Pancreatic insufficiency
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.In the case of pancreatic insufficiency, the pancreas no longer works efficiently. In the case of exocrine pancreatic insufficiency, the organ produces too few digestive enzymes. The result is digestive problems with diarrhea. In the case of endocrine pancreatic insufficiency, the production of blood sugar-regulating hormones is impaired. Then it comes to blood sugar disorders. Therapy depends on whether there is exocrine and / or endocrine pancreatic insufficiency. Here you can read everything you need to know about the dysfunction of the pancreas!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. K86

Pancreatic Insufficiency: Description
The pancreas is in the upper abdomen, just behind the stomach. It has two basic tasks: On the one hand, it produces digestive enzymes (exocrine function). On the other hand, it also produces hormones such as insulin and glucagon (endocrine function). These hormones are involved in blood sugar regulation.
With pancreatic insufficiency, one or both functions can be too weak or fail completely. This means: Endocrine and exocrine pancreatic insufficiency can occur independently of one another or at the same time.
Exocrine pancreatic insufficiency
The pancreas produces around one to two liters of digestive secretion every day. This reaches the duodenum via the pancreatic duct and supports the digestion of the food ingested: The pancreatic secretion neutralizes the acidic gastric acid that has entered the intestine with the food pulp. The secretion also contains enzymes for the digestion of proteins, fats and carbohydrates.
If too few or no digestive enzymes are produced in the pancreas, it is called exocrine pancreatic insufficiency. Symptoms of this form of disease usually only appear when 90 percent of the organ function has already failed.
Endocrine pancreatic insufficiency
If the pancreas produces too little or no more hormones, it is called endocrine pancreatic insufficiency. Insulin and glucagon are among the best-known pancreatic hormones: Both together regulate the blood sugar level:
- Insulin is responsible for the fact that the sugar in the blood (glucose) can be absorbed into the body cells - the blood sugar level drops.
- If, on the other hand, the body needs more energy (e.g. during stress or low blood sugar levels), glucagon mobilizes energy reserves in the body - it promotes the release of stored glucose (storage form: glycogen) and the formation of new glucose. This causes the blood sugar level to rise.
Most people with endocrine pancreatic insufficiency have diabetes (diabetes mellitus). With them, the pancreas produces too little or no insulin at all.
Note: If the sugar level in the blood is too high, it is called hyperglycaemia. If it is too low, it is called hypoglycemia.
Pancreatic insufficiency: symptoms
Depending on which region of the pancreas is no longer working properly, different symptoms appear.
Exocrine pancreatic insufficiency: symptoms
Here complaints only arise when around 90 percent of the organ function has already failed.
First and foremost, fat digestion causes problems for those affected - the dietary fat can no longer be broken down as well, which can cause nausea and vomiting. If the exocrine pancreatic insufficiency is very advanced, the fats contained in the food no longer get enough into the intestinal cells and are excreted with the stool. Oily diarrhea (fatty stools) with abdominal pain are typical. The excrement then appears greasy, shiny and usually smells bad. The stool can also be lightly discolored and liquefied, as with diarrhea.
Due to impaired digestion, people with exocrine pancreatic insufficiency can lose a lot of weight even though they eat enough.
Another consequence of the disturbed fat digestion: The fat-soluble vitamins E, D, K and A can no longer be properly absorbed into the body. This is how vitamin deficiencies can develop. These in turn cause their own complaints. For example, a severe vitamin K deficiency leads to an increased tendency to bleed.
Due to the insufficient production of digestive secretions, a lot of undigested food also gets into the colon. There, intestinal bacteria decompose the food components with strong gas formation. The result is sometimes very painful gas.
Exocrine pancreatic insufficiency often results from repeated inflammation of the pancreas. That is why those affected often notice the symptoms of such pancreatitis: Belt-shaped pains in the upper abdomen that radiate to the back are typical.
Endocrine pancreatic insufficiency: symptoms
In the case of endocrine pancreatic insufficiency, the normal sugar metabolism in particular is disturbed because the pancreas does not produce enough blood-sugar-regulating hormones.
If the pancreas does not produce enough insulin, the sugar circulating in the blood can no longer be absorbed by the cells. This can result in extremely high blood sugar levels (hyperglycaemia). The result is ailments that are also known from diabetes: thirst, frequent urination, fatigue, etc. The insulin deficiency also means that brain cells do not receive enough sugar and therefore not enough energy. As a result, the body produces so-called ketone bodies for energy production, which can also be transported into the cells without insulin. However, the ketone bodies are acidic, which means that they lower the pH value in the blood. So a "ketoacidosis" develops with its own symptoms (vomiting, thirst, acetone halitosis, etc.).
If glucagon is predominantly lacking in endocrine pancreatic insufficiency, the body can no longer raise a blood sugar level that is too low. This occurs, for example, when you haven't eaten for several hours. Normally, the body's energy reserves are then mobilized through the glucagon in order to raise the blood sugar level. If this is not possible, severe hypoglycaemia can occur. Typical symptoms are tremors, cold sweats and loss of consciousness. In this situation, glucose must be administered urgently so that there is no undersupply of the brain!
