Meniere's disease
Clemens Gödel is a freelancer for the medical team.
More about the experts All content is checked by medical journalists.Menière's disease is a disease of the inner ear that is believed to be caused by excess pressure in the inner ear. The three most important symptoms are unpredictable attacks of sudden vertigo, ringing in the ears (tinnitus) and decreased hearing. Menière's disease is basically not curable, but the severity and frequency of the attacks can be reduced with medication. Find out more about the symptoms and treatment options for Menière's disease here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. H81
Meniere's disease: description
The French doctor Prosper Menière described Menière's disease, which is named after him, as early as 1861. In 1938, doctors Hallpike and Yamakawa reported enlarged spaces in the inner ear in Menière's disease patients believed to be related to the disease.
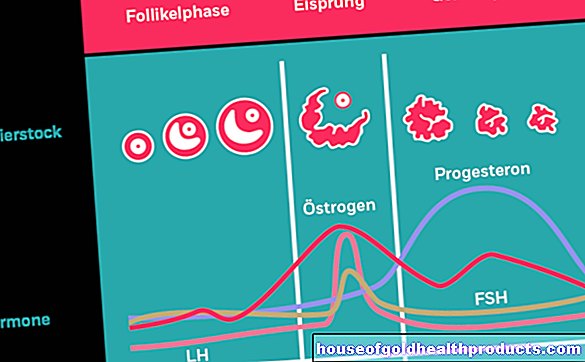
The cochlea and the organ of equilibrium as well as two different fluids - including the so-called endolymph - are located in the inner ear. According to the current state of knowledge, the absorption of this fluid in the inner ear is disturbed in Menière's disease. This causes too much endolymph to accumulate. Since the inner ear is lined with a membranous membrane, the fluid can only expand to a limited extent. The result is an increase in pressure in the inner ear, which damages the cochlea at a certain point (see causes and risk factors).
It is estimated that around ten percent of all vertigo attacks are caused by Menière's disease. Menière's disease often occurs between the ages of 40 and 60. But people in young adulthood also develop Menière's disease. Men are affected more frequently than women. In total, around half a million people in Europe suffer from Menière's disease.
Meniere's disease: symptoms
The vertigo that occurs in attacks in combination with ringing in the ears (tinnitus) and unilateral hearing loss is typical of Menière's disease. With vertigo, those affected have the feeling that the environment revolves around them very quickly (similar to a ride on the merry-go-round). The dizziness can be so severe that people have to lie down. Falls due to dizziness and nausea with vomiting can also occur. Spinning vertigo is described by those affected as the most stressful of Menière's disease symptoms, as this vertigo occurs without warning and can last for hours to days.
In addition, there are tinnitus and hearing loss, which mainly affects low tones. People affected often feel pressure on the ear during a Meniere's disease attack. While only one ear is usually affected at the beginning of the disease, Menière's disease can spread to the second ear as the disease progresses.
In addition to these main characteristics of Meniere's disease, people often get pale and sweaty. The eyes may begin to tremble (nytagmus).
Meniere's disease attacks come suddenly and suddenly. Mostly they last between ten and twenty minutes, but they can last for hours. Then the attacks usually stop by themselves. Since the Meniere's disease attacks are extremely stressful due to the vertigo and occur completely unpredictably, psychological problems such as anxiety disorders and depression can develop. This can create a vicious circle between the seizures and the psychological situation of the person concerned. The resilience in stressful situations is often reduced as a result.
Meniere's disease: causes and risk factors
According to the current state of knowledge, the cause of Menière's disease is a disorder in the inner ear. This assumption is based on the fact that the majority of those affected have enlarged spaces in the inner ear. However, it is still unclear whether this finding is causally related to Menière's disease.
The inner ear is responsible for the sense of hearing and balance. It consists of a complicated duct system filled with two different fluids (endolymph and perilymph). These are in a sensitive equilibrium and are essential for the function of the organ.
