Systemic lupus erythematosus
and Sabine Schrör, medical journalistMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts
Sabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.Systemic lupus erythematosus (SLE) is a form of the autoimmune chronic inflammatory disease lupus erythematosus. While other forms of lupus more or less only affect the skin, systemic lupus erythematosus also affects internal organs. The disease progresses in episodes and is usually chronic. Systemic lupus erythematosus belongs to the group of inflammatory rheumatic diseases, more precisely to the connective tissue diseases (collagenoses). Read more about SLE!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M32
Systemic lupus erythematosus: frequency
Between 20 and 50 out of 100,000 people in Europe are affected by systemic lupus erythematosus (SLE disease), in Germany around 36.7. Women are significantly more likely to develop this autoimmune disease than men; for Germany, a ratio of 4: 1 applies here.
SLE can break out at any time. The disease most often develops between the ages of 16 and 55. Basically, SLE is found much more often in people with Asian, African or Caribbean roots than in Europeans, for example.
Systemic lupus erythematosus: symptoms
Systemic lupus erythematosus can cause symptoms in various organs and organ systems. For example, blood vessels, skin, hair, lungs, heart, kidneys and / or joints can be affected. In addition, the disease can develop very differently from person to person. The clinical picture in SLE is correspondingly diverse.
First lupus symptoms
Systemic lupus erythematosus usually starts with general and unspecific symptoms. Symptoms such as tiredness and fatigue, decreased performance, fever and weight loss are the most common. Lymph node swelling is also observed in about half of the patients.
Lupus symptoms later
The lupus symptoms that occur in the further course depend on which organs and / or organ systems are affected by the disease:
- Skin and hair: In areas of skin that are exposed to the sun (such as the cleavage, face), rashes can suddenly or slowly develop. The reddening of the skin in the shape of a butterfly, which increases when exposed to sunlight, is typical. Other possible lupus symptoms are inflammation of the oral mucosa and circular hair loss.
- Vessels: The first symptoms of lupus can be "vascular cramps" in the fingers with a whitish-bluish discoloration as a reaction to cold temperatures (Raynaud's syndrome). Another possible sign of SLE is inflammation of the small blood vessels (vasculitis). It causes small, punctiform or patchy hemorrhages in the skin, for example on the lower legs, hands or mucous membranes (especially in the mouth). If the blood vessels at the back of the eye become inflamed, blurred vision and visual field defects occur.
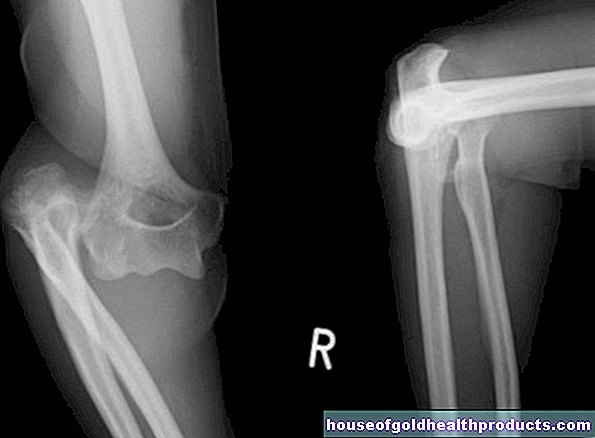
- Joints: Very common lupus symptoms are pain, swelling and / or deformation of the joints (especially the small joints). The joint pain usually occurs in the morning. Tendon sheaths are also often affected by the inflammatory changes.
- Muscles: If SLE affects the muscles, muscle inflammation (myositis), muscle pain and muscle wasting (muscle atrophy) occur.
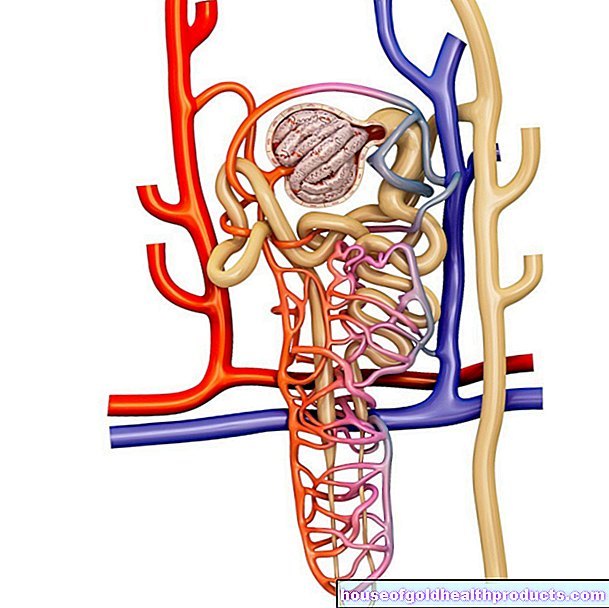
- Kidneys: About half of all lupus patients develop inflammation of the kidneys (lupus nephritis). It manifests itself with protein in the urine (proteinuria) and possibly water retention in the tissue (edema). The inflammation can worsen kidney function - up to and including kidney failure. Those affected are then dependent on regular blood washing (dialysis).
