Anal fissure
and Carola Felchner, science journalistDr. med. Mira Seidel is a freelance writer for the medical team.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.An anal fissure is a painful, elongated tear in the anal lining. It is often caused by pressing too hard on hard stools. A typical sign of an anal fissure is sharp pain during bowel movements. In most cases, it is an acute anal fissure that can be treated with ointments and stool-regulating measures. If the condition is chronic, surgery may be necessary. Find out what causes an anal fissure, how to treat it, and what effective prevention looks like here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K60

Brief overview
- What is an anal fissure? Painful tear in the mucous membrane of the anal canal
- Symptoms: pain during and after bowel movements, spasms of the anal sphincter, itching, bleeding, oozing or secretion of mucus from the wound, possibly thickening of the skin
- Causes: often strong pressing during bowel movements or stool that is too hard, possibly also anal sexual practices, hemorrhoids, diarrhea, chronic inflammatory bowel diseases (Crohn's disease, ulcerative colitis)
- Diagnosis: conversation, physical examination, if necessary rectoscopy
- Treatment: conservative with ointments, creams, baths; in the case of a chronic course, surgery
- Attending physician: proctologist, gastroenterologist
- Prognosis: An anal fissure is easily treatable, but can occur again and again with persistent hard faeces or other risk factors.
Anal fissure: symptoms
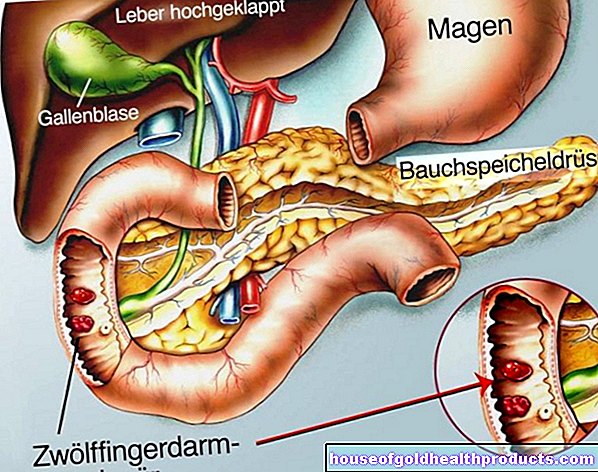
The anal fissure (Latin: fissura, "crack") is a longitudinal tear in the fine skin or the mucous membrane at the mouth of the anal canal (anoderm). There are many sensitive nerve endings there. An injury in this area is correspondingly painful.
This happens with an anal fissure
An acute anal fissure lasts for a maximum of four to six weeks. It is noticeable by a stabbing pain in the anus that occurs when the skin tears. As a result, stool can only be excreted with pain (painful defecation). To avoid this pain, many people hold back their stool (stool retention). A vicious circle, because the manure that is held back thickens and becomes even harder. Ultimately, this makes going to the toilet even more painful. Typically, the symptoms persist in the form of constant burning pain even after visiting the toilet.
Problematic: The pain can cause the sphincter muscle to cramp so much that the symptoms continue to worsen. The tissue may no longer be supplied with blood, making the anal fissure more difficult to heal. There is a risk that the acute tear could develop into a chronic anal fissure.
In addition, the spasms of the sphincter may cause further tears in the mucous membrane. Because muscle spasms like this make you push harder when defecating.
If the tear extends deep into the inner sphincter muscle, the strong cramping of the connective tissue around the muscle can increase and harden over time (fibrosis). Such a thickening of the skin can form with a chronic anal fissure. It is called the outpost fold.
Other possible symptoms of an anal fissure include:
- Chronic constipation caused by pain, when people hold back their stool for fear of pain
- Itching of the anus
- the wound may ooze or shed mucus (mucus secretion)
- light red blood deposits on the stool and blood residue on the toilet paper
Blood in the stool should always be checked by a doctor. In addition to an anal fissure, there can also be a more serious cause (such as cancer) behind it.
Anal fissure: causes and risk factors
It is often not possible to clearly explain why an anal fissure occurs. What is certain is that it can occur at any age. However, it often does so between the ages of 30 and 40. Usually an anal fissure develops in the direction of the rump.
