Coronavirus: mutations
and Christiane Fux, medical editor Updated onMaximilian Reindl studied chemistry and biochemistry at the LMU in Munich and has been a member of the editorial team since December 2020. He will familiarize himself with medical, scientific and health policy topics for you in order to make them understandable and comprehensible.
More posts by Maximilian ReindlChristiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.At the moment, the delta variant from Sars-CoV-2 is of particular concern to experts: It not only appears to be more contagious, but also more dangerous than the original wild type. Other mutations have proven to be at least more contagious. Here you can find out what properties the different coronavirus mutations have, where they spread and why the vaccinations still protect very well.
Mutations are normal
The emergence of new virus variants is nothing unusual: Viruses - including the Sars-CoV-2 pathogen - repeatedly randomly change their genetic makeup during replication. Most of such mutations are meaningless. But some are beneficial to the virus and prevail.
In this way, viruses are able to quickly adapt to the environment and their host. This is part of their evolutionary strategy.
In the meantime, however, so-called "Variants of Concern" (VoC) have emerged with Sars-CoV-2 - that is, variants that are of concern to experts. What they have in common is that they are more contagious than the original form of Sars-CoV-2.
These are the following four variants:
- Alpha: The line, also known as B.1.1.7, spreads from Great Britain.
- Beta: The line, also known as B.1.351, spreads from South Africa.
- Gamma: The line, also known as P.1, spreads from Brazil.
- Delta: The line, also known as B.1.617, spreads from India.
Virus variations are grouped into so-called clades or lines - researchers create a kind of "family tree of the coronavirus". Each variant is characterized according to its genetic make-up and given a combination of letters and numbers. Whether or not a certain virus strain is more dangerous cannot be determined from this designation - it is only used for systematic recording and documentation.
By the way: The World Health Organization (WHO) recently suggested introducing new names for the most important Sars-CoV-2 variants. According to the WHO, individual virus variants are now to be named in ascending order according to the Greek alphabet.
This new, simpler and, above all, neutral description is intended to prevent new virus variants from being equated with the location of their first detection. This is to prevent unjustified and scientifically unfounded stigmata, discrimination and prejudice against individual countries in the public debate.
Most likely. A study from Scotland published in the prestigious journal The Lancet shows that the risk of hospital treatment for an infection with Delta is twice as high as with the original variant.
Do the vaccinations protect against the Delta variant?
Yes. BioNTech / Pfizer protects 79 percent against illness against Delta after the second vaccination dose compared to 92 percent against the alpha variant, which was initially detected in Great Britain. After vaccination with AstraZeneca, the protection after the second vaccination dose is 60 percent compared to 73 percent.
These numbers relate to mild and moderate symptomatic courses. How well the vaccinations protect against severe disease and death is not taken into account. But it is precisely here that the protection rating could be significantly better.
Delta Virus - Immunological Facts
The delta variant of the coronavirus (B.1.617) was first found in India. It shows three sub-variants and combines several characteristic changes. Such a bundling was demonstrated for the first time in a virus variant.
On the one hand, these are changes in the spike protein, which is considered the “key” for the human cell. On the other hand, B.1.617 also shows changes that are discussed as a (possible) escape mutation.
Specifically, B.1.617 combines the following relevant mutations:
Mutation D614G: It can make the coronavirus more contagious. Initial modeling indicates that B.1.617 is transmitted at least as easily as the very contagious alpha variant (B.1.1.7).
Mutation T478K: It leads to an exchange of the uncharged amino acid threonine by the lysine at position 478, protonated under physiological conditions - and thus positively charged. It is assumed that this amino acid exchange influences the interaction with the ACE2 receptor. Experts suspect that this could trigger more severe Covid-19 illnesses.
Mutation P681R: Researchers also associate this with a possible increased virulence.
Mutation E484K: Was also found in the beta variant (B.1.351) and the gamma variant (P.1). It is suspected of making the virus less sensitive to neutralizing antibodies that have already been formed.
Mutation L452R: It is also discussed as a possible escape mutation. Coronavirus strains with the L452R mutation were partially resistant to certain antibodies in laboratory experiments.
Other known virus variants
In addition, additional Sars-CoV-2 virus variants developed that differ from the wild type - but experts do not currently count them as VOCs. These virus strains are called "Variants of Interest" (VOI) - that is, variants of particular interest.
