Pancreatic cancer
and Carola Felchner, science journalistDr. med. Julia Schwarz is a freelance writer in the medical department.
More about the expertsCarola Felchner is a freelance writer in the medical department and a certified training and nutrition advisor. She worked for various specialist magazines and online portals before becoming a freelance journalist in 2015. Before starting her internship, she studied translation and interpreting in Kempten and Munich.
More about the experts All content is checked by medical journalists.Pancreatic cancer (pancreatic cancer) is tricky: the disease remains symptom-free for a long time. Later, the symptoms resemble those of a chronically inflamed pancreas (upper abdominal pain, digestive disorders, etc.). This is why pancreatic cancer is often only discovered when it is more advanced. The chances of recovery are then usually poor. Read about the symptoms of pancreatic cancer, how the tumor develops and is treated, and what the prognosis is!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C25

Brief overview
- What is pancreatic cancer? Malignant tumor of the pancreas. Is relatively rare in Germany (around 16 out of 100,000 people develop it every year). The mean age of onset is 70 years (men) and 76 years (women). Despite its rarity, pancreatic cancer is the third most common tumor of the gastrointestinal tract (after colon and stomach cancer).
- Risk factors: smoking, alcohol consumption, obesity, diabetes (diabetes mellitus), hereditary breast cancer or ovarian cancer, etc.
- Symptoms: no complaints for a long time; later epigastric pain, back pain, weight loss, loss of appetite, jaundice, diabetes mellitus, nausea and vomiting, indigestion, fatty stools, etc.
- Examinations: blood tests (with determination of tumor markers), abdominal ultrasound, endoscopic ultrasound (endosonography), computed tomography (CT), magnetic resonance imaging (MRT), magnetic resonance cholangiopancreatography (MRCP; special MRI examination), removal and analysis of a tissue sample, possibly Laparoscopy, chest x-ray (chest x-ray) and other examinations
- Treatment: surgery, possibly chemotherapy, radiation therapy (only in certain cases), pain therapy
- Prognosis: Healing is only possible if the tumor is still locally limited. Because pancreatic cancer is often discovered late and usually grows rapidly and aggressively, the prognosis is generally poor.
Pancreatic cancer: symptoms
Pancreatic cancer symptoms are influenced by the type and location of the tumor:
The pancreas, which consists of the head, body and tail, is located in the upper abdomen behind the stomach and immediately in front of the spine. It consists of two different types of glandular tissue:
- The exocrine tissue forms the largest part. It produces digestive juice containing enzymes that is passed into the small intestine.
- Interspersed in the exocrine gland tissue are groups of cells from endocrine tissue, the so-called islets of Langerhans. These gland cells produce hormones such as the blood sugar lowering insulin and its counterpart glucagon. They are released into the blood.
About 95 percent of all pancreatic tumors develop from the exocrine gland tissue. In the remaining cases, the tumor arises from hormone-producing (endocrine) gland cells. Depending on the type of cell, one speaks of an insulinoma or a glucagonoma, for example.
The most common pancreatic cancer develops in the head part of the pancreas.
Cancer in the head of the pancreas
Common symptoms of pancreatic cancer
With any form of pancreatic cancer, those affected usually do not notice the disease for a long time. As soon as symptoms appear, the cancerous tumor often presses on neighboring structures (bile duct, stomach, small intestine, etc.) or grows into them. It is not uncommon for daughter resettlements (metastases) to be present. Symptoms of the following types are common at this advanced stage of pancreatic cancer:
- Persistent pain in the upper abdomen and back: The back pain can increase when you lie on your back.
- Loss of appetite
- Weight loss: If the exocrine tissue produces too few or no digestive enzymes as a result of pancreatic cancer, the nutrients in the intestine can only be broken down to a limited extent or not at all. The impaired supply of nutrients leads to weight loss.
- Digestive disorders and fatty stools: The lack of digestive enzymes from the diseased pancreas means, among other things, that the fat from food can no longer be properly absorbed in the intestine. It is then excreted undigested with the stool - the resulting fatty stool is light, shiny, and has a pungent odor.
