Optic nerve inflammation
and Martina Feichter, medical editor and biologistMareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
An inflammation of the optic nerve (neuritis nervi optici, optic neuritis) can occur in the context of various diseases. It is closely linked to multiple sclerosis. The patient's eyesight is greatly reduced within a very short period of time. Optic nerve inflammation can often be treated well with medication if therapy is started in good time. Here you can read everything you need to know about optic nerve inflammation.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. H46
Optic nerve inflammation: description
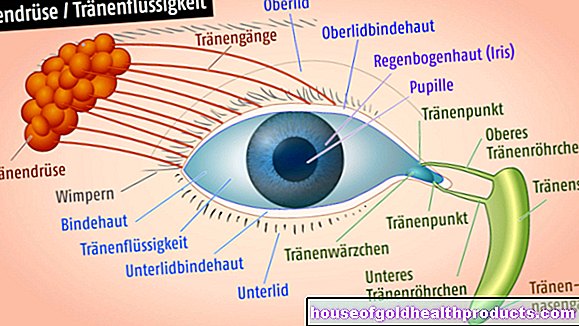
In the case of an inflammation of the optic nerve (neuritis nervi optici), the optic nerve that enables us to see is inflamed. It leaves the retina at the so-called papilla in the direction of the brain and there transmits the signals that are generated by the incidence of light on the retina. Optic nerve inflammation often affects both eyes in children; but otherwise it is usually one-sided.
Depending on where the inflammation occurs, a distinction is made between two forms of optic nerve inflammation - papillitis and retrobulbar neuritis:
- Papillitis (neuropapillitis optica): inflammation of the optic nerve in the eye in the area of the papilla. It is accompanied by swelling of the papilla.
- Retrobulbar neuritis: inflammation of the optic nerve behind the eye. The papilla is not swollen here. This form is the most common.
In addition, a distinction is made between typical and atypical forms of optic nerve inflammation, depending on the cause: The most common is typical optic nerve inflammation, which either occurs as part of multiple sclerosis or is of unknown cause. Atypical optic nerve inflammation has other causes (see below: Causes and Risk Factors).
Optic nerve inflammation: frequency
Typical optic nerve inflammation is the most common tendon disease in young adults. Most patients are between 18 and 45 years old. In principle, however, the disease can occur at any age.
The vast majority of patients are white. In western countries around four in 100,000 people develop typical optic neuritis every year. Women are 3.4 times more likely to be affected than men. More illnesses are registered in spring than in other times of the year - probably because the body releases less of the protective hormone melatonin in spring.
There is little epidemiological data on the frequency of atypical optic nerve inflammation. It is known, however, that this form of optic neuritis occurs more frequently among Afro-Caribbean and Asian people than among Europeans. In Germany, atypical optic nerve inflammation accounts for an estimated three percent of all cases. It is therefore much rarer than typical optic neuritis. Another difference: patients with atypical optic nerve inflammation are usually a little older (around 40 years).
Optic nerve inflammation: symptoms
Optic nerve inflammation primarily leads to a reduction in vision. Vision deteriorates drastically within a few hours or days. Visual acuity decreases significantly, especially in the central area of the visual field. The patients report that they see through a frosted glass or through a gray veil.
In most cases, there is also a dull pain in the eye, which increases with eye movements and pressure on the eyeball. Sometimes the pain is only perceived as a discomfort.
Another common symptom of optic nerve inflammation is color desaturation: colors are perceived as darker and duller.
In addition, about 30 percent of patients with optic nerve inflammation perceive flashes of light or other light phenomena (photopsia).
In so-called neuromyelitis optica (a form of atypical inflammation of the optic nerve), the Uthoff phenomenon can occur during or after the disease has progressed: The eyesight of the affected eye deteriorates as soon as the body temperature rises (e.g. through exercise or sauna).
In general, with atypical optic neuritis, symptoms other than those described here can occur.
Optic nerve inflammation: causes and risk factors
Causes of typical optic nerve inflammation
Typical optic nerve inflammation usually develops in the context of multiple sclerosis.In this autoimmune disease, the immune system attacks the protective layer (myelin sheath) of the nerve fibers, which impairs the transmission of nerve signals. An involvement of the optic nerve leads to an inflammation of the optic nerve. After a few weeks, the inflammatory activity subsides spontaneously and the visual function improves again. However, the damage to the optic nerve is usually not completely reversible.
