Obsessive-compulsive disorder
Updated onJulia Dobmeier is currently completing her master's degree in clinical psychology. Since the beginning of her studies, she has been particularly interested in the treatment and research of mental illnesses. In doing so, they are particularly motivated by the idea of enabling those affected to enjoy a higher quality of life by conveying knowledge in a way that is easy to understand.
More about the experts All content is checked by medical journalists.Obsessive-compulsive disorder is a serious mental illness. Those affected compulsively perform the same rituals over and over again or are plagued by disturbing thoughts that they cannot escape. Although they realize that their actions and fears are irrational, they cannot control their thoughts and actions. Read here how to recognize obsessive-compulsive disorder, how it develops and is treated.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. F42

Obsessive-Compulsive Disorder: Description
Obsessive compulsive disorder (OCD) is a serious mental disorder that puts a lot of stress on those affected.
Obsessive-compulsive disorder encompasses a wide range of behavioral and other psychological characteristics. Obsessive-compulsive thoughts haunt some people. For example, they have the compulsive idea of having to commit an act of violence or sexually undesirable behavior. Other people affected are under pressure to have to perform certain acts again and again in a ritualized form (e.g. washing hands, counting cars passing by).
The thoughts and actions are called coercion, because those affected often try unsuccessfully to fight them. The inner resistance to refraining from actions or thoughts costs a lot of strength and creates ever increasing tension and fear. Only when they give in to the constraints does the pressure ease. Similar to addicts, a kind of habituation effect occurs over time: the ritual usually becomes more and more complex and protracted until it brings the desired relaxation. The constraints therefore take up more and more time and energy.
Obsessive-compulsive disorder is an outdated term for obsessive-compulsive disorder. The obsessional neurosis definition implies that obsessive-compulsive people - in contrast to people with a psychosis - do not lose touch with reality. They know that their obsessional thoughts and actions are irrational, but they still cannot turn them off.
A bit of coercion is normal
There is a bit of compulsiveness in everyone - superstitious ideas are just as much a part of it as harmless rituals. Some otherwise rational people feel a little uneasy when they are supposed to sign an important contract on Friday the 13th.
The transition from normal behavior to OCD is fluid. For example, some people may just feel compelled to double-check that the stove is switched off before going to bed - even if they haven't cooked at all. Others, on the other hand, have to perform a washing ritual lasting several hours before they can leave the house.
Basically, obsessive-compulsive disorder only exists if the person concerned suffers from it himself or is massively restricted in his everyday life.
How many are affected?
People who suffer from obsessive-compulsive disorder are often ashamed of their irrational behavior and keep silent about it whenever possible. The number of unreported cases is therefore high. Experts estimate that about one to three percent of the population will experience OCD at some point in their lives.Men are more likely to have control compulsions, whereas women are more likely to suffer from washing or cleaning compulsions.
In addition to obsessive-compulsive disorder, those affected usually experience other psychological disorders such as depression or anxiety disorders.
Compulsory washing
You can find more information on the signs and treatment of compulsory washing in the article Compulsory washing.
Compulsion to control
You can find out how compulsory control expresses itself and how it is treated in the article compulsory control.
Compulsions in children
Obsessive-compulsive disorder often begins in childhood or adolescence. Around half of those affected show the first symptoms of obsessive-compulsive disorder before the age of 15. Children and adolescents often try to keep these constraints a secret. Boys are more often affected than girls. The compulsions often manifest themselves massively in life crises or conflict situations.
Obsessive-compulsive disorder in children, like adults, is treated with cognitive behavioral therapy. If the compulsions are strong, drugs, especially selective serotonin reuptake inhibitors (e.g. fluoxetine), can also be used in children.
Obsessive-compulsive disorder: symptoms
The main characteristic of obsessive-compulsive disorder is having recurring obsessions or compulsions. Often these symptoms also occur together. The obsessions and compulsive actions create a strong internal tension and are mostly associated with fear.
Compulsions
Compulsive acts are irrational acts carried out by those affected. Often it is about averting a possible disaster. The content of the actions does not have to be rationally related to the fears. For example, a mother may fear that something bad will happen to her children if she forgets to turn off the lights. So, fearing for her children, she constantly checks the light switches.
Frequent forms of compulsive behavior are, for example, compulsory cleaning and compulsory order. When cleaning is compulsory, those affected have to clean the apartment or objects again and again. Order constraints go hand in hand with an obsessive desire for uniformity and symmetry. Perhaps the pens on the desk have to be aligned exactly parallel or all shirts have to be folded to exactly the same size. Deviating from this requirement is unbearable for those affected.