- Nausea and vomiting
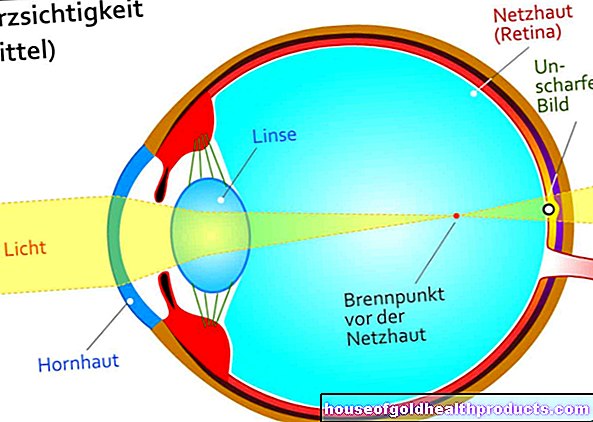
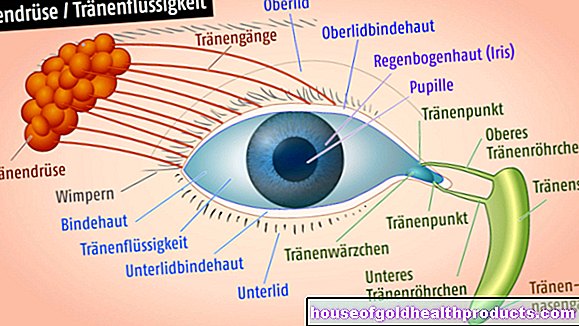
- Jaundice (jaundice): pancreatic cancer in the head of the pancreas can press on the bile duct or block it (this runs a little way through the head of the pancreas). The bile then builds up, which causes jaundice: the skin, mucous membranes and the white dermis in the eye turn yellow. The urine is dark, the stool light.
- Diabetes (diabetes mellitus): Sometimes the tumor produces too little or no insulin at all. It is then usually an endocrine tumor. The lack of insulin leads to diabetes.
The symptoms of pancreatic cancer are similar to those of inflammation of the pancreas (pancreatitis). Sometimes both diseases occur together. Both can make diagnosis difficult.
An endocrine pancreatic tumor sometimes produces an increase in the gastric acid-stimulating hormone gastrin. This can lead to the formation of a stomach ulcer because too much stomach acid is very irritating to the lining of the stomach. However, since stomach ulcers can also have other causes, they are no more specific symptoms of pancreatic cancer than back pain.
Smaller blood clots form less often in pancreatic cancer as a result of pressure on surrounding vessels. These can block the affected vessel (thrombosis). This often happens, for example, in the splenic vein, which runs near the pancreas.
The pancreas also contains a high concentration of the blood clotting factor thrombokinase. The organ changes caused by cancer can disrupt the blood coagulation system, so that small clots form everywhere in the vessels (disseminated intravascular coagulopathy, DIC). The coagulation factors are used up, which increases the risk of bleeding. In addition, clots can peel off and block a vessel elsewhere (embolism).
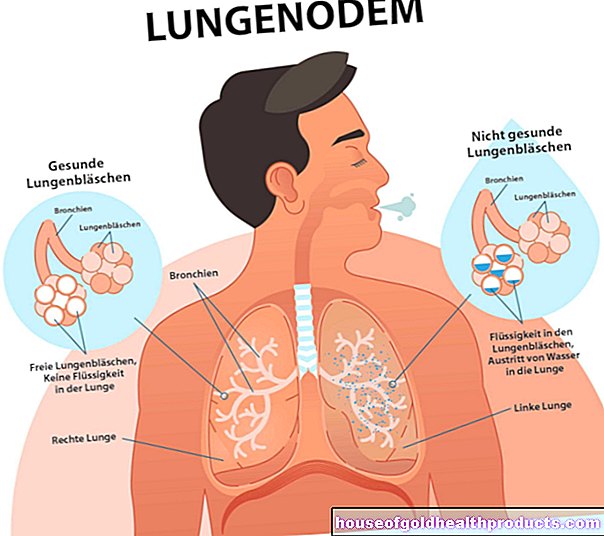
If the pancreatic cancer spreads to the peritoneum (peritoneal carcinosis), but the cancer cells release fluid into the abdominal cavity - "ascites" develops. Possible signs are a bulging or enlarged stomach, unwanted weight gain and indigestion.
