Dyspnea
and Martina Feichter, medical editor and biologistMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Anyone who suffers from dyspnea (shortness of breath, shortness of breath) is literally “breathed”. Despite increased breathing, those affected have the feeling that they are not getting enough air. Not only is this uncomfortable, but it can even cause fear of suffocation and death. The cause of dyspnea can be in the lungs or the airways, but it can also be completely different. A doctor can find this out with various tests. Read everything you need to know about the symptom "dyspnea" here.

Brief overview
- What is dyspnea? Shortness of breath or shortness of breath. It can occur acutely or chronically, also exist at rest or only show up under stress. Depending on the cause, other symptoms such as cough, palpitations, chest pain or dizziness may occur.
- Causes: foreign bodies in the respiratory tract, asthma, COPD, pseudocroup, diphtheria, epiglottis, vocal cord paralysis, glottic spasms, pneumonia, pulmonary emphysema, pulmonary embolism, pulmonary fibrosis, pneumothorax, pleural effusion, pulmonary artery disease, tumors, cardiac hypertension, heart disease Bruised ribs, broken ribs, scoliosis, diaphragmatic paralysis, amyotrophic lateral sclerosis, polio, sarcoid, hyperventilation, depression, stress, anxiety disorders.
- Examinations: Listening to the lungs and heart using a stethoscope, blood tests, lung function test, lung specimen, imaging procedures (such as X-rays, computer or magnetic resonance tomography)
- Treatment: depending on the cause, e.g. antibiotics for bacterial infections, cortisone and expectorants for croup, cortisone and bronchodilators for asthma and COPD, removal of the tumor and, if necessary, radiation or chemotherapy for cancer, etc.
Dyspnea: description

Dyspnea is initially a subjective feeling. The person concerned has the feeling that they cannot get enough air. In response, he begins to breathe harder - the breathing rate increases (usually around 15 to 20 puffs per minute). At first the breaths are still deep. The faster the patient breathes, however, the shallower the breaths become - shortness of breath occurs.
Forms of dyspnea
Doctors can characterize dyspnea more precisely using various criteria, such as the duration or the main situations in which it occurs. Some examples:
Depending on the duration of the shortness of breath, a distinction is made between acute and chronic dyspnea. An acute shortness of breath can be caused, for example, by an asthma attack, a pulmonary embolism, a heart attack or a panic attack. Chronic dyspnea can be observed, for example, in cardiac insufficiency, COPD or pulmonary fibrosis.
If the shortness of breath occurs even at rest, there is rest dyspnea. If someone is only breathless during physical exertion, one speaks of exertional dyspnea.
If the shortness of breath mainly becomes noticeable when lying flat, but improves when sitting or standing, it is orthopnea. For some people it is even more difficult: the shortness of breath torments them especially when they lie on their left side and less when they lie on their right side. This is then a trepopnea.
To a certain extent, the counterpart to orthopnea is platypnea: It characterizes shortness of breath that occurs preferentially in an upright posture (standing, sitting).
In speech dyspnea, the flow of speech is restricted or interrupted by the shortness of breath. The person concerned only brings out sentence fragments or individual words.
Sometimes the form of the dyspnea already gives the doctor clues as to the underlying cause. For example, trepopnea is typical of various heart diseases.
Dyspnea: causes and possible diseases
Dyspnea can have many different causes. Some of them lie directly in the area of the upper or lower airways (e.g. inhaled foreign bodies, pseudocroup, asthma, COPD, pulmonary embolism). In addition, various heart conditions and other illnesses can be associated with shortness of breath. Here is an overview of the main causes of dyspnea:
Causes in the respiratory tract
Often the cause of shortness of breath is that the airflow in the upper or lower airways is obstructed. Possible reasons for this are:
- Foreign bodies or vomit: If a foreign body is "swallowed" and gets into the windpipe or bronchial tubes, acute shortness of breath up to attacks of suffocation can result. The same thing can happen if, for example, vomit gets into the airways.
- Angioedema (Quincke's edema): This is a sudden swelling of the skin and / or mucous membrane. In the area of the mouth and throat, such swelling can cause shortness of breath or even attacks of suffocation. Angioedema can be caused by allergies, but it can also be triggered by various diseases and medications.
- Pseudo croup: This respiratory infection, also known as croup syndrome, is usually triggered by viruses (such as rhinitis, flu or measles viruses). The mucous membrane in the upper airways and at the larynx outlet swells. Whistling breath noises and barking coughs are the consequences. In severe cases there is also shortness of breath.