Many also suffer from compulsive counting and repetition, in which they feel compelled to perform certain actions a certain frequency. If those affected make a mistake in their rituals or have the impression that they were not thorough enough, they have to start all over again. Due to the increasing complexity of the rituals, an obsession can take several hours to complete.
Whether it is an obsessive thought or a compulsive act - those affected are well aware of the absurdity of their thinking and behavior and they are ashamed of it. You try again and again to oppose the coercion with resistance, but this only succeeds for a short time and with great exertion of force.
Obsessive thoughts
Obsessive thoughts are expressed in the form of intrusive ideas, conceptions or impulses. They often have violent, sexual or blasphemous content. For more information on signs and treatment for obsessive-compulsive thinking, see the Obsessive-Compulsive Thinking post.
Obsessive-compulsive disorder: causes and risk factors
How obsessive-compulsive disorder develops is not yet clear. Family examinations and twin studies show that - as with most mental illnesses - there is a hereditary predisposition to the obsessive-compulsive disorder. For it to break out, however, other factors must be added.
These include, for example, experiences in childhood that have led to a person being more insecure and having a stronger need for control. Obsessive-compulsive disorder is often preceded by a particularly stressful experience or life crisis. With the help of the compulsory ritual, the person concerned regains the lost feeling of security - the external insecurity is balanced out by an internal structure. But this security is deceptive: If the compulsory ritual is not carried out, fear comes back with power. In the long run, it gets worse, which makes OCD worse - a vicious circle.
Changes in the brain
It is now known that the frontal lobes of the brain are overactive in people with obsessive-compulsive disorder. Among other things, he controls the so-called basal ganglia. These are brain structures that are responsible for motor processes. This hypothesis is supported by the fact that people whose basal ganglia are affected by tumors or head injuries often develop obsessive-compulsive disorder.
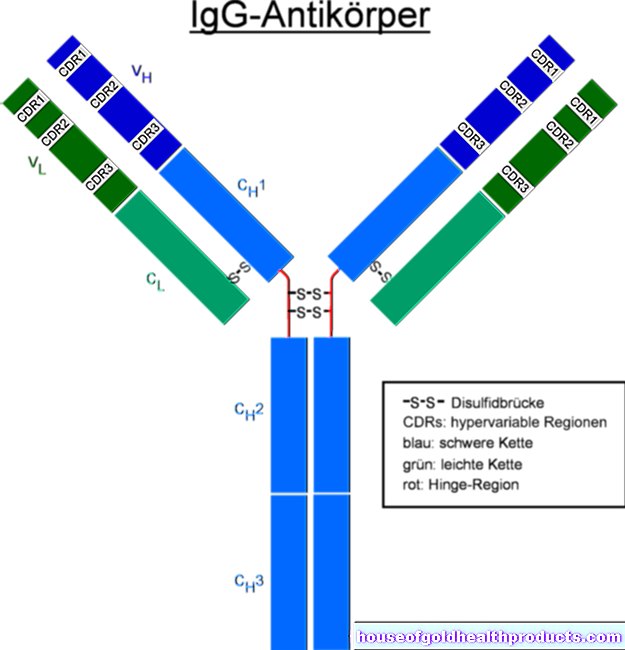
In addition, the serotonin levels in the brain appear to be disturbed in people with obsessive-compulsive disorder. Serotonin is an important neurotransmitter. Many patients are helped by drugs that increase serotonin levels.
Environmental influences
In the interplay with one's own personality and biological conditions, upbringing can also contribute to the development of obsessive-compulsive disorder. Children who tend to be anxious are made more insecure by their parents' overprotective behavior. They learn from their parents to avoid threatening situations instead of facing them. Parents who are very critical of their children or who have perfectionist demands can also promote obsessive-compulsive disorder in their offspring.
Obsessive-compulsive disorder triggers, as mentioned above, are often stressful events. Any overstrain creates the desire for control. However, when the person is unable to cope with the situation, obsessions and compulsions serve as a distraction. On the other hand, obsessive thoughts and actions give people who are anxious and have an increased need for security the illusion of being able to control events that are basically uncontrollable. For example, they hope to be able to avert accidents through certain rituals.
Obsessive Compulsive Disorder: Investigations and Diagnosis
Those affected are often ashamed of their compulsions because they see them as nonsensical. They find it difficult to confide in a psychologist or doctor. People should be aware, however, that the strange thoughts and actions are part of an obsessive-compulsive disorder and that many people struggle with the same or similar compulsions. Above all, compulsions usually don't go away on their own. It is therefore important to answer the doctor or psychologist openly and honestly so that they can recognize and treat the OCD.
Diagnostic criteria
For the diagnosis of obsessive-compulsive disorder, the therapist uses the ICD-10 classification of mental disorders. The following criteria must apply:
1. Those affected have obsessions and / or compulsions most days for a period of at least two weeks.
2. The obsessive thoughts and actions exhibit the following characteristics:
- Those affected know that the thoughts / actions are their own and are not generated by outside influences.
