Oral mucosa - important diseases
All content is checked by medical journalists.The most common diseases of the oral mucosa include aphthae and oral thrush. Find out here how these diseases develop, how they can be recognized and what can be done about them!
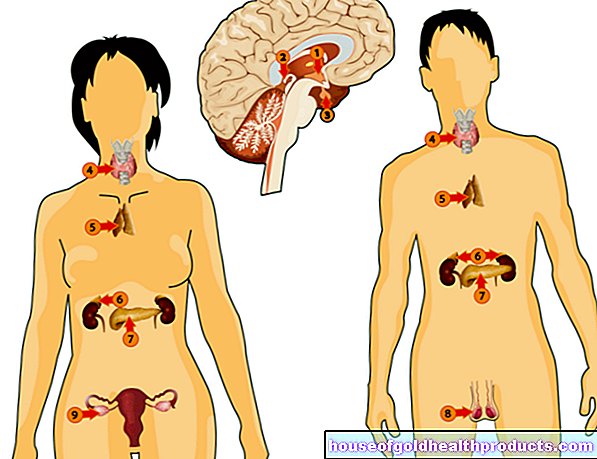
Balance of microorganisms
The oral cavity is not a sterile place. Fungi, viruses and bacteria can be found on the mucous membranes, tooth surfaces and in saliva. Most of these microorganisms are part of a healthy oral flora and are responsible for certain metabolic processes. They also prevent colonization with pathogens:
In a healthy body there is a balance between the "good" and "bad" germs. Cold, other pathogens, antibiotics, stress, serious illnesses and bad eating habits can shift this balance in favor of pathogens.
Possible changes
Not all diseases of the oral mucosa are recognizable to the layman. But some make themselves noticeable with clear changes. Then you should definitely visit your dentist! Because every thorough examination at the dentist includes not only an examination of the teeth but also an examination of the soft tissues and mucous membranes.
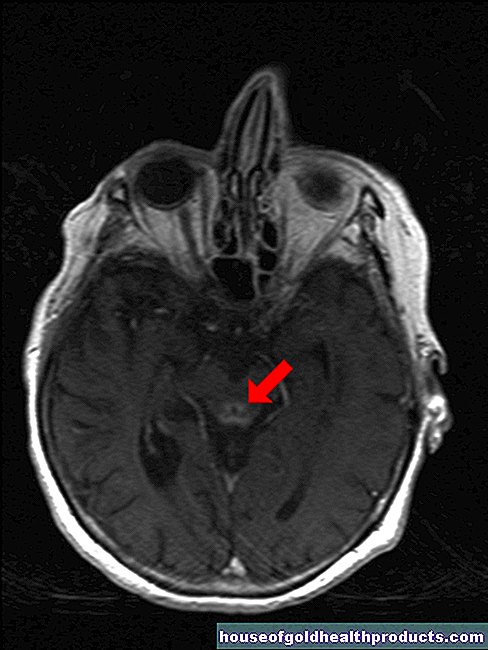
The most common inflammations of the oral mucosa are aphthae and oral thrush. There are also forms of cancer that occur in the oral cavity. Early detection is important here. Regular check-ups can reveal malignant changes at an early stage.
Aphthous ulcers
Aphthae are round (as if punched out), yellowish-white colored mucous membrane ulcers with a reddish inflamed area. They cause pain when they come into contact with acidic foods such as vinegar or sour fruits. There are three forms:
- The most common is the minor type with a few, two to five millimeter large mucosal ulcers, which predominantly occur in the front third of the oral cavity.
- The major type with a few ulcers over one centimeter in size is less common. They reach much deeper into the tissue and cause more discomfort. They are often accompanied by enlarged, tender lymph nodes.
- The herpetiform type with many, very small, herpes-like aphthae is rarest.
Individual aphthae can merge to form larger foci of inflammation. If a large part of the oral mucosa is affected, experts call it aphthous stomatitis. It makes chewing and swallowing very painful and takes significantly longer than a week to heal.
Why do aphthae develop?
The cause of the aphthous ulcers is unknown. Mineral and vitamin deficiencies, allergic factors, infections and hormonal fluctuations are discussed as triggers.
The infection theory is supported by the fact that disinfectants and antibiotics sometimes accelerate healing. Otherwise, the old ENT and dentists' slogan applies to aphthae: "With a disinfectant it takes a week to improve, without treatment eight days". This applies primarily to the minor type that is most widespread.
What can be done against aphthous ulcers?
So in most cases it means: take care of the sore spot and otherwise wait. For example, special pain relieving mouthwashes can be used to alleviate the symptoms. If there is a proven vitamin or mineral deficiency (such as iron or folic acid deficiency), appropriate preparations can be useful.
Aphthae can recur or more pronounced when the immune system is weakened by chronic diseases (such as diabetes). In the case of chronically recurring aphthae, the doctor may recommend a local treatment with a corticosteroid gel ("cortisone") alternating with antiseptic mouthwashes.
Oral thrush
Oral thrush is a fungal infection of the lining of the mouth. Candida yeasts are responsible for this. They are found in the saliva of almost everyone. If their growth takes over, however, a whitish coating forms on the mucous membrane. It can usually be scraped off relatively easily with a toothbrush or a scraper - except if it is more pronounced with thicker plaques or large, thick coverings.
The fungi multiply best on the rough surface of the tongue, in gum pockets and under ill-fitting dentures. The fungal lawn can also spread over the entire oral cavity. Often it is accompanied by bad breath.
Who is prone to oral thrush?
Children and the elderly have the highest risk of fungal infections of the oral cavity - especially if they have chronic diseases that affect the immune system (such as leukemia, HIV, diabetes). Certain drugs also promote thrush, especially antibiotics, cytostatics (cancer drugs) and agents that suppress the immune system (immunosuppressants).
How is oral thrush treated?
Thrush can be treated with antifungal agents (antimycotics) such as nystatin: The agents are applied locally (e.g. as a gel or lozenge) and work directly on site. Treatment with drugs that work throughout the body (systemic) is only necessary in severe exceptional cases and if there is an additional fungal attack in other parts of the body.
Therapy requires patience: it can take a few weeks for the fungi to disappear from the oral cavity.
If there is an increased risk of a pronounced fungal attack in the oral cavity, antimycotics are also taken preventively. This applies to prolonged antibiotic therapy or local radiation therapy in the mouth and throat area (for example in the case of tumors of the tongue, throat or larynx).
Brush your teeth, rinse your mouth
All people who are prone to recurring mouth infections or aphthae should brush their teeth particularly thoroughly and gargle with an antibacterial solution before going to sleep. Ask your dentist for specific suggestions.
The best way to protect yourself from a fungal attack on the tongue is to regularly clean the back of the tongue with a special tongue scraper. It is very flat and is less likely to trigger a gag reflex than a toothbrush.
Tags: unfulfilled wish to have children medicinal herbal home remedies eyes