pleurisy
and Martina Feichter, medical editor and biologistMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
In the case of pleurisy (pleurisy), the pleura and usually the pleurisy in the chest become inflamed. These are the sheaths of connective tissue around the lungs and on the inner wall of the chest. Typical symptoms of "dry" pleurisy are painful breathing. If fluid collects, it is called "wet" pleurisy. Read everything you need to know about signs, causes and treatment for pleurisy here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. J86J90J94A16
Brief overview
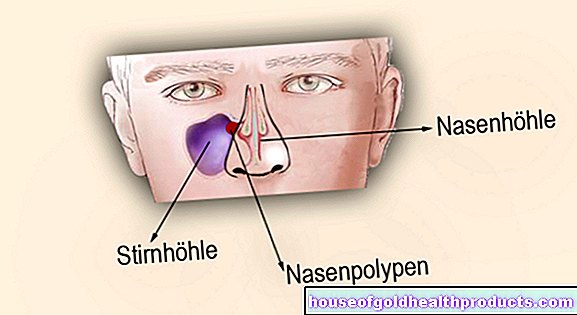
- Definition: In pleurisy (also pleurisy, pleurisy), the pleura, the pleura, is inflamed. This two-part layer of tissue lines the inside of the chest cavity (pleura) and covers the lungs (pleura).
- Caution: Even if one usually speaks of pleurisy, the second layer of the pleura, the pleura, is usually also inflamed.
- Symptoms: severe, breath-dependent pain when breathing ("dry" pleurisy); with "wet" pleurisy, decreasing pain and possibly breathing difficulties up to shortness of breath with large accumulation of fluid (pleural effusion); possibly fever
- Causes: pneumonia, pulmonary embolism, pulmonary infarction, tuberculosis, viral infection (Coxsackie B virus), autoimmune diseases (such as lupus erythematosus, rheumatoid arthritis), cancer, etc.
- Treatment: Treatment of the underlying disease (e.g. antibiotics for bacterial infection). Otherwise, symptom relief, for example with painkillers and antipyretic medication.
Pleurisy: symptoms
A pleurisy (or pleurisy) can cause different symptoms - depending on whether it is a "dry" pleurisy or a "wet" pleurisy. The difference between the two can be found in the so-called pleural cavity: This is the narrow, slightly fluid-filled space that separates the two thin leaves of the pleura:
The inner layer of tissue in the pleura is called the pleura and covers the lungs. The pleura joins on the outside and lines the chest cavity on the inside. The pleura and lungs are connected to each other at a fold at the edge of the lung.
The fluid between the pleura and pleura, i.e. in the pleural space, can change with pleurisy:
- "Dry" pleurisy (pleurisy sicca): no additional fluid in the pleural space. Most of the time, threads of fibrin (blood coagulation protein) are formed here, which increases the friction between the two sheets of the pleura.
- "Damp" pleurisy (exudative pleurisy): additional accumulation of fluid between the pleura and pleura (pleural effusion)
Pleurisy often affects only one side of the body. The left and right lungs, including the pleural cavities, are separated from each other by the mediastinum.
"Dry" pleurisy: symptoms
With pleurisy, both the pleura and the pleura are usually inflamed. Only the pleura is sensitive to pain - but this is even more so. The friction that arises between the two skins when breathing causes severe, breath-dependent and stabbing chest pain in dry pleurisy. The deeper the sick person breathes in, the more it hurts. This is why many patients only breathe shallowly. Some also instinctively assume a relieving posture, which relieves the inflamed side.
Dry pleurisy can also be accompanied by a painful cough. The pain is mostly one-sided. Depending on the severity of the inflammation, it can radiate into the shoulder.
Typical of pleurisy is also a creaking or rubbing breath, the so-called leather rubbing. It occurs because the pleura and pleura in the inflamed areas rub against each other with every movement of the chest.
If the pleurisy spreads to the diaphragm (the muscle plate that lies under the lungs), hiccups can also occur.
"Wet" pleurisy: symptoms
With a pleural effusion, more fluid collects in the pleural space than usual. In general, this can have various causes. If the pleural effusion forms in the course of pleurisy, doctors speak of "pleurisy exudativa" ("wet" pleurisy). Symptoms such as pain and leather rubbing are absent here or are greatly reduced. The effusion between the inflamed pleural leaves prevents them from rubbing painfully against each other.