It is not yet clear what impact these emerging VOI could have on the pandemic. Should they hold their own against strains of viruses that are already in circulation, they too could be upgraded to corresponding VOCs.
Variants of particular interest
According to the European Center for Disease Prevention and Control (ECDC), these VOI currently include:
- Eta: proven in many countries (B.1.525)
- Iota: First discovered in the USA in the New York area (B.1.526)
- Kappa: first discovered in India (B.1.617.1)
- Lambda: first discovered in Peru (c.37)
In addition, according to the ECDC, there are further VOI that are not yet described according to the new WHO nomenclature:
- B. 1,620 of unknown origin.
- B. 1,621 first discovered in Colombia.
According to information from the ECDC and the WHO, the variants previously mentioned as epsilon, zeta and theta are no longer part of the VOI. The variant B.1.616, which was detected for the first time in France, also circulated for a long time without having any significant impact on the pandemic.
Variants under observation
The so-called “Variants under monitoring” (VUM) are also in the expanded focus - however, there is still a lack of reliable, systematic data on these. Most of the time, there is only evidence of their bare existence. They include sporadically occurring variants or “modified” - or better said, further developed - descendants of already known mutations.
According to the ECDC, these rare VUM currently include:
- B.1.427 and B.1.429 - previously referred to as Epsilon by the WHO, now downgraded, first discovered in California.
- P.2 - previously referred to as Zeta by the WHO, now downgraded, first discovered in Brazil.
- P.3 - previously referred to as theta by the WHO, now downgraded, first discovered in the Philippines.
- B.1.214.2, A.27, A.28, C.16 and B.1.1.318 - variants of unknown origin.
- Other variants that were first detected in South Africa: B.1.351 + E516Q and B.1.351 + P384L, C.1.2
- Other variants that were first detected in Great Britain: B.1.1.7 + L452R and B.1.1.7 + S494P, A.23.1 + E484K, AV.1, B.1.671.2 + K417N
- Other variants that were first detected in the USA: B.1.526.1, B.1.526.2
- Variant that was first detected in Russia: AT.1
- Variant that was first detected in Egypt: C.36 + L452R
- Variant that was first detected in Mexico: B.1.1.519
Although a great number of new virus variants are now known, this does not automatically mean a greater threat. A risk assessment is not yet possible at this point in time. The influence of this VUM on the (global) infection process cannot be foreseen either. So whether some virus variants are relevant or dangerous can only be clarified by further observations.
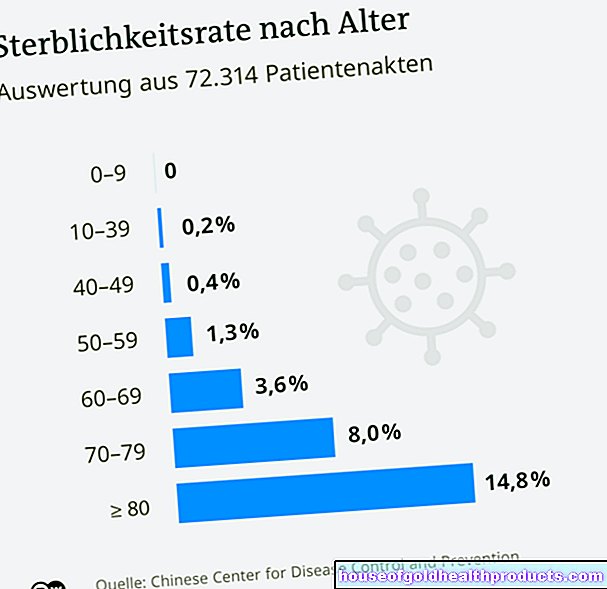
How dangerous are coronavirus mutations?
The coronavirus mutations officially classified as "Variants of Concern" are, according to the current state of knowledge, more dangerous than the wild type of the coronavirus. They are highly contagious and their appropriated changes (escape mutations) could promote secondary infections.
However, a general assessment of whether other coronavirus mutations are more dangerous than the original Sars-CoV-2 pathogen is not easily possible. There is a lack of experience and a solid database, especially with the newly emerging variants.
What does the higher contagious power mean?