Doctors believe that Meniere's disease is caused by excess fluid (hydrops) in the endolymph. The excess can result from a disturbed outflow or inflow. The increased endolymph creates high pressure in the inner ear, causing the so-called Reissner membrane to tear again and again - the suspected trigger for Menière's disease. The Reissner membrane is a thin cell membrane inside the cochlea. It is equipped with sensory cells for hearing and balance and separates the endo- and perilymph from each other. The two liquids (endo- and peripheral lymph) mix through cracks in the membrane, which disrupts the fine balance of salts (electrolytes) in these liquids. The crack also leads to a sudden change in pressure ratios. Overall, this results in a malfunction of the sensory cells, which could explain the symptoms of Menière's disease.
Possible causes for the excess fluid include the rare inflammation of the inner ear (labyrinthitis) or a concussion. In most cases, however, the cause remains unclear.
Meniere's disease: examinations and diagnosis
The first point of contact if you suspect Menière's disease is your family doctor. Depending on the symptoms, this person may be referred to the ENT doctor or neurologist. Many clinics also have special "vertigo centers" that are the contact persons, especially in severe cases.
During the consultation with the doctor, the doctor will first inquire about your symptoms and any previous illnesses. Possible questions from the doctor could include:
- Can you describe to me how you got caught up in vertigo?
- Is the dizziness also accompanied by tinnitus and hearing loss in that ear?
- How long does the vertigo attack last?
- Can the vertigo attack be provoked by a certain movement, for example by turning the neck? (This would speak against Meniere's disease.)
- Do you take any medicine?
Physical examination
During the physical examination, the doctor looks at the eardrum in the ear with a so-called otoscope. Although the damage in Menière's disease lies in the inner ear and is therefore not visible from the outside, existing diseases of the eardrum and middle ear should be excluded by inspection with an otoscope.
The standard tests in ear, nose and throat medicine also include the Weber and Rinne tuning fork test. A vibrating tuning fork is placed on the top of the head or behind the ear.The patient must indicate when he can no longer hear the sound of the tuning fork or whether he can hear it again when the tuning fork is held in front of the ear (Rinne test). He should also state whether the tone of the tuning fork placed on the top of the head appears louder in one of the two ears (Weber test). These tests can be used to draw conclusions as to whether the symptoms are caused by damage to the inner or middle ear.
As part of the clarification of Menière's disease, a check is also made to determine whether the patient has any involuntary eye movements ("nystagmus"). Typical for Menière's disease are twitching eye movements to one side (horizontal nystagmus), which usually only occur during the seizure.
Further investigations
A hearing test (tone threshold audiometry) must be carried out in order to be able to assess an existing hearing loss more precisely. In people with Menière's disease, hearing is significantly reduced in one ear. In addition, the hearing performance for low frequencies in particular is reduced. In many cases, hearing recovers after the seizure, but sometimes permanent hearing loss persists.
In addition, brain waves that occur after a sound signal (= acoustic evoked potentials) can be analyzed in order to check the connections of the auditory pathway in the brain. These compounds are not affected in Meniere's disease.
Symptoms such as those seen in Menière's disease can occur in a similar way in other diseases. These alternative causes of Meniere's disease symptoms need to be ruled out. For example, the auditory nerve is examined to ensure that it is not damaged. Computed tomography (CT) and magnetic resonance imaging (MRI) can be used to take images of the head and inner ear. In this way, for example, tumor and inflammatory processes can be excluded.
Diagnosis of Meniere's disease:
The diagnosis of Menière's disease can be made on the basis of four criteria established by an American professional association of specialists. If all of these four criteria are met, Menière's disease can be assumed:
- Two or more attacks of dizziness, each lasting a minimum of 20 minutes
- Hearing deterioration confirmed by an examination
- Ringing in the ears (tinnitus) or pressure in the affected ear
- Exclusion of other causes
Meniere's disease: treatment
Menière's disease therapy pursues two main goals: On the one hand, the severity of the symptoms in an acute attack should be reduced to a tolerable level. On the other hand, one tries to prevent further attacks with preventive measures (prophylaxis) so that these occur as rarely as possible.
Acute therapy
To combat dizziness and vomiting caused by Menière's disease, various anti-vertigo medications (antivertiginous drugs) can be used. The standard drug is the active ingredient dimenhydrinate. Menière's disease sufferers should always have this with them in order to be able to react immediately in the event of a sudden attack.
In severe cases of Menière's disease, diazepam, which belongs to the so-called benzodiazepines, can also be used. Benzodiazepines should only be used for short periods of time as they impair brain function and in some cases can lead to dependence.