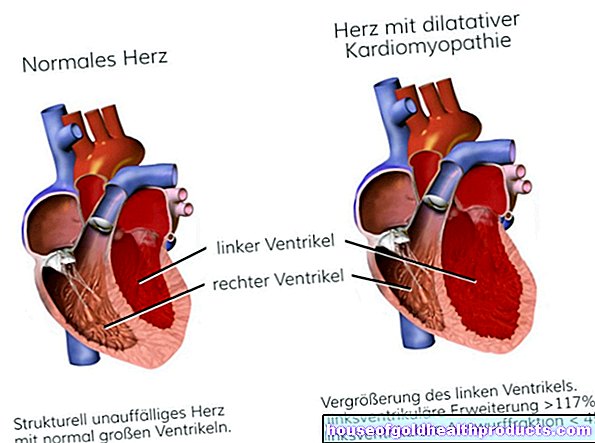
- Lungs and heart: three out of four lupus patients develop pleurisy (pleurisy). It is accompanied by severe pain when breathing. Inflammatory changes in the heart area (such as myocarditis, pericarditis) are possible lupus symptoms.
- Abdominal area: Some lupus patients develop inflammation of the peritoneum (peritonitis). Signs of this include stomach pain, nausea, and vomiting.
- Central nervous system: The brain is affected in around ten to 15 percent of lupus patients. Then epileptic seizures, migraine-like headaches, concentration and memory disorders, psychological changes (such as depression, psychosis) as well as uncontrolled tremors and convulsions can occur.
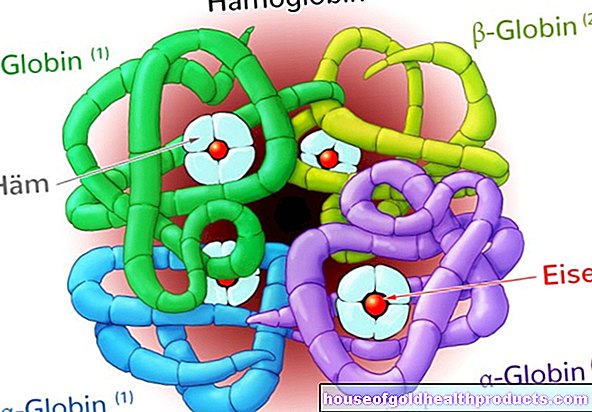
- Blood count: About half of the patients have low white and / or red blood cell counts, and sometimes platelet counts as well. Possible consequences are anemia and an increased tendency to bleed.
Flare-ups in systemic lupus erythematosus are most often accompanied by fever, fatigue, and joint and muscle pain. As far as the affected organs are concerned, symptoms of lupus in the episode appear mainly in the area of the skin and joints, i.e. with reddening of the skin and joint pain.
Systemic lupus erythematosus: causes
It is unclear exactly what causes systemic lupus erythematosus. However, several factors appear to be involved, most notably genetic changes. In combination with external factors that stress or stimulate the immune system, systemic lupus erythematosus can then break out. In addition, such factors can worsen an existing disease flare-up. These include:
- Virus or bacterial infections
- intense sun exposure
- extreme climate change
- extreme mental stress
- hormonal changes (e.g. during puberty, pregnancy and menopause)
Systemic lupus erythematosus: diagnosis
Diagnosing systemic lupus erythematosus can be difficult because the disease often begins slowly. In addition, the symptoms are so diverse and often unspecific that they can also indicate other diseases. In addition, systemic lupus erythematosus is relatively rare and therefore little known. To make matters worse, in addition to the "pure" lupus disease, there are also mixed forms with other rheumatic diseases.
If “systemic lupus erythematosus” is suspected, patients should be examined by a specialist, i.e. a rheumatologist or pediatric rheumatologist. Because of the wide range of symptoms, it makes sense to work with other specialists, for example with a dermatologist, a heart and kidney specialist or a gynecologist. The extensive examinations that are necessary for the diagnosis of "systemic lupus erythematosus" can also be carried out on an in-patient basis in the hospital (for example on children).
Conversation and physical examination
The doctor will first have a detailed discussion with the patient (in the case of children with the parents) about the medical history (anamnesis). This is followed by a physical examination.
Blood test
Various laboratory tests, some of which are very specific, help diagnose “systemic lupus erythematosus”. A blood sample from the patient is examined for certain antibodies. These antibodies are defense substances that are directed against the genetic material (DNA). Doctors also refer to them as antinuclear antibodies (ANA). Different types of these antibodies can be detected in the blood, which the doctor can use to identify a lupus disease.
Furthermore, the blood test often shows a lack of white blood cells (leukocytes) and blood platelets (thrombocytes) and anemia (anemia). The rate of sedimentation of the blood cells (ESR) is often accelerated.
Further investigations
Numerous other examinations allow the doctor to assess the extent of systemic lupus erythematosus and the involvement of individual organs. For example, increased blood pressure and protein in the urine can indicate involvement of the kidneys in terms of kidney inflammation (lupus nephritis). Further examinations such as an ultrasound of the kidneys can confirm the suspicion.