If the Sars-CoV-2 becomes more contagious, it will also be more difficult to stop its spread. Measures that have so far successfully contained the spread may then no longer suffice.
If, for example, it is possible to lower the replication value R for the wild form of the virus to 0.8 and thus gradually reduce the number of infected people, a virus that is around 35 percent more contagious would spread further and set chains of infection in motion if the same measures were taken.
What does this mean for the vaccines?
There is no general answer to this. A possible reduced protective effect of the newly developed vaccines is lively discussed in specialist circles. So far, the vaccine manufacturers and preliminary investigations have given the all-clear in this regard.
For example, Comirnaty shows in initial studies a comparable effectiveness against the alpha variant (B.1.1.7) and beta variant (B.1.351). VaxZevria also seems to give good protection in B.1.1.7, but the effectiveness against the B.1.351 line could be reduced.
To what extent the other vaccines from Moderna and Johnson & Johnson will hold their own against the modified virus variants has not yet been conclusively clarified.
As the virus progresses, vaccine adjustments may be necessary. However, due to the progress in vaccine development, this can be done in a short period of time. However, all vaccines approved in the European Union still provide effective and adequate protection - especially against severe and fatal courses of Covid-19.
Further information on the subject of coronavirus vaccines can be found here.
How quickly does Sars-CoV-2 mutate?
In the future, Sars-CoV-2 will continue to adapt to the human immune system and to a (partially) vaccinated population through mutations. How quickly this happens depends largely on the size of the actively infected population.
The more cases of infection - regional, national, and international - the more the coronavirus multiplies - and the more frequently mutations occur.
Compared to other viruses, however, the coronavirus mutates relatively slowly. With a total length of the Sars-CoV-2 genome of around 30,000 base pairs, experts assume one to two mutations per month. For comparison: Influenza viruses mutate two to four times as often in the same period.
How can I protect myself from coronavirus mutations?
You cannot specifically protect yourself against individual coronavirus mutations - the only option is not to become infected.
As a general rule, adhere to the rules of hygiene, keep your distance and wear your FFP2 mask in public. If you get vaccinated, you will also enjoy a good basic immunity against severe courses.
How are coronavirus mutations discovered?
Germany has a close-knit reporting system to monitor circulating Sars-CoV-2 viruses - it is called an "integrated molecular surveillance system". To this end, the relevant health authorities, the Robert Koch Institute (RKI), specialized diagnostic laboratories and the consulting laboratory for coronaviruses at the Berlin Charité work closely together.
How does the reporting system work if a mutation is suspected?
First of all, every professionally carried out positive coronavirus test is required to report to the responsible health authority.This includes coronavirus tests that were carried out in a test center, at your doctor's, in your pharmacy or at government facilities - such as schools. However, private self-tests are excluded from this.
Further information on coronavirus rapid tests for personal use can be found in our topic special Corona self-tests.
If the result is positive, doctors send the corresponding patient sample to a specialized diagnostic laboratory, which confirms the result using a PCR test. If the PCR test is also positive - the sample can also be sent to a sequencing laboratory where it can be further examined (sequencing genome analysis).
The RKI then compares the reporting data and the result of the sequence analysis in a pseudonymized manner. Pseudonymized means that it is not possible to draw any conclusions about a single person. However, this information forms the data basis for scientists and stakeholders in the health care system in order to obtain a precise overview of the current pandemic situation. This enables the best possible assessment of the situation in order to (if necessary) derive political measures.
What is a sequencing genome analysis?
A sequencing genome analysis is a detailed genetic analysis. She examines the exact sequence of the individual RNA components within the viral genome. This means that the Sars-CoV-2 genome, comprising around 30,000 base pairs, is deciphered and can then be compared with that of the coronavirus wild type.
Only in this way can the individual mutations be recognized at the molecular level - and an assignment within the "coronavirus family tree" possible.
Genome sequencing is a time-consuming and costly process with (very) limited capacities. So not every positive sample can be routinely sequenced. Experts make a preselection - so they take a sample.
This also makes it clear that not every country in the world is able to track the exact spread of certain coronavirus variants in detail. It is therefore likely that there is a certain lack of clarity in the available reporting data.
Tags: foot care interview smoking










.jpg)