Pancreatic Insufficiency: Causes and Risk Factors
In most cases, pancreatic insufficiency occurs as part of an acute or chronic inflammation of the pancreas (pancreatitis).Occasionally, it is caused by a metabolic disease called cystic fibrosis, a malignant tumor, or surgery that involves removing part or all of the pancreas.
In rare cases, no trigger can be found for the disease. Then experts speak of idiopathic pancreatic insufficiency.
Pancreatic insufficiency when the pancreas is inflamed
The pancreas can become inflamed for various reasons (pancreatitis). A distinction is made between acute and chronic inflammation. Acute inflammation is caused in over half of all cases by biliary tract diseases such as narrowing or gallstones. Excessive alcohol consumption is often to blame for the disease. In rare cases, drugs (e.g. estrogens, cyclosporine, HIV drugs), abdominal injuries, infections or genetic diseases trigger acute pancreatitis.
In 80 percent of the cases, chronic and excessive consumption of alcohol is responsible for chronic inflammation of the pancreas. More rarely, it is caused by drugs, genetic changes or metabolic diseases in which the lipid metabolism is affected or the parathyroid glands are impaired. With repeated inflammations of the pancreas (recurrent pancreatitis), more and more cells of the pancreas are gradually damaged. The result is chronic pancreatic insufficiency.
Pancreatic insufficiency in cystic fibrosis
Cystic fibrosis (cystic fibrosis) is a hereditary disease that affects not only the pancreas but also the airways, intestines, liver and biliary tract. Incorrect information in the genome means that a channel in cell membranes (chloride channel) is not properly formed. This influences important transport and metabolic processes in the cells. Above all, glands in the body in which this channel fulfills an important function can be impaired - for example those glands in the pancreas that produce digestive secretions. The secretion of those affected is much more viscous than that of a healthy person. It thereby clogs the pancreatic duct. As a result, the digestive enzymes are still activated in the pancreas, causing the organ to become inflamed. The first thing that develops is exocrine pancreatic insufficiency. In the course of the disease, endocrine pancreatic insufficiency can also occur.
Pancreatic insufficiency in tumors or after surgery
In the case of malignant tumors that are close to the pancreas, part of the pancreas must sometimes be surgically removed due to the anatomical proximity. This is the case, for example, with certain stomach tumors. Tumors of the pancreas (pancreatic carcinoma) are also partially surgically removed. They can clog the pancreatic duct, which is the route through which digestive fluids enter the duodenum. The juice then builds up and causes inflammation of the pancreas. As a result, pancreatic tissue is destroyed. Surgical removal of tumors also reduces the tissue of the pancreas. Overall, the secretion production can then no longer be sufficient. If the proportion of functioning tissue shrinks below ten percent, symptoms of exocrine pancreatic insufficiency usually occur.
Pancreatic insufficiency: examinations and diagnosis
The right person to contact if you suspect pancreatic insufficiency is your family doctor or a specialist in internal medicine. The doctor receives important information just by describing your symptoms (anamnesis). Possible questions from the doctor could include:
- Do you have greasy and shiny stools?
- Do you have diarrhea? If so, how many times a day?
- Have you ever had an inflammation of the pancreas?
- Do you tolerate fatty foods poorly?
- Do you take any medicine?
Physical examination
Based on the medical history, the doctor may physically examine you. In particular, he will listen to the abdomen with the stethoscope and carefully feel it with his fingers. Please tell the doctor if you have abdominal pain or feel painful to feel.
The investigation of a possible malfunction of the pancreas also includes an inspection of the skin and eyes. In the case of pnacreas diseases, the skin and eyes can turn yellow (jaundice = jaundice). However, jaundice is not specific to a malfunction of the pancreas! It can also occur, for example, in diseases of the liver (hepatitis) or the biliary tract.
Laboratory examination for pancreatic insufficiency
The determination of the enzymes elastase-1, lipase and amylase in the blood can provide evidence of inflammation of the pancreas as the cause of pancreatic insufficiency. The activity of the pancreatic enzymes (elastase and chymotrypsin) in the stool is analyzed specifically to prove that the pancreas is involved. This stool examination is the most important part of the diagnosis if exocrine pancreatic insufficiency is suspected.
In addition, an elaborate test is very rarely used, in which the secretion production of the pancreas can be measured directly (secretin-pancreozymin test). Since the pancreas does not work continuously, a substance is injected prior to this examination that artificially stimulates secretion production. A probe that is pushed through the mouth to the duodenum can then be used to directly measure how well the pancreas is still secreting.