In addition to the MS-related opicus neuritis, there is also typical optic nerve inflammation with an unknown cause (idiopathic).
Causes of atypical optic nerve inflammation
Depending on the mechanism of the disease, there are three groups of atypical optic nerve inflammation:
- Atypical optic nerve inflammation as a manifestation of an autoimmune disease such as neuromyelitis optica, sarcoid or lupus erythematosus
- atypical inflammation of the optic nerve that develops after infection (post-infectious) or vaccination (post-vaccinal)
- Atypical inflammation of the optic nerve that occurs as part of an infection (directly or indirectly triggered by the respective pathogen), e.g. in Lyme disease, syphilis or as neuroretinitis (a simultaneous inflammation of the optic nerve and retina, e.g. in the case of cat disease caused by Bartonella bacteria)
Rare causes are drugs (such as tamoxifen for breast cancer or ethambutol for tuberculosis) or poisoning (for example with alcohol, nicotine or lead).
Optic nerve inflammation: examinations and diagnosis
In order to be able to make the diagnosis of "optic nerve inflammation", your doctor will first ask you in detail about your medical history (anamnesis). He will ask you the following questions, among others:
- When did your vision deteriorate?
- Are eye movements causing you pain?
- Is vision worse on one side than on the other?
- Have you recently had a cold or a fever?
- Have any of your family members already had similar symptoms?
- Do you suffer from an underlying disease (e.g. multiple sclerosis, lupus erythematosus)?
- Do you have any known cases of multiple sclerosis in your family?
- Do you feel dizzy or have you noticed weaknesses in your muscles?
- Do you smoke, drink alcohol or take medication regularly?
- Are the symptoms worse when it is warm (for example, when taking a bath, sitting in the sauna, or doing sports)?
- Do you perceive flashes of light?
Investigations in optic nerve inflammation
This is followed by various eye exams.
Determination of visual acuity
Your visual acuity is determined with the help of a letter or number board attached at a certain distance. It is reduced in the case of an inflammation of the optic nerve. Low-contrast visual acuity is severely impaired in the acute phase and recovers more slowly than visual acuity and visual field.
Test of the pupillary reaction
After that, your doctor will take turns shining a small lamp into your eyes and watching the reaction of your pupils. Usually, both pupils narrow equally, regardless of which eye the doctor directs the light cone into.
In retrobulbar neuritis, however, what is known as a relative afferent pupil defect (RAPD) is often present. This means that the optic nerve of the affected eye does not conduct the incoming light signals into the brain as well as the other optic nerve. As a result, both pupils constrict less when the doctor directs the light onto the diseased eye and more when it shines into the healthy eye.
Examination of eye mobility
The doctor will also check the mobility of your eyes. For example, you should follow his finger or a pen with your eyes only (not with your whole head) and state whether the eye movements hurt you or you see double vision.
Determination of the field of view
Next, your visual field will be tested. This is the area of the environment that the eyes can see without moving your head. The visual field can be roughly checked with the examiner's fingers. The doctor moves his finger in different directions in front of your eyes and you have to let you know as soon as you see or no longer see the finger in your field of vision.
With a so-called perimeter, the visual field check can be carried out more precisely. Various points of light flash up, which you should recognize in your field of vision. In the case of optic nerve inflammation, there is often a restriction of the field of vision in the central area (central scotoma).
Examination of the fundus
The doctor then mirrors the fundus of your eye (funduscopy or fundoscopy). To do this, it shines into your eyes with an ophthalmoscope. So he can judge the retina. Among other things, he pays attention to changes in the blood vessels and the point where the optic nerve leaves the eye (papilla).
Fundoscopy is usually normal for retrobulbar neuritis. The papilla is changed in only about 30 percent of cases. In contrast, in papillitis, the papilla is typically red and swollen.
Examination of color perception
Your color perception is also tested. In the case of typical optic neuritis, the color saturation for red in particular is weakened.
Optic nerve conduction test
With the help of visually evoked potentials (VEP), the conduction speed of the optic nerve can be checked. In this measurement method, electrodes are attached to your head. After stimulating your optic nerve by showing pictures, the electrodes are used to measure which signals are arriving in the brain via the optic nerve and how quickly. If the optic nerve is inflamed, the measured values are often changed.
Optic nerve inflammation: advanced diagnostics
Once your doctor determines whether it is typical or atypical inflammation of the optic nerve, further tests will be done. With their help one wants to find out the cause of the neuritis nervi optici.