The most common cause of an anal fissure is too much straining when defecating, coupled with too hard a stool. Both of these stretch the mucous membrane, which can easily tear. Stool that is too hard is the result of chronic constipation, for example. This in turn can be caused by insufficient fluid intake, a low-fiber diet, lack of exercise and a "sluggish bowel".
In some cases, anal sexual practices that damage the mucous membrane are the cause of an anal fissure. Hemorrhoids, inflammation in the rectum (cryptitis) and long-lasting diarrhea are also possible triggers. Patients with inflammatory bowel disease such as Crohn's disease or ulcerative colitis are also prone to anal fissures.
An anal fissure that occurs as a result of another condition (such as Crohn's disease) is called a secondary anal fissure. In contrast to this, a primary anal fissure is an independent disease (e.g. as a result of excessive pressure when defecating).
Anal fissure: examinations and diagnosis
If an anal fissure does not heal on its own within a few days, you should definitely consult a doctor. The right contact person is a specialist in diseases of the rectum (proctologist) or a specialist in diseases of the gastrointestinal tract (gastroenterologist). You can, however, first go to your family doctor, who will then refer you to others.
Most of those affected are embarrassed by their problem. They shy away from going to the doctor and prefer to try to get their symptoms under control with home remedies. Often they only seek help when the suffering becomes too great due to constant itching, burning, pain and blood loss.
If there is a wound in the anus area (such as an anal fissure), the risk of infection is very high. A lot of germs cavort here. If you wait too long to see a doctor, you run the risk of infection with potentially serious complications.
Patient discussion
The doctor first asks about the medical history (anamnesis). He asks the patient in detail about his complaints. Possible questions are:
- In what situations does the pain occur? Only when defecating?
- Do you feel an itchy anus?
- Are you constipated?
- Have you noticed mucus or fresh blood on the toilet paper?
- Does the wound on the anus wet?
Physical examination
The doctor then inspects the anal area and gently palpates it. The characteristic, extremely painful mucosal injuries are usually found in the areas to be expected. In many cases, a rectal examination is only possible after local anesthesia. In this way, the doctor can assess whether the problem is possibly hemorrhoids or other diseases of the anus.
Rectoscopy
If there is an anal fissure, the doctor may do a rectoscopy (proctoscopy). He can take a closer look at the inside of the rectum and take samples of the mucous membrane. For the proctoscopy, the patient usually receives a local anesthetic (local anesthesia) - in the case of an anal fissure, the examination can be quite painful.
Further investigations
Should the doctor discover signs of a malignant disease (e.g. anal cancer), further examinations may be necessary. These can be, for example, blood tests, a colonoscopy, computed tomography (CT) or magnetic resonance tomography (magnetic resonance imaging, MRI).
Anal fissure: treatment
The treatment of an anal fissure depends on whether it is an acute or a chronic anal tear. The two forms differ not only in the duration (acute: max. 4-6 weeks; chronic: longer), but also in the extent of the tissue change:
- In the case of an acute anal fissure, the mucous membrane is damaged more superficially. This can be treated well with conservative (non-surgical) means. These include soothing ointments, creams, or hip baths.
- A chronic anal fissure develops when a deep ulcer develops from the acute mucosal injury and the wound edges change with scarring. Sometimes a rough fold of skin also forms (outpost fold). If conservative treatment methods do not work, the chronic anal fissure must be operated on.
An anal fissure is only operated on if absolutely necessary. There is a risk that the anal sphincter will be injured during the procedure. The patient may then no longer be able to control the defecation (faecal incontinence).
Anal fissure: conservative treatment
An acute anal fissure can be treated with special creams that relax the sphincter system. They contain calcium antagonists or nitrates as active ingredients. Agents that soften the stool and promote defecation, such as solutions with macrogol, are also helpful. Use laxatives only after consulting your doctor!
In addition, ointments for local anesthesia of the skin (anesthetic ointments) can be applied to an anal fissure. Pain relievers and anti-inflammatory ointments and suppositories are also often used.
Wash your hands before applying any ointment. This prevents wound infections.
Sitz baths that increase in temperature can also alleviate the symptoms of anal fissure. They promote blood circulation in the anus area. This strengthens the local defenses and allows the anal tear to heal better. This is how the Sitz bath works: Sit upright in the bathtub with your feet on a stool outside the bathtub. Add chamomile extract to the tub and start running lukewarm water first. Then increase the water temperature to 36 to 40 degrees over ten to 15 minutes. Then take a cold shower and lie down for an hour if possible (bed rest). If you feel cold in the bath, you can wear socks and a sweater.