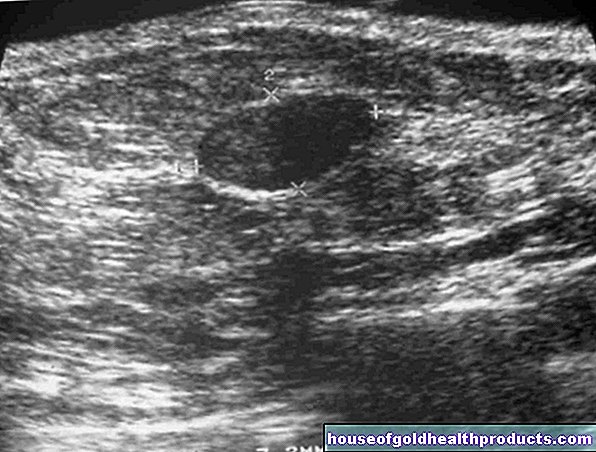
Imaging for pancreatic insufficiency
In exocrine pancreatic insufficiency, imaging is primarily used to discover the obvious causes of the disease (tumor, inflammation). The doctor can detect calcification of the pancreas particularly well with computed tomography (CT). If such calcifications are visible, chronic pancreatitis probably led to pancreatic insufficiency. The pancreas can also be examined in detail with magnetic resonance imaging (MRI).
As part of an endoscopic examination, pancreatic stones and changes in the ducts can be assessed well. To do this, as in a gastroscopy, a thin tube is pushed through the mouth to the mouth of the pancreatic duct in the duodenum. With a small probe, the doctor injects a contrast agent into the pancreatic ducts, making them clearly visible for the X-ray image.
Another method for assessing the pancreas is an ultrasound examination (sonography). However, since the pancreas lies quite deep in the abdomen and is mostly covered by intestinal gases, it is relatively difficult to see it with sonography. That is why ultrasound is more likely to be used in slim patients.
Pancreatic Insufficiency: Treatment
If exocrine pancreatic insufficiency is triggered by a specific cause, this should first be eliminated. Stones or constrictions in the duct of the pancreas can be treated endoscopically. The examination is similar to a gastroscopy. Stones are removed with a pair of pliers and a small collecting basket or crushed and washed out. Narrow spots are widened with a small balloon and then held open with a piece of tube ("stent").
If the exocrine pancreatic insufficiency persists despite such an intervention, an attempt is made to alleviate the symptoms and replace the function of the pancreas. The following therapeutic measures can help:
1) Exocrine Pancreatic Insufficiency: Diet
People with exocrine pancreatic insufficiency should split their diet into five to seven small meals a day and avoid fatty foods as much as possible. In addition, those affected should completely refrain from alcohol. These dietary measures serve to relieve the digestion and thus reduce the symptoms. If fat stools persist despite this diet, the fat content of the diet must be reduced further.
2) Exocrine pancreatic insufficiency: enzyme replacement
If a change in diet alone does not improve the symptoms, the enzymes in the pancreatic secretions can be replaced. To do this, special capsules are taken several times a day. These have an enteric coating so that the digestive enzymes they contain are only activated in the small intestine. The digestive enzymes contained in the drug mostly come from the pancreas of slaughtered pigs. But there are also preparations with fungal enzymes.
Some digestive enzymes can also be produced by other organs in the body, such as the salivary gland. So they don't necessarily need to be replaced. Only the fat-splitting enzyme (lipase) has to be added to the larger meals. The amount depends individually on the size and composition of the food.
3) Exocrine pancreatic insufficiency: vitamin replacement
Vitamins E, D, K, A are fat-soluble. This means that they can only be absorbed in the intestine if they are dissolved ("emulsified") in fat. This is only possible if the fats are also broken down by certain enzymes (lipases). Split fats, together with the fat-soluble vitamins, form a complex (“micelle”) that is not repelled by the polar intestinal wall.
Exocrine pancreatic insufficiency may interfere with adequate vitamin absorption, as insufficient fat-splitting proteins are formed and the fat-soluble vitamins can therefore not be absorbed from the intestine into the blood. For example, a vitamin K deficiency can cause severe bleeding. A vitamin D deficiency can promote the development of osteoporosis. In severe pancreatic insufficiency (with many fatty stools), the fat-soluble vitamins are therefore artificially injected into the muscle.
Endocrine pancreatic insufficiency: insulin therapy
In the case of endocrine pancreatic insufficiency, the blood sugar level must be checked regularly and, if necessary, artificially supported. If there is an absolute lack of insulin, this is also referred to as type 1 diabetes mellitus. Those affected have to inject insulin regularly.
If the antagonist of insulin, glucagon, is also affected by endocrine pancreatic insufficiency, this increases the risk of life-threatening hypoglycaemia due to insulin administration. This must be taken into account when treating pancreatic insufficiency.
Pancreatic insufficiency: disease course and prognosis
An already existing pancreatic insufficiency cannot be cured. But you can influence it positively with the right therapy and usually reduce the symptoms to a tolerable level. The prognosis essentially depends on whether only one function (exocrine or endocrine) of the pancreas is impaired and the underlying cause of the disease. In any case, triggering factors such as alcohol should be avoided as they can worsen pancreatic insufficiency.
Tags: skin care pregnancy birth palliative medicine