shock
and Sabine Schrör, medical journalistMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.A medical shock is characterized by an inadequate supply of oxygen: the oxygen supply cannot meet the oxygen demand. Then only the vital organs are adequately supplied with blood and thus oxygen - at the expense of the periphery (limbs). If the lack of oxygen continues to worsen, the organs will ultimately no longer receive sufficient oxygen - there is a danger to life! Read everything you need to know about shock here!

Brief overview
- What is a shock? Relocation of the blood volume to the center of the body in the event of a lack of oxygen to supply the vital organs. As a result, limbs (periphery) and - if the lack of oxygen progresses - later also the organs with oxygen.
- Types of shock: Depending on the trigger, a distinction is made between hypovolemic, cardiogenic, anaphylactic and septic shock. Special forms are neurogenic and hypoglycemic shock.
- Causes: In hypovolemic shock, e.g. severe blood loss, lack of fluids (e.g. severe diarrhea). In the case of cardiogenic shock, e.g. heart attack, heart valve constriction, injuries or diseases of the lungs. In the case of anaphylactic shock, allergens such as insect venom or medication. Septic shock e.g. after infections (such as wound infection).
- Symptoms: restlessness, fear, pallor, tremors, freezing, chills, cold sweats. With some forms of shock: warm, reddened skin. With advanced shock: apathy, unconsciousness.
- First aid measures: Call the emergency doctor immediately (acute danger to life!). Until this arrives: Shock position with legs raised (except for cardiogenic shock: here upper body lie higher), calm the patient, if necessary heart massage and mouth-to-mouth resuscitation.
- Treatment: After the immediate measures, further treatment depending on the type of shock, e.g. medication or infusions to increase blood volume, blood reserves, pain relievers, oxygen supply, medication to increase the contraction force of the heart, antiallergics, antibiotics.
Shock: description

Put simply, in the event of a shock, the blood volume is increasingly shifted to the center of the body: the vessels in the periphery of the body, i.e. in the arms and legs, narrow so that less blood can circulate there. This makes more blood available for the internal organs and the brain. This phenomenon is known as "centralization". The shock is therefore an emergency program of the body that aims to maintain the blood supply and thus the functionality of the vital organs.
The shock - a vicious circle
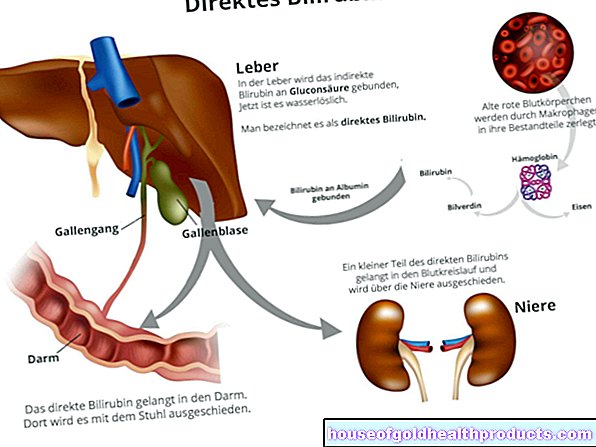
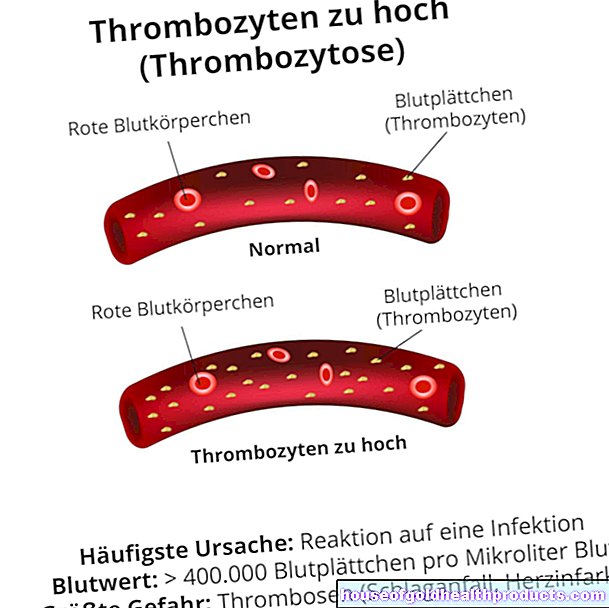
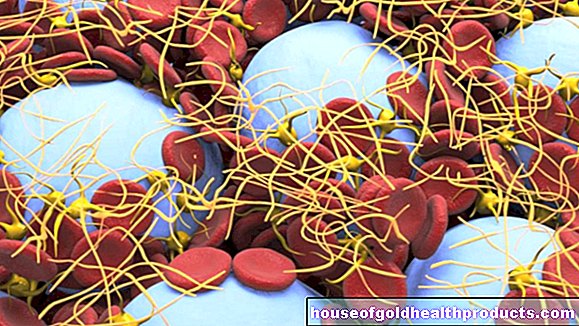