On the other hand, other symptoms often arise with this form of rib inflammation: Signs of the pleural effusion can be difficult breathing or even shortness of breath (dyspnoea). This happens when the effusion is so large that it compresses the lungs significantly. With a small effusion, however, the patient can breathe normally.
Dry and moist pleurisy
Transition from dry to damp
Often a wet pleurisy develops from a dry one. This means that the inflammation causes fluid to escape from the fine blood vessels (capillaries) and collect as a watery effusion in the pleural space. If the pleural effusion is purulent, doctors speak of a pleural empyema. But it can also consist largely of blood (hemorrhagic pleurisy).
Sometimes fever accompanies the transition from dry to “wet” pleurisy.
Pre-existing illness affects symptoms
Other symptoms of pleurisy depend on the underlying disease. Some examples:
Pneumonia often causes a high fever with chills and a cough with sputum. If pleurisy develops as a result of tuberculosis, many patients also suffer from cough, fatigue and night sweats.
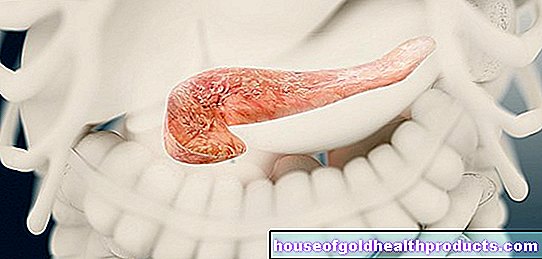
In the case of a Coxsackie B virus infection (Bornholm's disease), in addition to breathing difficulties, those affected also have cramp-like pain in the chest and upper abdomen. Such pain can also occur if the pleurisy is the result of a disease in the upper abdomen, such as inflammation of the pancreas (pancreatitis).
Cancer diseases such as a malignant tumor of the pleura (pleural mesothelioma) are also possible triggers of pleurisy. In an advanced stage, signs of pleural mesothelioma correspond to those of "normal" pleurisy.
Inflammation of the pleura: causes
Inflammation of the pleura can have a number of causes. It usually occurs with or as a result of another disease, for example:
- Inflammation of the lungs (pneumonia)
- tuberculosis
- Coxsackie B virus infection (Bornholm's disease)
- Tumors in the pleural area
- Connective tissue diseases (collagenoses) such as lupus erythematosus or rheumatoid arthritis
- Pulmonary embolism, pulmonary infarction
- Urea poisoning (uremia)
- Upper abdominal disorders such as pancreatitis
The most common underlying disease of pleurisy is pneumonia: the inflammatory processes can spread relatively easily from the lungs to the pleura.
The pleura can also be damaged directly, for example by Coxsackie B viruses or as a result of diseases in the upper abdomen (such as pancreatitis). Tuberculosis is also a possible cause of pleurisy. This so-called "pleurisy tuberculosa" has become rare in Central Europe.
Inflammation of the pleura with a bloody pleural effusion can be a sign of what is known as pleural cancer. Doctors use the term when a malignant tumor has formed daughter tumors (metastases) in the area of the pleura. This can happen with lung cancer and breast cancer, for example.
In rare cases, the cells of the pleura develop into cancer cells on their own. This creates a primary tumor of the pleura (pleural mesothelioma). This can trigger pleurisy. By the way: pleural mesothelioma mainly affects people who have come into contact with the construction and industrial material asbestos.
Pleurisy: examinations and diagnosis
First, the doctor has a detailed discussion with the patient to collect his or her medical history (anamnesis). He has the complaints that arise in detail. In addition, the doctor asks whether other illnesses (past or current) are known, for example pneumonia, tuberculosis or a tumor. If so, the doctor asks what therapies and medical interventions were carried out.
Physical examination
The anamnesis will be followed by a physical examination. Sometimes the doctor can tell from the patient's posture that something is wrong with the breathing on one side of the lung. In addition, the side of the body on which the pleurisy is located is usually less involved in breathing movements. This is known as "dragging".
Tapping and listening to the chest provide more precise clues. Typically, pleurisy can be heard with the stethoscope a creaking breath, the so-called leather rubbing. In the case of pleurisy with pleural effusion (exudative pleurisy), however, the noise is only weakened or can no longer be heard at all.