Pancreatic cancer: treatment
A pancreatic carcinoma discovered at an early stage is attempted to be cured as completely as possible. Unfortunately, however, pancreatic cancer is often discovered very late. A cure is then usually no longer possible. The treatment then serves to alleviate the symptoms of the patient and to slow down or stop the further spread of the tumor (palliative therapy).
In principle, the doctor has various options for treating pancreatic cancer. When which therapy is useful depends on the individual case.
Operative therapy
Surgery is only an option for 10 to 20 percent of pancreatic cancer patients. The procedure is only really effective if the surrounding tissue is still free of cancer. If the tumor can be completely removed during the operation, a cure may be possible.
The most common pancreatic cancer develops in the head of the pancreas. A Kausch-Whipple operation is then generally performed: The surgeon removes the head of the pancreas as well as the gallbladder, bile duct, small intestine, the lower part of the stomach and regional lymph nodes. An alternative is the pylorus-preserving pancreatic head resection. The lower part of the stomach (pylorus = stomach outlet) is retained.
With pancreatic cancer in the tail of the pancreas, it is often necessary to remove the spleen as well.
In some cases of pancreatic cancer, it is not enough to cut out the diseased tissue from the pancreas - the whole pancreas has to be removed.
After the operation, many patients have to take the now missing pancreatic digestive enzymes in capsule form. This is the only way that digestion can continue to function.
chemotherapy
As a rule, the pancreatic cancer operation is followed by chemotherapy (adjuvant chemotherapy). Special drugs (cytostatics) are administered to prevent the rapid division of cells. The aim is to eliminate cancer cells that may still be present in the body after the operation. If possible, chemotherapy should be started within six weeks after the operation and should last six months.
Sometimes chemotherapy is given before the operation. This neoadjuvant chemotherapy is designed to shrink the tumor so that it can then be cut out more easily.
radiotherapy
Radiation therapy (radiotherapy) for pancreatic cancer is not generally recommended. However, it can be used in controlled studies. For example, one can try in such a study to support pancreatic cancer treatment with combined radiation and chemotherapy (radiochemotherapy). This comes into play in the case of locally advanced pancreatic carcinoma that cannot be operated successfully.
In the case of pancreatic cancer that is no longer curable, radiation can also be used specifically to alleviate symptoms (such as tumor pain).
Pain therapy
Many people with pancreatic cancer experience severe abdominal pain. These are treated by means of pain therapy according to the level scheme of the World Health Organization (WHO):
First you try to relieve the pain with non-opioid drugs such as paracetamol or ASA. If that is not enough, the doctor will also prescribe weakly effective opioids such as tramadol. If the pain cannot be brought under control, the non-opioid level 1 painkillers are combined with highly effective opioids (such as morphine). These have the strongest pain relieving effect.
In some patients with incurable pancreatic cancer, this drug-based pain therapy does not help sufficiently. Then you can try blocking a plexus of nerves in the abdomen, the so-called celiac plexus. This prevents the transmission of pain stimuli to the brain.
Other measures
Particularly in palliative pancreatic cancer treatment (i.e. in the case of cancer that is no longer curable), further measures are often taken for the benefit of the patient. The aim is to ensure that the patient can spend the rest of his life without (severe) discomfort as much as possible.