So a shock makes perfect sense - but only at first glance! This is because the metabolism changes in the low-blooded, oxygen-poor body periphery, with acidic metabolic products being created. These cause more fluid to escape from the smallest vessels (capillaries) into the tissue, and the arterioles (small, blood-supplying vessels) to widen. Their counterparts, the venules, on the other hand, dilate less. Therefore, they cannot completely drain the blood that has been enriched with carbon dioxide from the tissue - blood congestion occurs. Small blood clots (microthrombi) form in them. In addition, even more fluid flows into the tissue. The amount of blood circulating in the periphery continues to decrease, and the tissue is supplied with even less oxygen - a vicious circle that medical professionals refer to as a shock coil.
If left untreated, this spiral continues to turn, with increasingly fatal consequences. In extreme cases, the formation of microthrombi can consume important substances in the blood that are responsible for blood clotting (consumption coagulopathy). This can lead to more bleeding in the body. Over time, vital organs are no longer adequately supplied with blood or oxygen. Then the cycle breaks down - multiple organ failure occurs.
Few people survive multiple organ failure. It is therefore important to intervene as early as possible in the event of a shock.
Depending on the triggering cause, a distinction is made between different types of shock:
Hypovolemic shock
The hypovolemic or volume deficiency shock is triggered by severe fluid loss, for example after severe internal or external bleeding (hemorrhagic shock), severe diarrhea or vomiting. There are three stages:
- Stage 1: The blood pressure is normal, the skin is pale and damp and cool.
- Stage 2: The blood pressure drops (below 100 mmHg systolic), the pulse rises to more than 100 beats per minute.
- Stage 3: The blood pressure continues to fall (below 60 mmHg), the pulse becomes flatter and can hardly be felt. In addition, there are impaired consciousness, urinary retention and shallow, rapid breathing.
Cardiogenic shock
Cardiogenic shock originates in the heart. If this is damaged as a result of a heart attack, for example, it lacks the strength to pump sufficient blood into the circulation. Then after a while the spiral of shock sets in. An effusion or hemorrhage in the pericardium as well as a pulmonary embolism can reduce the performance of the heart and thus set the shock spiral in motion.
Anaphylactic shock
The shock is due to an extremely exaggerated allergic reaction of the immune system: In the case of an allergy, the immune system incorrectly interprets certain substances (allergens) in food, medicines or insect venom as dangerous. When it comes into contact with these substances, it releases messenger substances that expand the blood vessels and allow fluid to escape from the capillaries. As a result, the blood volume decreases and the shock coil begins to turn.
Septic shock
Septic shock is triggered by a local or whole body infection. As with anaphylactic shock, messenger substances (mediators) are released here too, which dilate the blood vessels and allow fluid to escape into the tissue. A special form of septic shock is toxic shock syndrome (TSS): Here the immune system reacts to toxins that are produced by invading bacteria.