Prevention (prophylaxis)
In addition to acute therapy, the most important goal is to reduce the number of attacks. There are a number of therapy options for this. The current recommendation for seizure prophylaxis in Menière's disease is the administration of betahistine. A high dose of this active ingredient can significantly reduce the number of attacks of Menière's disease. Betahistine stimulates the docking points (receptors) for a certain messenger substance (histamine) and thereby improves the blood circulation in the inner ear. Due to the higher blood flow, the excess fluid (endolymph) in the inner ear is probably transported away more quickly - the pressure in the inner ear drops.
For the treatment of Meniere's disease, the doctor prescribes betahistine. To avoid stomach irritation, it should be taken after eating. Other possible side effects include headache, vomiting, and allergic reactions. In the case of known gastrointestinal ulcers, the drug should not be taken. After six to twelve months, an attempt can be made to slowly reduce the therapy.
The anti-inflammatory cortisone can also be used to prevent Menière's disease. It can be injected into the middle ear through the eardrum under local anesthesia (intratympanic corticosteroid therapy). From there, the cortisone diffuses into the inner ear, where it has an anti-inflammatory and vascular sealing effect. For a few years now, this therapy has also been used in particular to treat sudden hearing loss.
Psychological care
In addition to the medical treatment of Menière's disease, psychological support is very important for Menière's disease. The sudden and unpredictable attacks can become a serious psychological burden.
Elimination of the organ of equilibrium
If the therapies mentioned remain unsuccessful in Menière's disease patients, there are very radical procedures that completely and permanently switch off the affected equilibrium organ: This can be done either with medication or by destroying the equilibrium organ with an operation. These procedures lead to hearing loss or deafness and a loss of the sense of balance. They are also irreversible (irreversible). The healthy side can partially take over these functions. The radical, surgical procedures, in particular, are only used in severe cases, since Menière's disease can also affect the other side in the course of the disease and once the functions have been destroyed, they cannot be restored.
Medicinal deactivation of the inner ear consists in injecting the antibiotic gentamicin into the middle ear in order to render the balance organ in the inner ear inoperative. This can be repeated at intervals of several weeks. The large interval between gentamicin doses is necessary in order to avoid undesirable damage to the cochlea (also in the inner ear) as much as possible. Gentamicin can cause hearing loss. For this reason, Menière's disease patients in particular are treated with gentamicin who have significant hearing impairment even before treatment.
If you do not achieve sufficient success in this way, a part of the inner ear, the so-called labyrinth, can be removed as a last resort for Menière's disease (labyrinthectomy). However, this therapy is controversial. Surgical therapies are not recommended at the moment.
Alternative therapies
Aside from conventional medicine, there are also alternative therapeutic approaches for treating Menière's disease. Homeopathy can help, above all, to reduce the often excruciating dizziness. It is recommended to take Cocculus D6 three times a day for several weeks. Tabacum D12 is used to interrupt the seizure.
The concept of homeopathy and its specific effectiveness are controversial in science and not clearly proven by studies.
Certain diets (especially salt-free foods) also alleviate the symptoms of some Menière's disease sufferers. Further supportive therapies are acupuncture, Feldenkrais or balance training.
Menière's disease: disease course and prognosis
The course of Menière's disease varies greatly from person to person. It is possible that it could stay with a single seizure. Most of the time, however, the attacks are repeated. But even after five years, Menière's disease can end spontaneously and never recur. Any damage to hearing and balance that has occurred up to that point usually remains permanent in this case as well. These sequelae of Menière's disease attacks can range up to complete numbness on the affected side. After five years of illness, symptoms affect both sides in 50 percent of cases.
Certain professions that place high demands on the sense of balance are sometimes no longer possible as a result of Menière's disease. Recognition as a disability is possible for those affected by Menière's disease. However, severe disability is only attested in serious cases with very numerous and / or severe illness attacks.
Last but not least, the decisive factor for the prognosis of Menière's disease is how great the influence of the complaints is on the psyche of an affected person. The fear of new attacks is very stressful and can in turn provoke new attacks. Breaking this vicious circle, if necessary with therapeutic support, is an important therapeutic goal in the treatment of Menière's disease.
Tags: drugs pregnancy birth digital health