If a typical optic nerve inflammation occurs for the first time, the patient will develop multiple sclerosis (MS) in around 30 percent of cases over the next five years. To diagnose them, magnetic resonance imaging (MRI) is done of the head and spine. A cerebrospinal fluid puncture is also necessary: A sample of the cerebrospinal fluid (CSF) is taken from the lumbar spine through a thin hollow needle and examined for signs of inflammation that could indicate MS.
Atypical optic nerve inflammation can be caused by other diseases. For this reason, blood is often drawn in order to examine it for various pathogens or antibodies.
Optic nerve inflammation: Differentiation from other diseases
The doctor should also examine whether there is another condition that is causing symptoms similar to optic nerve inflammation. These differential diagnoses include the congestive papilla. It occurs when the intracranial pressure increases and causes similar symptoms, but usually does not impair vision to the same extent as optic neuritis.
Poisoning with alcohol, for example, can also present itself as an inflammation of the optic nerve. As a rule, however, it always occurs on both sides.
Possible differential diagnoses are also other eye diseases such as anterior ischemic optic neuropathy (AION; often in diabetes mellitus) and Leber hereditary optic neuropathy (LHON).
Optic nerve inflammation: treatment
Optic nerve inflammation is usually treated with high-dose glucocorticoids ("cortisone"). These have anti-inflammatory and immunosuppressive effects (suppressing immune reactions). Treatment makes the inflammation subside faster, but does not affect ultimate vision. The glucocorticoids are usually administered in the first few days as an infusion and then in tablet form, but sometimes only in tablet form. In both cases, the treatment can be slowly tapered off at the end by administering tablets in ever lower doses.
Because of the possible risks and side effects (such as stomach ulcers), high-dose cortisone treatment is often carried out as an inpatient. To protect the gastric mucosa, some patients receive special medication (e.g. proton pump inhibitors) during treatment.
If the optic nerve inflammation occurs in connection with a bacterial infection, the cortisone treatment should be supplemented with antibiotic therapy in the first few days.
Multiple sclerosis, sarcoid and other systemic diseases underlying optic neuritis may require further therapeutic measures.
When cortisone doesn't help
If (repeated) cortisone treatment does not improve the symptoms of optic nerve inflammation enough, in some cases plasmapheresis or immunoadsorption - two methods of blood washing (apheresis) - can be considered. During plasmapheresis, the blood plasma and its dissolved components (such as antibodies) are exchanged. During immune adsorption, specific soluble components of the immune system are filtered out of the blood. This can be helpful in treating autoimmune diseases.
In optic neuritis due to lupus erythematosus, if the cortisone therapy does not work, treatment with the immunosuppressant cyclophosphamide can be attempted.
Check-ups
A check-up should take place no later than two weeks after the first visit to the ophthalmologist. Further check-ups depend on the findings.
If the patient has a known underlying disease such as multiple sclerosis, long-term check-ups by the attending specialist (e.g. neurologist) are advisable.
Optic nerve inflammation: disease course and prognosis
A typical optic nerve inflammation usually heals within about five weeks with consistent treatment. However, color and contrast perception are usually somewhat limited in the long run.
The probability of developing an inflammation of the optic nerve again in the same or the other eye within ten years is on average 35 percent. On closer inspection, the following applies: If the first illness is associated with multiple sclerosis (MS), the risk of relapse is significantly higher at 48 percent. In contrast, in typical optic neuritis without developing MS, it is 24 percent.
The likelihood of optic nerve inflammation turning out to be the first sign of multiple sclerosis over time depends, among other things, on whether so-called demyelinating foci can be detected in the MRI. These are focal points on nerve fibers where the myelin sheath (also called myelin sheath) has been destroyed:
About 15 percent of all patients without demyelinating foci have developed MS five years after optic neuritis. If there is evidence of one or two demyelinating foci, this percentage is 35 percent. And if optic neuritis occurs for the first time with more than three demyelinating foci on the MRI, around half of those affected will develop MS within five years.
With atypical optic nerve inflammation, the prognosis with regard to vision is worse than with typical optic neuritis: the visual acuity of those affected is usually more impaired.
Regarding the course and prognosis of optic nerve inflammation, a distinction must be made between retrobulbar neuritis and papillitis. In principle, a check-up should be carried out by the doctor once a week for the first three weeks. After that, the time interval between the controls must be selected individually.
Tags: dental care nourishment parasites