Special shock forms
There are also some special forms of shock, for example:
- Neurogenic shock: Here part of the nervous system fails so that the blood vessels can no longer constrict and the circulation breaks down. Liquid can also escape in an uncontrolled manner.
- Hypoglycemic shock: If the sugar concentration in the blood falls below a critical limit (around 50 mg / dl), the patient suddenly becomes unconscious because the brain is no longer adequately supplied with energy.
Shock: symptoms
Important signs of shock include:
- Skin changes: pale, cold sweaty skin in hypovolemic and cardiogenic shock; reddened, hot skin in septic shock; pale, warm, dry skin in neurogenic shock; allergic skin symptoms in anaphylactic shock (reddening, overheating, itching, possibly swelling)
- Drop in blood pressure
- Palpitations (tachycardia), exception: in the case of neurogenic shock and certain cardiac arrhythmias, the heartbeat is significantly slowed down (bradycardia).
- barely palpable pulse
- accelerated breathing, subjectively difficult breathing
- Restlessness, nervousness, fear, tremors
- Disturbances in consciousness in advanced shock, e.g. apathy, unconsciousness
In children, an unexplained palpitations is often the earliest symptom of shock. A drop in blood pressure and breathing disorders, on the other hand, usually only occur later.
Shock: causes
Depending on the type of shock, different causes come into question. Important: These causes do not always result in shock!
Causes of Hypovolemic Shock
Hypovolemic shock is due to excessive loss of blood from the vessels. Possible triggers are:
- Heavy bleeding, e.g. after injuries to blood vessels or organs, after bone fractures, operations or childbirth (heavy secondary bleeding), with reduced blood clotting due to diseases (hemophilia) or blood-thinning drugs (e.g. coumarins, heparin)
- Fluid deficit, for example due to prolonged vomiting or severe diarrhea. Even if you keep drinking too little, the blood volume can decrease dangerously.
Causes of Cardiogenic Shock
If the heart is too weak to pump enough blood into the circulation, it can result in cardiogenic shock. Reasons for the inadequate cardiac output are, for example:
- Weak contraction of the heart, for example due to a heart attack, an inflammation of the heart muscle or abnormal development of the heart muscle. The heart cannot then contract properly and therefore cannot generate enough pressure in the blood vessels.
- Excess supply of blood, for example when a heart valve does not close properly. During the filling phase, blood then flows from the aorta or the lungs back into the corresponding heart chamber and fills it excessively.
- Heart valve constriction (like aortic valve stenosis): Here the heart has to pump against increased resistance. The strong pressure load damages the heart muscle, at the same time less blood gets into the vessels due to the smaller diameter of the valve opening.
- Narrowing of the pericardium due to an effusion, bleeding (pericardial tamponade) or inflammation-related (constrictive pericarditis). Then the heart chambers can no longer fill sufficiently, which reduces the heart's pumping capacity.
- Injuries or diseases of the lungs can impede venous return to the heart. The possible consequence is reduced cardiac output, which can lead to cardiogenic shock.
Causes of Allergic Shock
The cause of allergic (anaphylactic) shock is an excessive reaction of the immune system. The triggers are individual allergens, i.e. substances to which the person concerned has an allergic reaction, for example:
- Insect venom (bee or wasp venom)
- Food like nuts, stone fruits or strawberries
- Medicines, e.g. pain relievers, anesthetics or antibiotics (especially penicillins)
Causes of Septic Shock
Septic shock is caused by an infection (e.g. bacteria or fungus). This can be local or affect the entire body. The following factors can cause septic shock:
- Inflammations: Inflammation of the peritoneum (peritonitis), inflammation of the pancreas (pancreatitis), inflammation of the gallbladder (cholecystitis), inflammation of the kidneys (pyelonephritis) or pneumonia.
- Catheters (venous catheters, urine catheters, etc.): Pathogens can enter the body through them and cause sepsis, in the worst case with shock.