- The thoughts / actions repeat themselves continuously, are perceived as unpleasant and recognized as exaggerated or nonsensical.
- People try to resist the obsessive thoughts or actions.
- Those affected find the execution of obsessive thoughts or actions uncomfortable.
- Those affected suffer from obsessive-compulsive disorder and the enormous amount of time it takes limits them in their professional and social lives.
anamnese
In an initial interview (anamnesis), the doctor or therapist will ask questions to determine whether the criteria mentioned apply to the person. The obsessive-compulsive disorder expert might ask the following questions:
- Do you often have unpleasant thoughts that arise?
- Do you feel an inner pressure to carry out certain actions over and over again?
- Do you find these thoughts or actions nonsensical?
- Do you fear that if you don't perform the actions, something bad could happen?
- Do you need a very long time for everyday activities?
Obsessive-Compulsive Disorder: Treatment
Cognitive behavioral therapy shows the best treatment success. In addition, medication can be helpful.
Cognitive behavioral therapy
At the beginning the therapist discusses the concrete procedure with the patient. One method in cognitive behavioral therapy is exposure exercises, which are considered to be particularly effective. During these exercises, the patient is confronted with the stimulus that normally triggers his compulsive behavior without being allowed to give in to internal pressure. Someone who has an obligation to order, for example, has to bring clutter into their closet and then not sort the clothes again. The exposure can take place in such a way that the challenges are increased from time to time or the person concerned is confronted with his greatest fear right at the beginning of the therapy.
While the urge to follow the usual ritual seems overwhelming at first, the patient experiences how the pressure slowly eases - even without giving in to the pressure. Through this conscious experience, he regains control over his behavior to a certain extent. At the beginning of obsessive-compulsive disorder therapy, however, it can take several hours for this effect to set in.
In order to cope with obsessive-compulsive thoughts, the patient is asked to allow the unpleasant thoughts to occur. Because the suppression means that these occur even more frequently. If those affected get involved and deal directly with the thoughts, they can overcome their compulsions.
In addition, the behavior therapist explains to the patient how compulsions arise and helps him to change unfavorable thought patterns.
Methods to reduce stress such as autogenic training, progressive muscle relaxation or mindfulness training also have a supportive effect.
Obsessive Compulsive Disorder: Medication
So-called Selective Serotonin Reuptake Inhibitors (SSRI) - a special group of antidepressants - help a large proportion of the OCD. As a rule, they have to be dosed significantly higher than in the treatment of depression. Taking SSRIs reduces internal tension in most people. The obsessive-compulsive symptoms subside. However, they usually do not go away completely and return more often after stopping the medication. Accompanying cognitive behavioral therapy is therefore always recommended.
Tips for relatives
Obsessive-compulsive disorder is a burden not only for the patient but also for everyone who lives with them. The time-consuming compulsions are also at the expense of the partner and family. Sometimes they are even asked to submit to the coercion, for example by observing excessive hygiene rules themselves.
The following tips can help relatives to cope with the difficult situation:
- The patient can only control the compulsory ritual to a limited extent and with great effort. The request to pull yourself together, as well as discussions about the pointlessness of doing, therefore do not help. The only thing that really helps is therapy.
- Therefore, encourage the person affected to seek therapeutic help.
- Do not support the victim in his ritual. For example, don't help him check all electrical appliances or count things for him to calm him down before leaving the house. In the long run, you only stabilize the compulsive behavior.
- Praise them for progress, but don't criticize them if the symptoms get worse again - for example, if the person is under pressure. Such fluctuations in the severity of symptoms are normal.
- Do not allow yourself to be overwhelmed by the compulsion of the person concerned. Continue to pursue your hobbies, meet friends and try to do something with the obsessive-compulsive disorder as well as he can.
- Set clear boundaries for what you are willing to accept and what not.
- If you feel exasperated and angry at times (and this is inevitable!), Make it clear that this relates to the symptoms, not the person with the disease.
Obsessive-compulsive disorder: disease course and prognosis
Obsessive-compulsive disorder is usually chronic. Symptoms worsen under stress.
In the past, obsessive-compulsive disorder was thought to be hardly treatable. With today's methods of psychotherapy and certain medications, however, the symptoms can usually be reduced to a tolerable level. The following applies: the earlier the therapy starts, the better the prognosis. However, those affected who also suffer from depression have poorer prospects.
Long-term studies have shown that the condition of about two thirds of the patients treated has improved or very much improved two to six years after the end of therapy compared to before. However, a complete cure for OCD is very rare.
Tags: laboratory values alcohol anatomy