- Diphtheria ("real croup"): This bacterial respiratory tract infection also causes the mucous membrane of the upper respiratory tract to swell. If the disease spreads to the larynx, barking coughs, hoarseness and, in the worst case, life-threatening dyspnea result! Thanks to vaccination, diphtheria is now rare in Germany.
- Epiglottitis: Epiglottitis is a bacterial, life-threatening inflammation of the epiglottis. Typical symptoms are fever, shortness of breath and increased salivation. If you suspect an epiglottitis, you have to call the emergency doctor immediately!
- Paralysis of the vocal cords: Bilateral vocal cord paralysis is another possible cause of dyspnea. It can occur through nerve injuries as a result of an operation in the neck area or nerve damage as part of various diseases
- Glottic cramp (glottic cramp): The larynx muscles suddenly cramp and thus narrow the glottis - shortness of breath occurs. If the glottis is completely closed by the spasm, there is an acute danger to life! Glottic spasm occurs mainly in children. It can be triggered by irritants in the air you breathe (such as certain essential oils).
- Bronchial asthma: This chronic respiratory disease is very often the reason for sudden breathlessness. In the event of an asthma attack, the airways in the lungs temporarily narrow - either triggered by allergens such as pollen (allergic asthma) or, for example, by physical exertion, stress or the cold (non-allergic asthma).
- Chronic obstructive pulmonary disease (COPD): COPD is also a widespread chronic respiratory disease that is associated with narrowing of the airways in the lungs. In contrast to asthma, this narrowing is permanent. The main cause of COPD is smoking.
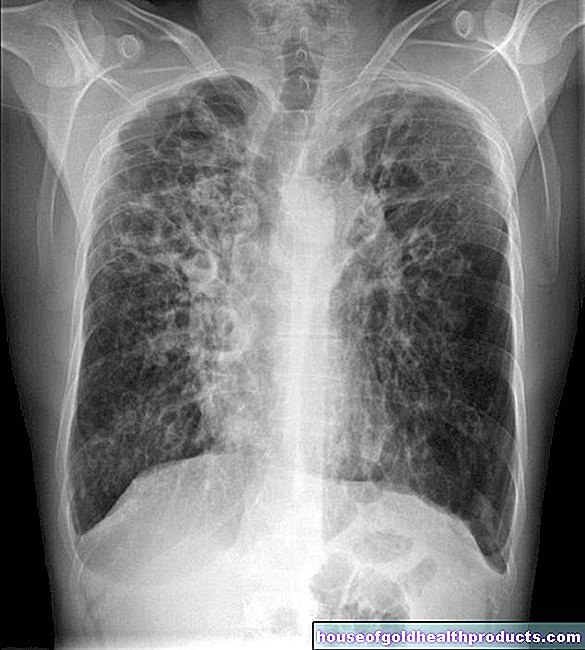
- Pulmonary emphysema: In pulmonary emphysema, the alveoli are partially overstretched and destroyed. The main symptom of the disease is dyspnea. Possible causes of emphysema are smoking, COPD, chronic bronchitis, and inhalation of pollutants. Age-related emphysema can also develop (old age emphysema).
- Inflammation of the lungs (pneumonia): In addition to symptoms such as fever and fatigue, it can also cause dyspnoea. Pneumonia is often the result of a respiratory infection and usually heals again without major complications. Pneumonia can be dangerous for children and old people.
- Atelectasis: Doctors refer to a collapsed ("collapsed") section of the lung as atelectasis. Depending on the extent, the result may be more or less severe dyspnea. Atelectasis can be congenital or as a result of a disease (such as pneumothorax, tumor) or an invading foreign body.
- Pulmonary embolism: In pulmonary embolism, a blood vessel in the lungs is usually blocked by a blood clot that has formed elsewhere in the body (such as in a leg vein in a leg vein thrombosis). Sudden shortness of breath with chest pain may indicate this. In severe cases, there is a risk of circulatory collapse and death.
- Pulmonary fibrosis: One speaks of pulmonary fibrosis when the connective tissue in the lungs increases abnormally and then hardens and scars. This progressive process increasingly affects the gas exchange in the lungs. This causes shortness of breath, at first only during physical exertion, later also at rest. Possible triggers for pulmonary fibrosis are, for example, inhalation of harmful substances, chronic infections, irradiation of the lungs and certain medications.
- Pleural effusion: The pleura (pleura) is a two-leaved skin in the chest. The inner leaf (lung fur) covers the lungs, the outer leaf (pleura) lines the chest. The narrow gap in between (pleural gap) is filled with some fluid. If this amount of fluid increases due to illness (for example with damp pleurisy), it is called pleural effusion. Depending on the extent, it can cause shortness of breath, tightness in the chest and breathing-dependent chest pain.
