Genital herpes
Marian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the experts All content is checked by medical journalists.Genital herpes is a sexually transmitted disease and is caused by viruses. After infection with herpes in the genital area, the outbreak cannot be prevented, but the severity and duration of the symptoms can be reduced. Read the most important information about genital herpes here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. A60
Genital herpes: description
"Herpes on the penis", "vaginal herpes", "intimate herpes" - all these terms are summarized under genital herpes, the infestation of the genital area with herpes.
How does genital herpes come about? - Trigger and transmission route
Genital herpes is triggered by herpes simplex viruses (HSV), which are divided into type 1 (HSV1) and type 2 (HSV2). Type 2 is responsible for 70 to 80 percent of cases, the rest is triggered by type 1.
Typically, genital herpes infection with type 2 occurs as a smear infection through unprotected sexual intercourse. Body fluid infected with the virus passes directly or indirectly from one person to the next. The herpes viruses find their way into the body through minimal damage to the mucous membrane. After the facial region, the penis and vagina are the preferred sites of infection for the herpes simplex viruses.
Type 1 herpes in the genital area comes about through the transmission of cold sores to the genital region. This usually happens through oral sex or through infection from hands contaminated with viruses.
Indirect genital herpes infection through infected objects is also possible. This is because the viruses survive outside the human body for up to 48 hours. Used condoms or worn underwear therefore always carry a risk of infection.
During pregnancy and childbirth, the herpes virus can be transmitted from mother to child and cause serious complications, including miscarriage.
Once genital herpes, always genital herpes? - Primary infection and reactivation
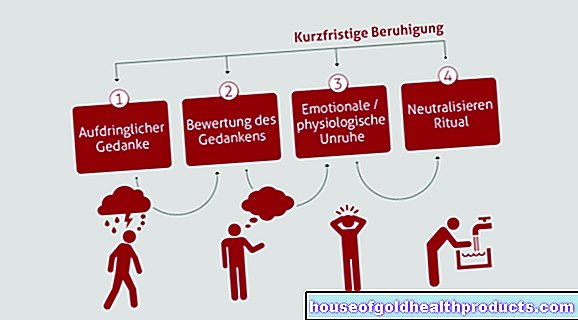
Herpes viruses remain in the body for life after being infected for the first time, the so-called primary infection. First, the viruses enter the organism via the smallest cracks in the skin and mucous membranes and multiply there in superficial skin cells, so-called epithelial cells, with the typical symptoms.
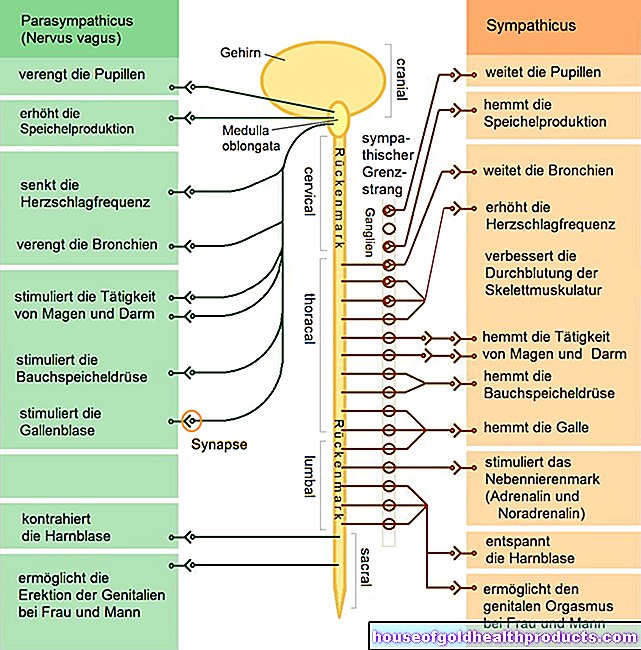
After a while the symptoms disappear, but the herpes viruses are not completely destroyed by the body's own defenses. Some of the pathogens migrate along the nerve pathways to the nerve roots (retrograde axonal transport). There the viruses switch to a kind of sleep mode and escape the access of the immune system. In this state, also known as latency, the herpes viruses survive a lifetime.
The reactivation
From time to time the viruses become active again and migrate back to the epithelial cells of the skin. There they cause a new outbreak of genital herpes. This phenomenon is known as reactivation (or recurrent infection) and occurs especially when the immune system is weakened.
Typical triggers for reactivation are colds, psychological or physical stress or intense physical exertion.