This can often be achieved with individually tailored pain therapy (as described above). If necessary, additional palliative measures can be added. For example, if the tumor constricts or closes the bile duct, those affected suffer from jaundice. Then an endoscopic procedure can help: With the help of a thin, tubular instrument (endoscope), the doctor inserts a small plastic tube (stent) into the bile duct to keep it open.
A gastric outlet enclosed by the tumor can also be widened using an endoscope. In the event of severe constriction, it can make sense to supply the patient with the necessary nutrients via a feeding tube in the future (enteral nutrition). Parenteral nutrition is also possible - the administration of nutrient solutions directly into the blood.
In addition to doctors, physiotherapists, masseurs, social workers, psychologists and pastors can effectively support the palliative treatment of pancreatic cancer patients.
For all palliative therapy measures for pancreatic cancer, the doctor and patient must bear in mind that the mean life expectancy for inoperable tumors is only three to five months after diagnosis. Therefore, measures that have serious side effects should be avoided here.
Diet in pancreatic cancer
Pancreatic cancer can destroy tissue in such a way that organ function is impaired. This also applies after an operation in which surgeons have removed the pancreas or parts of it. On the one hand, the pancreas produces important digestive enzymes. On the other hand, it controls the blood sugar balance with hormones such as insulin.
Diet in cancer of the head of the pancreas
If the cancer has spread to the head of the pancreas or if it has been removed, it mainly causes digestive problems. Mushy, fatty stools are the result. To replace the missing enzymes, doctors prescribe special drugs. These contain a mixture of enzymes (pancreatin) that compensates for the deficiency. Affected people take the capsules with a meal.
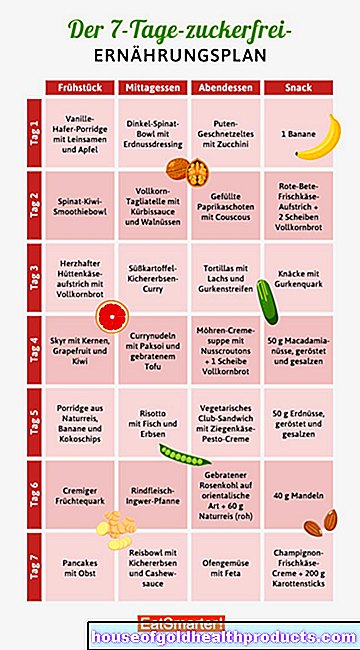
If you have cancer of the pancreas or after its operation, it is advisable to adjust your diet. Nutritional tips for pancreatic cancer are:
- No lavish meals: It is better to eat several times throughout the day (five to eight times) and in smaller quantities.
- No high-fat meals: Also use special fats when cooking, so-called MCT fats (= medium-chain triglycerides). You can find these in a health food store, for example.
- Easily digestible: Eat light whole foods. Avoid large amounts of raw vegetables or flatulent foods such as cabbage, onions or legumes. Heavily smoked, grilled or fried meat products are also less on the menu.
- Chewing copiously: This means that enough saliva mixes with the food. This is because it contains substances that have a similar effect to the enzymes in the pancreas.
- Drink the right thing: Drink water, tea or vegetable juices in particular. When it comes to pancreatic cancer, it's best to leave the alcohol aside. He puts a lot of strain on the organ.
The general rule is: Eat what you can tolerate best. A food diary can help to find out.
Diet in pancreatic tail cancer
If the tail of the pancreas is affected, digestion is often only slightly affected. However, this usually disrupts insulin production. So patients become diabetic (pancreatic diabetes) and have to inject insulin. Special diabetes and nutritional advice can then help those affected.
Because in addition to injecting insulin, they must now also learn to recognize the signs of hypoglycaemia, for example. Symptoms include, for example:
- Tremble
- Cravings
- sweat
- Racing heart
- Circulatory disorders
- fatigue
- confusion
- Fainting, coma
Those affected should always carry glucose or special sugar solutions with them in an emergency.Also inform the people in your area so that they know what is going on in an emergency and can help accordingly.