- Pneumothorax: In the case of a pneumothorax, air has penetrated into the gap-shaped space between the pleura and pleura (pleural gap). The resulting symptoms depend on the cause and extent of this amount of air. For example, dyspnoea, throat irritation, stabbing and breath-dependent pain in the chest and blue discoloration of the skin and mucous membranes (cyanosis) can occur.
- Cystic fibrosis (cystic fibrosis): This hereditary metabolic disease is associated with the formation of extremely viscous glandular secretions. The secretions of the lungs are also affected. Because they are so tough, they are difficult to remove (cough up). So they collect in the lungs, causing increased breathlessness and making them prone to bronchitis and pneumonia.
- Pulmonary hypertension: In pulmonary hypertension, the blood pressure in the lungs is permanently increased. Depending on the severity, this triggers symptoms such as shortness of breath, easy fatigue, fainting or water retention in the legs. Pulmonary hypertension can be an independent disease or the result of another disease (such as COPD, pulmonary fibrosis, HIV, schistosomiasis, liver disease, etc.).
- "Water in the lungs" (pulmonary edema): This is an accumulation of fluid in the lungs. For example, it can be caused by heart disease, toxins (such as smoke gas), infections, inhaling liquids (such as water), or certain medications. Typical symptoms of pulmonary edema are dyspnoea, cough and frothy sputum.
- Tumors: If benign or malignant tissue growths narrow or block the airways, dyspnea also sets in. This can happen with lung cancer, for example. Scar tissue after the surgical removal of a tumor can also narrow the airways and thus obstruct the flow of air.
Causes in the area of the heart
Various heart diseases can also be responsible for dyspnea. These include, for example:
- Heart failure: In the case of left heart failure (left heart failure), the weakened left half of the heart can no longer adequately pump the oxygen-rich blood from the lungs into the body's circulation. This is how the blood backs up in the pulmonary vessels (congested lung). This can lead to a build-up of water in the lungs (pulmonary edema) with shortness of breath and coughing. These symptoms also occur when both halves of the heart are weakened (global heart failure).
- Valvular heart disease: Valvular heart disease can also cause shortness of breath. For example, if the mitral valve - the heart valve between the left atrium and the left ventricle - leaks (mitral valve insufficiency) or is narrowed (mitral valve stenosis), those affected suffer from shortness of breath and coughing, among other things.
- Heart attack: Sudden severe dyspnea, a feeling of tightness or tightness in the chest, and fear or even fear of death are typical symptoms of a heart attack. Nausea and vomiting can also occur, especially in women.
- Inflammation of the heart muscle: If shortness of breath during exertion, weakness and increasing tiredness in connection with flu-like symptoms (runny nose, cough, fever, headache and body aches), the reason could be an inflammation of the heart muscle (myocarditis).
Other causes of dyspnoea
Breathlessness can have many other causes. Some examples:
- Anemia: Anemia is caused by a lack of hemoglobin. This is the red blood pigment in the red blood cells. These are responsible for the transport of oxygen (bound to hemoglobin).Therefore, anemia can cause shortness of breath, palpitations, ringing in the ears, dizziness and headaches, among other things. A possible cause of anemia is, for example, a lack of iron or vitamin B12.
- Injury to the chest (chest trauma): Shortness of breath can also occur, for example, with a bruised rib or a broken rib.
- Diaphragmatic Paralysis: The diaphragm is an important respiratory muscle. If the nerve supplying it (phrenic nerve) is paralyzed, the diaphragm can no longer effectively support breathing - dyspnoea occurs. Diaphragmatic paralysis can be triggered, for example, by a tumor along the nerve, amyotrophic lateral sclerosis or a chest injury.
- Scoliosis: In scoliosis, the spine is permanently curved to the side. In severe cases, this can impair lung function, leading to dyspnea.
- Sarcoid: This inflammatory disease is associated with the formation of nodular tissue changes. These can form anywhere in the body. Very often the lungs are affected. This can be recognized, among other things, by a dry cough and exertion-dependent dyspnea.
- Neuromuscular Disorders: Some neuromuscular disorders can also cause dyspnoea if the respiratory muscles are affected. Examples are poliomyelitis, amyotrophic lateral sclerosis (ALS) and myasthenia gravis.
- Hyperventilation: The term describes an unusually deep and / or rapid breathing, combined with a feeling of shortness of breath. In addition to certain illnesses, the cause can also be great stress and excitement. Women are more often affected than men.
