure of the testicle is necessary. If an abscess (encapsulated collection of pus) has already formed in the area of the epididymis, it can be felt as a fluctuating swelling.
Epididymis: laboratory tests
The doctor will also ask for a urine sample. On the one hand, you can quickly confirm the suspicion of a urinary tract infection with so-called "urine stix" and, on the other hand, create so-called urine cultures. The latter should help to determine the causative pathogen and its sensitivity to certain antibiotics (resistogram). In addition, if epididymitis is suspected, a swab of the urethral entrance can be taken and examined in the laboratory.
In the case of epididymitis, the blood test shows typical signs of inflammation (such as an increased number of white blood cells). If a mumps virus infection is suspected, antibodies in the blood can be determined.
Epididymis: imaging tests
If epididymitis is suspected, an ultrasound examination of the testicles (testicular ultrasound) is particularly important for diagnosis. It can be repeated at any time and is completely safe. This is why sonography is also ideal for assessing the course of the disease. The urologist uses the ultrasound image to identify the extent of the inflammation and whether the process has already spread to the neighboring testicles. The beginning of an abscess formation can also be recognized in good time.
If there is a suspicion of an obstruction of the drainage in the urinary system, which presses the urine into the spermatic duct and testicles, ultrasound examinations and possibly also X-ray examinations of the urinary tract with a contrast medium (urography) are carried out. For example, constrictions in the urethra (urethral strictures) can be identified. If necessary, a measurement of the urine stream or a cystoscopy may also be necessary.
Epididymis: treatment
Epididymitis therapy consists of bed rest, pain relievers and, if necessary, antibiotics. It is important to elevate the testicles and cool them with cold compresses. The acute inflammation can last eight to ten days. The healing process is characterized by the fact that the temperature normalizes, the pain disappears and the epididymis slowly swells. Only then is the patient allowed to get up. He is given a jockstrap (a bag-shaped bandage to protect the testicles) so that the epididymis and testicles cannot sink.
If the pain is severe, the spermatic cord can be infiltrated with local anesthetics. There is an increased risk of thrombosis during bed rest. To prevent blood clots, the patient may therefore be given an injection of anticoagulant heparin.
In children, a malformation of the urinary tract that obstructs the flow of urine usually leads to epididymitis. The urine is then often temporarily drained from the bladder (puncture cystostomy) in order to speed up healing.Surgical correction of the malformation may be necessary following treatment of the epididymis.
If an abscess (encapsulated collection of pus) forms as a result of epididymitis, it must be surgically opened and removed.
If an infection with chlamydia was the trigger for epididymitis, all sexual partners should always be treated as well. Otherwise, new infections (re-infections) are possible again and again.
In the case of a chronic course, the treatment lasts longer (especially the administration of antibiotics). In severe cases, the epididymis must be surgically removed (epididymectomy) or the spermatic cord severed (vasectomy).
If the seminal ducts stick together due to inflammation (occlusive azoospermia), this can be remedied with microsurgical techniques after the inflammation has subsided: As part of the so-called epididymovasostomy, a continuous path for the sperm is created again.
Epididymis: disease course and prognosis
The treatment of epididymis requires a lot of patience: the healing process can take up to six weeks - even with optimal treatment. Only then does the scrotum feel normal again in many men.
Usually epididymitis heals well. However, complications are also possible, such as fistulas, local destruction of the epididymal tissue and the propagation of the inflammation along the seminal and urinary tract. Occasionally, the focus of inflammation (abscess) is encapsulated in a pronounced epididymis. It then has to be cleared out operationally.
Frequent or protracted epididymis can lead to scarring and constrictions in the epididymis or vas deferens. This can hinder the transport of the sperm, which leads to infertility, especially in the case of bilateral occlusion (occlusive azoospermia). In addition, the inflammation can spread to the neighboring testicles, among other things.
In the case of recurrent epididymitis, surgical severing of the spermatic cord (vasectomy) or removal of the epididymis (epididymectomy) often helps. In the advanced stages of the inflammation, the testicles may also have to be removed.
In addition to blood poisoning (sepsis), the so-called Fournier gangrene is a dreaded complication if the epididymis is very severe when the immune system is weakened. This leads to tissue death (necrosis) of connective tissue strands in the testes, which can lead to a severe inflammatory reaction of the entire organism with a high mortality rate.
Tags: toadstool poison plants parasites organ systems