Nutrition with removal of the whole pancreas
If the cancer has destroyed large parts of the pancreas or if doctors have completely removed the organ, both important digestive proteins and hormones are missing. Those affected then also receive medication with enzymes and henceforth inject themselves with insulin. Here, too, the treating doctors and nutritionists are the most important contacts.
In severe cases in particular, oncological rehabilitation makes sense after treatment has been completed. Here, trained specialists help, among other things, to successfully implement new eating habits.
Pancreatic cancer: causes and risk factors
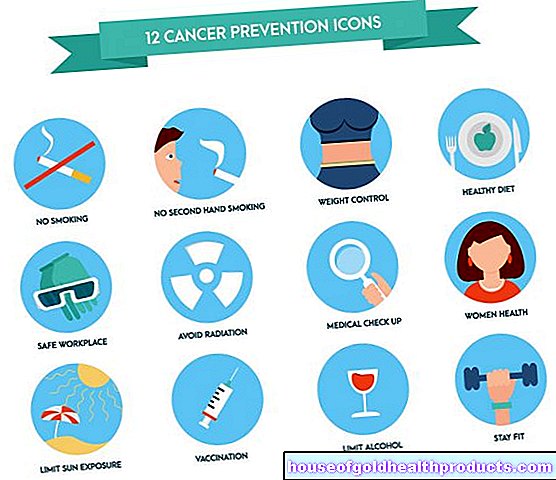
It is not yet fully understood why pancreatic cancer develops. Hereditary predisposition probably plays a certain role. Smoking and alcohol consumption are established risk factors: According to experts, the so-called cotinine level is increased in heavy smokers. This substance is produced when nicotine is broken down in the body and is considered to be carcinogenic. Regular alcohol consumption often causes the pancreas to become inflamed - and chronic inflammation makes the glandular tissue more susceptible to pancreatic cancer.
The metabolic changes in the case of excessive weight and abdominal fat can also lead to a kind of chronic inflammation. Therefore, obese people are more likely to develop pancreatic cancer. Since the pancreatic tissue is also pre-damaged in diabetes mellitus patients, they too are more susceptible to pancreatic cancer.
Certain diseases are other established risk factors. Women with hereditary breast cancer or ovarian cancer and their relatives have an increased risk of pancreatic cancer. Some rare hereditary diseases also make people more susceptible to malignant pancreatic tumors (e.g. Peutz-Jeghers syndrome).
In addition, there are some factors that are thought to increase your risk of pancreatic cancer. These include the frequent consumption of sugar as well as smoked or grilled food and frequent contact with certain chemicals and toxins (chromium and chromium compounds, chlorinated hydrocarbons, herbicides, pesticides, etc.).
Tip: To reduce the risk of pancreatic cancer, one should not smoke, avoid alcohol as much as possible and maintain a healthy body weight. A diet rich in fruit and vegetables may also reduce the risk of the disease.
Pancreatic cancer: examinations and diagnosis
If pancreatic cancer is suspected, the doctor will first have a detailed discussion with the patient in order to collect their medical history (anamnesis). Among other things, he has all complaints described in detail, asks about any previous illnesses and any known pancreatic carcinoma diseases in the family.
The anamnesis is followed by a wide variety of examinations. They serve to clarify the suspicion of pancreatic cancer and to rule out diseases with similar symptoms (such as pancreatitis). If the suspicion of pancreatic cancer is confirmed, the examinations also help to determine the spread of the tumor in the body.
- Physical examination: For example, the doctor palpates the abdomen to determine any swelling or hardening in the abdomen.
- Blood test: A blood analysis gives the doctor information about the general health of the patient and the function of various organs (such as the liver). In addition, so-called tumor markers are determined. These are certain substances that can be increased in a tumor disease (CA 19-9, CA 50, CEA). Using the tumor markers, the tumor stage can be determined and the course of the disease assessed.
- Abdominal ultrasound: The doctor can use ultrasound to assess the size and condition of the pancreas and other abdominal organs (liver, gallbladder, stomach, small intestine, etc.) and the surrounding lymph nodes.