Proper anal hygiene is also advisable with an anal fissure: It is best to wash the anal region with lukewarm water after using the toilet. Do not use soap or shower gel for this! Both of these can destroy the skin's natural protective acid film and dry out the skin. That makes them more susceptible to bacteria. Intimate washing lotions and intimate sprays are also not recommended.
You should also do without damp toilet paper. The additives contained in it can lead to allergic reactions of the skin. Use regular toilet paper that is as soft as possible.
If you have an anal fissure, make sure you eat a high-fiber diet: Consume at least 30 grams of fiber per day. These stimulate bowel movements and bind water in the feces. This makes the manure softer overall. A lot of fiber can be found in whole grain products, vegetables and fruits, for example. Wheat bran is also very valuable. But you have to make sure that you drink enough fluids. This is the only way for the fiber to swell well and act accordingly.
Tip: If you suddenly consume large amounts of fiber, you can get gas. Therefore, you should only slowly increase the fiber in your diet. This is how your digestive system can adjust to it.
In the case of a chronic anal fissure, it can be helpful to carefully dilate the anus several times a day with a special anal dilator. This can reduce spasms of the sphincter somewhat. The blood flow to the skin / mucous membrane improves and hardening is counteracted.
Anal fissure: surgery
If conservative measures in anal fissure therapy do not help enough, surgery is the last option. In general, anal fissure surgery is just a minor procedure that is performed under short or spinal anesthesia. The surgeon will remove the surrounding scar tissue as completely as possible. It is rare that part of the anal sphincter has to be removed. The procedure is usually carried out on an outpatient basis in younger patients. Elderly patients are temporarily admitted to the hospital for the operation.
Like any surgical procedure, anal fissure surgery also has its risks: nerves can be damaged, especially during operations in the area of the anal sphincter, which surrounds the anus in a ring. The possible consequence is that the patient can no longer control the discharge of feces in the future (fecal incontinence).
The healing process after the operation takes a long time (usually four to six weeks). It can lengthen if there is a wound infection. This is not uncommon for operations on the anus because this region of the body is heavily colonized with germs.
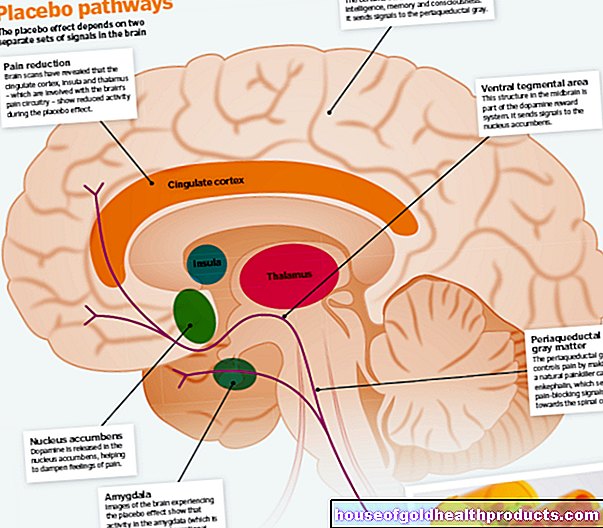
Anal fissure: botox
Botox injections into the anal sphincter are a new but expensive treatment option for chronic anal fissures. Botox (botulinum toxin) is a neurotoxin that paralyzes the sphincter muscle for several weeks. This allows the ulcer to heal in peace.
Anal fissure: disease course and prognosis
An acute anal fissure usually heals without problems after a few weeks if it is treated with conservative measures. If left untreated, however, there is a risk that it will become chronic. In addition, anal fistulas or abscesses (collections of pus) can develop.
In most cases, a chronic anal fissure can be successfully treated with surgery.
Acute or chronic - after successful treatment, an anal fissure can recur if the causes and risk factors (such as hard stool, strong pressure) are not eliminated. Make sure you have a high-fiber diet, adequate fluid intake and plenty of exercise. This keeps the stool soft and supports the bowel movement and can thus prevent (renewed) anal fissures.