Other risk factors for reactivation of genital herpes are skin injuries or infections of the penis or vagina. Herpes viruses can penetrate the body particularly well here. High UV radiation can also reactivate genital herpes.
Certain medications, hormonal changes and diseases that are associated with an immune deficiency (for example AIDS) can also promote the occurrence of genital herpes.
The frequency of outbreaks varies from person to person and decreases with age. In principle, reactivations occur more frequently after an infection with HSV2 than after an infection with HSV1.
When is genital herpes contagious?
Affected people are always contagious when the body excretes viruses. The more, the greater the risk of infection. As long as the viruses are in a dormant state, infection is not possible, but only during the primary infection and subsequent reactivations, when the typical vesicles appear.
In the case of so-called "latent infections", there are few or no symptoms vaginally or on the penis, but viruses are nevertheless excreted. The risk of infection is particularly high here because those affected cannot take any precautions.
Who does genital herpes affect?
Infection with the HSV2-caused genital herpes usually only takes place from the beginning of sexual activity. According to a study by the Robert Koch Institute, between twelve and 16 percent of the total population in Germany are infected with HSV2. Women are more likely to be affected than men because women are more likely to be infected during sexual intercourse.
Genital herpes: symptoms and complications
After an initial infection with genital herpes, the typical early symptoms only appear after two to twelve days (incubation period). The vagina and penis are red and swollen. Those affected often feel an uncomfortable tingling and itching sensation or a stinging, burning sensation. In addition, the lymph nodes in the groin often swell.
Sometimes after a few hours, but often only after a few days, small, painful blisters appear. These are filled with a transparent to purulent-cloudy liquid that contains a lot of viruses and is highly contagious. The vesicles and gradually burst open.
This results in skin damage (erosions), occasionally even small, painful ulcers (ulcerations), which are often covered by a thin crust. In addition, pain can occur when urinating (dysuria), as well as inflammation of the entire glans (balanitis) or vagina (vulvovaginits). When the blisters and skin damage have completely disappeared, the genital herpes has healed.
The symptoms vary from person to person. In principle, primary infections are usually more violent than reactivations. The patients then suffer from general symptoms such as fever, headache and body aches. But some show only very mild symptoms or no symptoms at all.
If those affected are already infected with HSV1, an HSV2 infection is often less pronounced because the two types of virus are very similar and the immune system is already adapted.
Vaginal herpes is usually accompanied by a glassy discharge, which in herpes on the penis is much less pronounced or is completely absent.
Genital herpes complications
As a rule, the symptoms only affect the genital parts of the genital herpes: vagina and vulva in women, the penis in men. Occasionally larger areas are also affected.
Genital herpes can spread over the buttocks to the thighs or around the anus. Other modes of transmission are also possible through sexual practices. Genital herpes can even develop in the area of the fingers.
People who suffer from active genital herpes are at greater risk of contracting other sexually transmitted diseases through unprotected sex. Herpes weakens your immune system and makes your body more vulnerable. Conversely, patients with HIV, for example, are often infected with genital herpes.
Genital herpes: duration
The time course of the disease depends on many individual factors. The duration of the illness ranges from a few days to four weeks. As a rule, genital herpes is over after two to three weeks.
Genital herpes: diagnosis
Genital herpes usually has a typical appearance, but other diseases also have similar symptoms. A mere visual diagnosis by the doctor is usually not enough for a first-time infection. Additional laboratory tests confirm the suspicion.
In addition to special antibody tests (antibody detection), the smallest virus components (antigen detection) or their genetic information can be detected in the laboratory. Finally, the herpes viruses can also be cultivated and precisely determined.
Genital herpes: what helps?
Certain so-called antiviral drugs are used for genital herpes treatment. They work very similarly, are given in tablet form or, in more severe cases, injected directly. These drugs shorten the duration of the illness and reduce symptoms.
Genital herpes: disease course and preventive measures
Most genital herpes is harmless and without further complications. However, it is always advisable to consult a doctor, especially with initial infections, as a diagnosis should first be confirmed. In addition, only the doctor can prescribe the necessary drugs for the treatment of genital herpes.
As with all sexually transmitted diseases, sexual partners should also be examined and treated if necessary. The risk of infection can be significantly reduced with protected sexual intercourse, although transmission of genital herpes cannot be completely ruled out even with a condom. During an active outbreak of genital herpes, it is best for those affected to avoid sexual intercourse altogether.
Avoiding stress of any kind and supporting the immune system through a healthy diet, adequate sleep and regular exercise is helpful. Because healthy defenses are the best protection against frequent outbreaks of genital herpes.
Tags: menopause smoking skin