- severe, extensive burns: The wounds can become infected and even lead to septic shock.
- weakened immune system: it promotes septic shock.
Septic shock is particularly dangerous,
- caused by meningococci (causing meningitis),
- which occurs as part of a Waterhouse-Friderichsen syndrome (acute failure of the adrenal glands) or
- which occurs in people who have had their spleens removed.
First aid in case of shock
If you suspect a shock, please call the emergency services immediately!
Until the emergency doctor arrives, you should definitely provide first aid:
- If the person concerned (adult or child) is conscious, put them in shock. To do this, lay it flat, but place your legs higher than your upper body. This will make it easier for the blood to flow to the heart.
If a cardiogenic shock is suspected, on the other hand, the upper body must be raised so that the heart is not additionally stressed.
- Avoid any additional excitement for the person concerned.
- Calm down the victim.
- Keep the patient warm with a thermal blanket or foil to prevent them from cooling down due to the shock.
- Stop bleeding to prevent further blood loss.
- In the event of unconsciousness or cardiovascular arrest, take the appropriate first aid measures: clear the airways, if necessary, mouth-to-mouth resuscitation, cardiac massage.
- If you are unsure about the patient's condition, but your heartbeat and breathing are stable, the stable side position is the best solution.
- Make sure to stay with the person affected and check your breathing and pulse regularly until the emergency doctor arrives and treats the shock.
Shock: diagnosis and treatment
First of all, it is important to recognize a shock as such. For this it is important to inform the (emergency) doctor about previous, relevant events: For example, did the person concerned eat something special shortly beforehand, was they bitten by an insect or is they known to have a heart disease? Has there been an accident, an operation or an infection in the recent past? These are important questions that can help the doctor diagnose. The typical shock symptoms provide further information (see above).
In addition, there are various signs that can be used to quickly identify shock:
- Shock index: it is an important indicator. The pulse rate is divided by the systolic blood pressure value (the first value when measuring blood pressure). If the result is greater than 1 (i.e. if the pulse value exceeds that of the blood pressure), this indicates a shock. In the early stages of a shock, however, the value can still be below 1.
- Fingernail test: This involves pressing a fingernail until the nail bed underneath is bloodless and white. Shortly after letting go, the nail bed should turn red again. If this lasts longer than a second, it indicates a disturbed peripheral blood flow and thus a shock.
- Sunken neck veins (jugular veins) and tongue floor veins are typical signs of hypovolemic shock.
In addition, the following examinations are carried out if shock is suspected:
- Electrocardiography (EKG)
- Measurement of central venous pressure
- Measurement of the amount of urine produced (diuresis)
- Determination of various blood values (such as oxygen saturation)
Shock therapy
After the first aid measures described above, the attending physician initiates appropriate treatment depending on the cause of the shock:
- Hypovolemic shock: Here, in particular, the lost blood volume must be replaced.This is done with the help of so-called isotonic crystallines (table salt or glucose) as well as with colloidal infusion solutions, i.e. blood volume-increasing solutions with macromolecules such as carbohydrates (hydroxyethyl starch, dextrans) or proteins (gelatine or human albumin). If necessary, the patient is also given blood.
- Cardiogenic shock: If necessary, it is treated with pain relievers and drugs that increase the force of contraction of the heart (dobutamine). In addition, oxygen is supplied to improve the supply of tissue and heart muscle. In the event of a heart attack, doctors will try to clear the clogged coronary artery again.
- Anaphylactic shock: The patient receives medication against the excessive reaction of the immune system (glucocorticoids, antihistamines). In addition, there are active ingredients that constrict the widened blood vessels (adrenaline) and widen the cramped bronchi (beta-2 mimetics). A volume replacement may also be necessary here.
- Septic shock: the causative pathogens are fought with suitable drugs (e.g. antibiotics against bacteria). In addition, patients often need volume replacement and possibly vasoconstricting medication in order to overcome the shock.