Blood clotting
and Martina Feichter, medical editor and biologistValeria Dahm is a freelance writer in the medical department. She studied medicine at the Technical University of Munich. It is particularly important to her to give the curious reader an insight into the exciting subject area of medicine and at the same time to maintain the content.
More about the expertsMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Blood clotting is also known as secondary hemostasis and is a vital process in the body. Via the coagulation cascade, blood coagulation closes bleeding wounds with the help of blood clots (red thrombi).Find out more about the different coagulation factors and how blood clotting works here.
What is blood clotting?
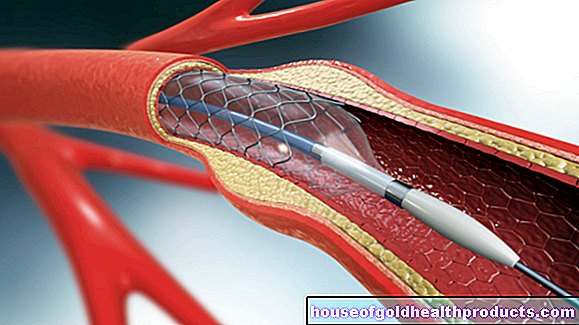
While primary hemostasis only temporarily closes bleeding, blood clotting (secondary hemostasis) tightly seals wounds with the help of a "red thrombus". It consists mainly of cross-linked fibrin and red blood cells stored in it.
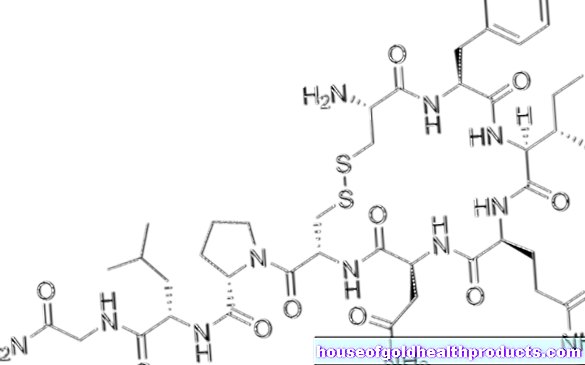
The complex mechanisms of coagulation are also referred to in their entirety as the coagulation cascade. Above all, various coagulation factors are involved. These have their own names, but are also numbered with Roman numerals. They will only be activated before use. This protects against the accidental and unwanted formation of thrombi, which could block the vessels.
Some of the names of the coagulation factors change when they are activated. In addition, a small “a” is added after the Roman numeral of a factor. Fibrinogen (factor I) becomes fibrin (factor Ia) and prothrombin (factor II) becomes thrombin (factor IIa).
Blood clotting: process
Blood coagulation can be divided into an extrinsic and an intrinsic path, which take place at different speeds, but both meet in a common end path.
Extrinsic route of blood clotting
We bleed from a wound when blood vessels are injured as well. With such vessel injuries, the inner wall of the vessels, the endothelium, is also damaged. In addition to many other substances, the so-called tissue factor (tissue thromboplastin, factor III) lies beneath the endothelium. In the event of an injury, it activates factor VII in the blood to form factor VIIa. This in turn activates factor X to factor Xa.
The extrinsic coagulation takes place within seconds.
Intrinsic route of blood clotting
In addition to factor III, there is also collagen under the endothelium, which plays an important role in primary hemostasis. In addition, it activates factor XII together with two other substances (kallikrein and kininogen). This in turn activates factor XI (to factor XIa), which in turn activates factor IX (to factor IXa). Together with factor VIIIa (as well as calcium ions and phospholipid), factor IXa forms factor X into factor Xa.
Intrinsic coagulation takes place in a matter of minutes.