- Endosonography: This is an endoscopic ultrasound examination (ultrasound "from the inside"). For this purpose, a tubular instrument (endoscope) with a small ultrasound probe is pushed over the mouth and stomach into the duodenum. Since the pancreas is close to it, even the smallest changes in tissue can be detected in the ultrasound. If necessary, the doctor can insert a fine hollow needle into the interior through the endoscope in order to take a tissue sample from the pancreas (biopsy).
- Tissue sample: As mentioned, tissue samples are usually taken from suspicious areas as part of endosonography. You can also insert a hollow needle directly through the abdominal wall into the pancreas in order to remove tissue.
- Computed tomography (CT): With this special X-ray examination, detailed sectional images of the pancreas and other structures are made. In this way, the doctor can assess the exact location and size of the tumor and detect any settlements (e.g. in lymph nodes or liver).
- Magnetic resonance tomography (MRT): Here, too, detailed sectional images of body structures are made, but with the help of strong electromagnetic fields. The location and spread (metastases) of the cancer can be clearly seen on it. Magnetic resonance cholangiopancreatography (MRCP) is particularly meaningful with regard to a pancreatic cancer diagnosis: In this MRI examination, the duct systems of the pancreas and bile are shown in detail. Most pancreatic carcinomas develop from the cells that line the exocrine gland ducts (called adenocarcinomas).
- Laparoscopy: Sometimes there are indications that the pancreatic tumor has already spread to neighboring organs or into the peritoneum (for example in the case of a greatly increased tumor marker CA 19-9 or ascites), although the imaging does not reveal any metastases. Then a laparoscopy (laparoscopy) can bring clarity.
- Chest X-ray: Any daughter tumors (metastases) in the lungs can be seen on the X-rays.
Pancreatic cancer: stages
Depending on the extent of the malignant tissue change, pancreatic cancer is divided into four stages:
- Stage 1: The tumor is limited to the pancreas.
- Stage 2: The adjacent tissue is also affected by the cancer.
- Stage 3: There are metastases in the lymph tissue.
- Stage 4: Metastases have also formed in other organs (such as lung or liver metastases).
Pancreatic cancer: disease course and prognosis
The course of the disease in pancreatic cancer depends above all on the type of tumor: Most pancreatic carcinomas are adenocarcinomas (developed from the cells that line the exocrine glandular ducts). These tumors grow quickly and quickly spread to other parts of the body via the blood and lymph. If they are not discovered early (which is rarely the case), the prognosis looks rather poor. In contrast, rarer forms of pancreatic cancer tend to grow more slowly and less aggressively. Your prognosis is therefore usually more favorable.
In general, the earlier a pancreatic carcinoma is discovered and treated, the better the chances of recovery. If the tumor is inoperable, life expectancy is low: on average, those affected die three to four months after diagnosis.
Overall, pancreatic cancer has the lowest survival rates of all cancers: five years after diagnosis, only nine to ten percent of patients have not yet died of the pancreatic tumor (relative five-year survival rate for Germany).
Additional information
Books:
- Pancreatic cancer: advice and help for those affected and their relatives (advice & help) by Hermann Delbrück, Kohlhammer, 2010
Guidelines:
- Guideline "exocrine pancreatic carcinoma" of the German Cancer Society and the German Society for Gastroenterology, Digestive and Metabolic Diseases
- Patient guideline "Cancer of the pancreas" of the German Cancer Society and the German Society for Gastroenterology, Digestive and Metabolic Diseases
Self help:
- The working group of pancreatectomized e. V .: https://www.bauchspeicheldruese-pankreas-selbsthilfe.de/
- The German Pancreas Club e.V .: http://www.med.uni-magdeburg.de/dpc
- TEB e.V. self-help: http://www.teb-selbsthilfe.de/
- Pancreatic Cancer Center: http://www.bauchspeicheldruesenkrebszentrale.de/