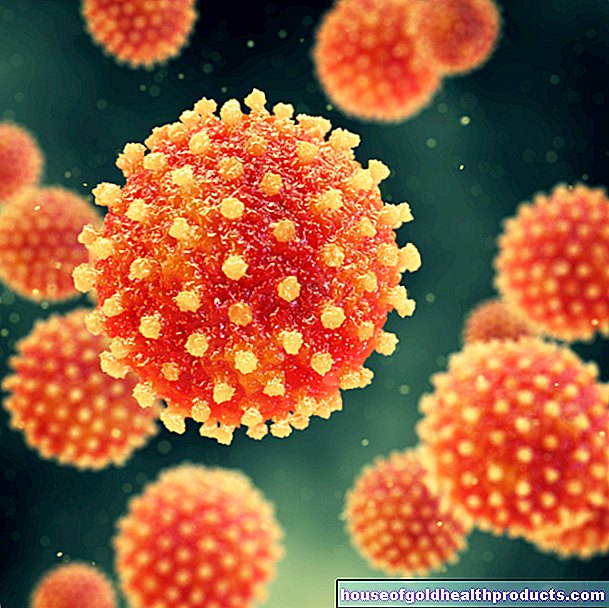
Corona: What role do the super spreaders play?
Christiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.A visit to a restaurant, a church service - even one infected person can infect numerous others. Such superspreaders pose a risk - but they also open up surprising opportunities to combat the pandemic.
The number of people infected and new infections in Germany is falling continuously - and with it the risk of contracting someone. But there is no all-clear. Two outbreaks in recent times show how quickly the situation can change again: Under unfavorable conditions, one or a few infected people can be enough to infect tens of people. In medicine, such people are called super spreaders.
Particularly problematic: Sars-CoV-2 infected people are highly contagious when the symptoms have not yet appeared. They then go unsuspectingly among people and, under unfavorable circumstances, infect many others.
Church service and restaurant - two super spreader events
This is what happened during the test run for a restaurant reopening on May 10th in the East Frisian district of Leer. Around 40 people were present, all of them adhered to the hygiene rules, the landlord assures. The balance of the happy occasion: 20 people - guests, staff and their contacts - subsequently tested positive for Sars-CoV-2. In addition, more than 100 other people are in quarantine.
Even more devastating was a service on May 1st in Frankfurt - the first in the congregation since the introduction of the contact restrictions. Here, too, the hygiene rules were adhered to, according to those responsible. So far, 200 of the participants have tested positive. It is not known how many are in quarantine.
Is it all just isolated cases?
These are still isolated cases. But it won't stop there. Because the virus isn't gone, it's just largely under the radar. With the relaxation, there will be more infections again - especially when groups of people meet in closed rooms.
The incidents can be explained - provided the rules are observed - using aerosols. The distance rules do not protect against swirling, virus-containing microparticles: At least in closed rooms, these aerosols remain in the air for longer and also spread further (read more on the subject in the article Aerosols - Contagion via the air).
In fact, the two outbreaks had one thing in common: the participants (at least mostly) did not wear masks. In restaurants, of course, this is only mandatory as long as you are not sitting at the table. Most of the time, the guests are "topless". And the Baptist congregation also announced that the lack of masks (which were previously not required for attending church services) and singing were probably responsible for the infection.
The superspread factors
The fact that two outbreaks from the first period of loosening became known should cause discomfort.
But that does not mean that in every restaurant or church in which an unknowingly infected person sits, many others are inevitably infected. In order for a so-called superspread event to occur, various unfortunate circumstances are likely to be linked.
Number 1 - Virulence: The infected person is particularly contagious right now. With Sars-CoV-2, this is unfavorably the case one to two days before and two to the days after the onset of symptoms. But there could actually be people who develop a particularly large amount of virus in their throats.
Number 2 - Behavior: Does the infected person give out hugs or kisses? Does he sing or shout? How loud someone speaks, whether they have a particularly wet pronunciation, is also decisive for the spread of the virus.
Number 3 - Breath intensity: Studies have already shown that when singing, for example, a particularly large number of infectious droplets are thrown out. Even those who exert themselves physically are more likely to secrete the virus than someone who sits relaxed in their chair.
Number 4 - Contacts: The infected person meets many people. And many of these in turn meet many more people.
Number 5 - Encounters without a mask: It is still unclear how well a simple mouth and nose mask actually protects the environment from the virus being emitted by the wearer. However, some of the infectious droplets or aerosols will be intercepted.
Number 6 - unfavorable spatial situation: It is particularly unfavorable if the infected person is in a closed room with many others. Then the decisive factor is how big the room is and how well it is ventilated. It depends on how much the virus concentration is diluted.
Number 7 - people on the move: But it also has a great influence whether the meeting is more static or dynamic. If the participants sit in fixed seats, as in the theater or cinema, the people sitting next to them in particular will be infected. In situations such as a standing reception, where those present mingle, are more likely to get infected.
Number 8 - Duration of the encounter: With a 10-minute get-together, the risk is significantly lower than with a two-hour visit to a restaurant.
Number 9 - the dispersion factor K: And there is still another factor - the dispersion factor k, also known as the scattering parameter. What's it all about?
The dispersion factor K-factor
Different diseases have different dispersion factors (scatter parameters). These describe, for example, whether a few individual super spreaders infect a great many others when an infection occurs - or whether the infections go back quite homogeneously to many infected people, i.e. whether there are no or few super spreaders.
The dispersion factor is mapped using the value k, which lies between zero and one. If it is very low, the super-spreaders have a high proportion of the infection rate - for example in the Sars-1 outbreak of 2003/2004. If the number is high, many people only infect a few others.
In seasonal flu, the k value is around 1. Superspreader events do not play a major role in the spread. In the SARS epidemic of 2002/2003, however, superspreading played a particularly important role. The k value was about 0.16. That was one of the reasons the spread could be quickly brought under control.
How many super spreaders are there in the current pandemic?
How high it is at Sars-CoV-2 is still unclear. According to two different calculations, it was 0.1, for example - then 80 percent of the infections could be traced back to 10 percent of the infected. So there would be a lot of super spreaders. According to another calculation, 20 percent of those infected infected the remaining 80 percent (k = 0.45).
Either way, superspreaders could play a not insignificant role in the spread of Sars-CoV-2. And that's good news. Why?
Stay vigilant, follow up consistently!
If superspreaders are a driving force in the pandemic, they can be contained much better. One measure is to include the risk factors for the respective situation and to reduce the risk as much as possible. Some examples:
- Thoroughly ventilate closed rooms regularly or leave windows open when the temperature is right.
- Wear masks as much as possible.
- Regular testing of people who have frequent contacts. This is already planned for medical staff, teachers and kindergarten teachers. This may also be useful for other professional groups such as hairdressers, fitness trainers, etc.
- Facilitate tracking of contacts, e.g. by leaving contact details or voluntarily using the app that is currently being developed.
Return to largely normalcy even without vaccination?
But if a superspread event becomes known, quick and consistent action is necessary, says Prof. Christian Drosten from the Berlin Charité in the NDR Podkast on May 26th. In that case, the contact persons must be immediately and consistently quarantined. "There is then no time for testing," said the virologist.
But above all, Drosten sees an opportunity in the significant spread of the virus via super spreaders: If it were possible to get the individual outbreaks under control quickly, the pandemic could possibly be effectively contained - even without vaccination.
It is crucial to take systematic action in the event of an outbreak: All contact persons have to go into quarantine immediately, even before a test result is available.
Tags: fitness digital health alcohol