- Depression and anxiety disorders: In both cases, those affected may have the feeling that they cannot breathe at times.
A psychologically induced shortness of breath (in the case of depression, stress-related hyperventilation, anxiety disorders, etc.) is also referred to as psychogenic dyspnea.
Dyspnea: when do you need to see a doctor?
Insidious or sudden, people with dyspnea should always see a doctor. Even if there are no further symptoms at first, serious illnesses can be the reason for the shortness of breath. If symptoms such as chest pain or blue lips and pale skin appear, it is best to call the emergency doctor immediately! Because these can be signs of a life-threatening cause such as a heart attack or pulmonary embolism.
Dyspnea: what does the doctor do?
First, the doctor will ask specific questions about the medical history (anamnesis), for example:
- When and where did the shortness of breath occur?
- Does the dyspnea occur at rest or only during physical activity?
- Does the shortage of breath depend on certain body positions or times of the day?
- Has the dyspnea got worse lately?
- How often does dyspnea occur?
- Are there any other symptoms besides shortness of breath?
- Are you aware of any underlying illnesses (allergies, heart failure, sarcoid, etc.)?
Various examinations follow after the anamnesis interview. They will help determine the cause and extent of the dyspnea. These examinations include:
- Eavesdropping on the lungs and heart: the doctor can use the stethoscope to listen to the chest and detect suspicious breathing noises, for example. The heart should also be monitored.
- Blood test: The patient's blood is routinely drawn in order to examine it in the laboratory for possible causes of the dyspnea. In the case of anemia, for example, the number of red blood cells is low. During a heart attack, certain enzymes are increased (such as troponin). A pulmonary embolism also leads to typical changes in certain blood values.
- Pulmonary function test: With the help of a pulmonary function test (such as spirometry), the doctor can assess the functional state of the lungs and airways more precisely. This can be used to assess the extent of COPD or asthma, for example, very well.
- Lungoscopy: The pharynx, larynx and upper bronchi can be viewed more precisely using a lung specimen (bronchoscopy).
- Imaging tests: They may also provide important information. For example, pneumonia, pulmonary embolism and tumors in the chest can be detected using X-ray examinations, computed tomography and magnetic resonance imaging. Ultrasound and nuclear medicine examinations can also be used.
The severity of the dyspnea can be assessed with the help of the Borg scale: This is done either by the doctor (based on the patient's description) or by the patient himself using a questionnaire. The Borg scale ranges from 0 (no breathlessness at all) to 10 (maximum breathlessness).
Dyspnea: Treatment by the doctor
Therapy for dyspnea depends on the cause. It can be correspondingly different. Some examples:
Bacterial infections like diphtheria are treated with antibiotics. Pseudocroup is treated with cortisone and expectorant drugs (secretolytics). Patients should also breathe fresh, moist air.
People with asthma are usually given anti-inflammatory glucocorticoids ("cortisone") and / or beta sympathomimetics (which widen the bronchi) for inhalation.
In pulmonary embolism, the first thing people often do is a sedative and oxygen. If necessary, the cycle must be stabilized. The trigger of the embolism - the blood clot in the pulmonary vessel - is tried to dissolve with medication. It may also have to be removed in one operation.
If iron deficiency anemia is causing the dyspnea, the patient is given an iron supplement. In severe cases, stored blood (red blood cells) must be given as a transfusion.
If a cancerous tumor in the chest area is the reason for the shortness of breath, the therapy depends on the stage of the disease. If possible, the tumor is surgically removed. Chemotherapy and / or radiation therapy may also be useful.
Dyspnea: You can do it yourself
If dyspnea occurs, it is best to see a doctor immediately. In the short term, the following tips can sometimes help against shortness of breath:
- In acute respiratory distress, the person affected should sit down with the upper body upright and support their arms (slightly bent) on their thighs. In this position (called the "coachman's seat"), certain muscles can mechanically support inhalation and exhalation.
- Those affected should keep calm as possible. Especially in the case of psychologically-related dyspnea, this can help the breathing to return to normal.
- Cool, fresh air is also beneficial. Not least because cold air contains more oxygen. This can reduce dyspnea.
- Asthmatics should always have their asthma spray close at hand.
- Patients with a long history of chronic lung disease often have oxygen bottles at home. You should discuss the dose of oxygen with your doctor.
- A healthy lifestyle can help prevent chronic shortness of breath from developing. Try to quit smoking or do not even start smoking. This significantly reduces the risk of dyspnea later.