Depending on the symptoms, x-ray examinations, for example, are also carried out, the fundus is examined and / or the lung function is checked.
The catalog of criteria simplifies the diagnosis
Because systemic lupus erythematosus can trigger so diverse and often difficult to interpret symptoms, American rheumatologists have created a catalog of criteria to simplify the diagnosis. Accordingly, SLE is suspected if four out of eleven symptoms are present. These include, for example, butterfly-shaped skin reddening on the face, repeated ulcers in the mouth without any other cause, unexplained swelling of the joints, pleurisy or pleurisy, pericardial inflammation and the detection of certain antibodies.
Systemic lupus erythematosus: treatment
Systemic lupus erythematosus cannot be treated causally - neither in children nor in adults. Only symptomatic therapy is possible, i.e. treatment of the symptoms of the disease. To this end, doctors create an individual therapy plan for each patient - depending on which organs are affected how severely and how active the disease is.
Medication
The aim of treating SLE disease is to reduce inflammation and excessive activity of the immune system. There are four different substance groups available for this:
- Non-steroidal anti-inflammatory drugs (NSAIDs): If systemic lupus erythematosus is only mild, such anti-inflammatory drugs are often sufficient. They also have an analgesic and fever lowering effect and prevent blood platelets from clumping together.
- Glucocorticoids ("cortisone"): They have a strong anti-inflammatory effect and are often given in high doses over a short period of time in acute disease flare-ups (shock therapy or pulse therapy).
- Immunosuppressants: They reduce the activity of the immune system, which is overactive in SLE. Examples are azathioprine, cyclosporine and cyclophosphamide.
- Chloroquine: This active ingredient is mainly prescribed when systemic lupus erythematosus affects the skin and joints. It is also suitable as an alternative to cortisone in the case of mild disease.
Accompanying measures
The drug treatment of lupus can be supplemented by other measures. These include physical therapies (such as cold applications for swollen, painful joints or breathing therapy for breathing difficulties), lowering blood pressure (e.g. with medication) and avoiding sunlight.
Systemic lupus erythematosus: course and prognosis
Systemic lupus erythematosus is usually chronic and relapsing. Months or years can pass between two consecutive flare-ups. In many patients, the relapses also become rarer and weaker over time - so SLE can decrease with age.
Systemic lupus erythematosus is curable neither in children nor in adults. The disease can be kept in check with the help of various drugs, so that as few inflammatory processes as possible occur in the body. The earlier SLE is treated, the better the course of the disease can be influenced. In most cases, patients must be treated for life.
Life expectancy
SLE patients in Germany now have a normal life expectancy.However, the quality of life of many patients is limited: those affected suffer from constant fatigue, skin changes and infections or are dependent on regular blood washing (dialysis). The most common cause of death in people with systemic lupus erythematosus is no longer the disease itself - most patients die from complications of the disease.
Complications
Systemic lupus erythematosus can cause serious and sometimes life-threatening complications:
- Kidney inflammation: Over time, it can cause kidney function to decline (kidney failure) or to be completely lost (kidney failure). Those affected then need regular blood washing (dialysis) or a kidney transplant.
- Cardiovascular diseases: Systemic lupus erythematosus promotes vascular calcification (arteriosclerosis) and thus cardiovascular diseases such as heart attacks and strokes.
- Inflammation of the spinal cord: it causes paralysis of the legs and (less often) the arms and can lead to paraplegia if not treated quickly.
- Inflammation of the optic nerve: If an optic nerve inflammation is not discovered and treated in time, there is a risk of blindness.
- increased risk of infection: SLE patients are particularly susceptible to infections with viruses, bacteria and fungi. If these are not treated consistently, there is a risk of organ damage.
- increased susceptibility to malignant diseases (cancer)
Systemic lupus erythematosus: prevention
Systemic lupus erythematosus cannot be prevented - the causes of the chronic inflammatory autoimmune disease are not yet known. However, several factors have been identified that can trigger a disease flare-up. To prevent an SLE attack, you should take the following advice to heart:
- Avoid being overweight
- do not smoke
- Drink alcohol in moderation
- eat a balanced, low-fat diet
- Exercise regularly and exercise in moderation (also with complaints such as joint pain)
- Do not stay unprotected in the sun or under artificial UV light (use sunscreen with a high sun protection factor!)
- Avoid sources of infection, especially when taking immunosuppressants (these make you more susceptible to infections)
Psychological factors also influence the course of the disease. Chronic diseases such as systemic lupus erythematosus can depress mood and make you feel depressed. This in turn triggers stress, which in the long term can negatively affect the hormonal balance, the immune system and thus also the course of the disease.
A positive attitude towards life is therefore very important for patients. Relaxation techniques (biofeedback, autogenic training, etc.) and / or talking to a psychologist are helpful here. A visit to a self-help group “Systemic Lupus Erythematosus” can also be useful.
Tags: magazine prevention skin care