The doctor can also obtain valuable information from the knocking sound. For example, a muffled tapping sound can indicate an accumulation of fluid (pleural effusion).
Imaging procedures
To diagnose pleurisy, a chest x-ray (chest x-ray) is particularly important. The doctor usually takes pictures of the chest from the front and the side. A "dry" pleurisy is normal on the X-ray. On the other hand, a pleural effusion can usually be recognized well.
To make small or hard-to-see accumulations of fluid visible, the doctor can perform an ultrasound examination and, if necessary, a computed tomography (CT) scan.
The various imaging procedures not only help with the diagnosis of "pleurisy". They often also serve to clarify the cause of the inflammation. For example, imaging can make tuberculosis foci or tumors visible.
Further investigations
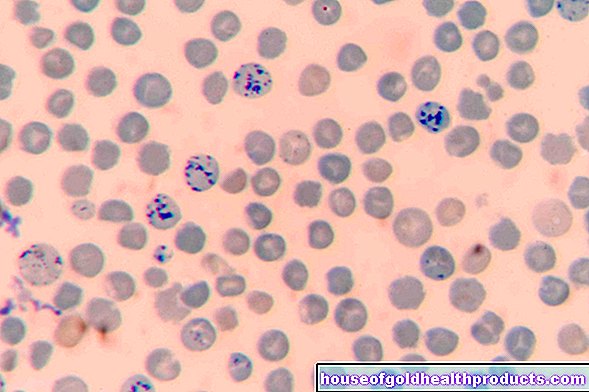
A blood test is also important if you have pleurisy. Using various inflammation parameters (such as blood cell sedimentation, CRP, white blood cells, etc.), the doctor can estimate how pronounced the inflammatory processes are.
If the doctor suspects that the pleurisy is caused by an autoimmune disease (such as lupus erythematosus), this can also be clarified for a blood test. It is checked whether antibodies can be detected in the patient's blood that incorrectly attack the body's own tissue (such as the pleura) (autoantibodies).
Analyzing the fluid in the pleural space can also help identify the cause of pleurisy. To do this, the doctor sticks a thin hollow needle between the ribs and pushes it forward to the pleural effusion in order to take a small sample (pleural puncture). The liquid is then carefully examined in the laboratory, for example for the presence of blood, pathogens (such as tuberculosis bacteria) or tumor cells.
In some cases, a thoracoscopy (thoracoscopy) is also useful. The doctor makes a small opening in the chest wall and inserts a laparoscope over it. Among other things, it is equipped with a small camera and a light source. This enables the doctor to examine the inside of the pleural cavity.
Pleurisy: treatment
Treating the underlying disease is part of any therapy for pleurisy.
For example, if bacteria are the trigger (as in tuberculosis or bacterial pneumonia), the patient is given antibiotics. These fight the pathogens directly. In addition, the symptoms are treated as needed, for example with pain relievers and antipyretic medication.
In other cases, viruses (e.g. Coxsackie B viruses) are the trigger for pleurisy. The treatment here is limited to alleviating the patient's symptoms (pain relievers, fever reducers, etc.). Medicines that specifically help against the viruses (such as antibiotics against bacteria) are not available here.
In the case of "wet" pleurisy, it may also be necessary to specifically remove the pleural effusion. To do this, the doctor usually performs a so-called thoracic drainage: a thin tube is pushed into the pleural space through a small opening in the chest wall. Then the effusion is sucked off. If necessary, the pleural cavity can also be rinsed with saline and antibiotics.
Chest drainage is necessary, for example, if the pleural effusion is large and causes shortness of breath. The procedure is also carried out in the event of a purulent effusion. Smaller, watery effusions, on the other hand, can usually be removed by the body itself.
Inflammation of the pleura: disease course and prognosis
The course of the disease depends on the cause and severity of the pleurisy. The duration and prognosis can vary widely, depending on how quickly and successfully the pleurisy can be treated. However, pleurisy usually has a good prognosis, especially in young people.
If the inflammation persists over a long period of time, the pleura and the pleura can grow together with a scar. Large-scale adhesions after pleurisy are also known as pleural calluses or pleural rinds. In extreme cases, these calluses can also calcify (pleurisy calcarea). This permanently restricts breathing.
Tags: healthy feet medicinal herbal home remedies menshealth