Common final route
The extrinsic and intrinsic coagulation systems end with the activation of the coagulation factor X (to factor Xa) and then enter the common end segment: factor Xa and factor Va form the factor Xa-Va complex (prothrombinase). The prothrombinase activates factor II to factor IIa (thrombin). Thrombin splits off small parts of factor I (fibrinogen), the fibrin monomers (factor Ia). They are glued together with the help of factor XIIIa.
This stable fibrin network strengthens the blood platelets (thrombocytes) that are already attached to one another at the location of the vascular leak. Red blood cells get caught in the mesh, creating a red thrombus. In the further course, connective tissue cells migrate into the thrombus, with which wound healing begins.
Coagulation factors: table
There are 12 different coagulation factors, numbered from I to XIII. There is no factor VI.
|
Roman numeral |
Surname |
|
I. |
Fibrinogen |
|
II |
Prothrombin |
|
III |
Tissue Factor, Tissue Thromboplastin |
|
IV |
calcium |
|
V |
Pro-accelerator |
|
VII |
Proconvertin |
|
VIII |
Antihemophilia Factor A. |
|
IX |
Antihemophilia factor B or Christmas factor |
|
X |
Stuart Prower Factor |
|
XI |
Plasma thromboplastin antecendent (PTA)
|
|
XII |
Hageman factor |
|
XIII |
fibrin stabilizing factor |
The coagulation factors of the coagulation cascade also reinforce each other in ways that have not yet been clarified. Therefore, different proteins are necessary, which partially inhibit the coagulation, so that an equilibrium arises. These include antithrombin, protein C and protein S.
Antithrombin
You can find out more about this protein in the article Antithrombin.
When do you check blood clotting?
If someone bleeds for an unusually long time from injuries, laboratory tests must be performed to rule out a disruption of primary hemostasis or secondary hemostasis (blood clotting). Such a bleeding disorder can be congenital or acquired.
Blood clotting is also checked in people with liver disease because the liver is where the clotting factors are produced.
By determining blood coagulation, anticoagulant treatment with oral anticoagulants (such as phenprocoumon or warfarin) can also be controlled.
Blood coagulation is routinely checked before operations to rule out an increased risk of bleeding.
Quick value / INR
If the extrinsic pathway of blood coagulation is disturbed, the so-called Quick value is lowered. A possible cause is, for example, a lack of vitamin K, which the liver needs to produce the coagulation factors II, VII, IX and X.
In some people, the individual coagulation factors are reduced due to hereditary diseases. For example, factor VIII deficiency is referred to as hemophilia A and factor IX deficiency is referred to as hemophilia B. In both cases, blood clots very slowly - so bleeding is difficult to stop.
Liver diseases such as cirrhosis of the liver can also be the cause of a lowered Quick value.
The intake of anticoagulant drugs with coumarins also reduces the Quick value. However, the reduced production of the coagulation factors is desired here (for example after a pulmonary embolism or in the case of atrial fibrillation).
On the other hand, taking sedatives (barbiturates) or the antibiotic penicillin can increase the Quick value.
The quick value can vary depending on the test method. That is why the “International Normalized Ratio” (INR) was introduced, which makes Quick values comparable. The INR is too high with a reduced Quick value and too low with an increased Quick value.
Partial Thromboplastin Time (PTT)
To check the intrinsic pathway, the partial thromboplastin time (PTT) is measured. It is increased in disorders of this part of the blood clotting. This is the case, for example, with the hemophilia mentioned above. Other blood clotting disorders (such as von Willebrand syndrome) and treatment with the anticoagulant heparin also reduce PTT.
Conversely, the partial thromboplastin time can be reduced during pregnancy, through the use of the contraceptive pill and after surgery.
What to do if the blood coagulation values change?
Smaller deviations are usually not a cause for concern. However, if a change in blood clotting suggests a disease, further tests and examinations are carried out until the final diagnosis is made. In this case, your doctor will discuss how to proceed with you.
In the case of treatment with anticoagulants, deviating blood coagulation values (within a certain range) are the goal of the therapy.
Tags: baby toddler alcohol drugs drugs