Idiopathic thrombocytopenic purpura
Astrid Leitner studied veterinary medicine in Vienna. After ten years in veterinary practice and the birth of her daughter, she switched - more by chance - to medical journalism. It quickly became clear that her interest in medical topics and her love of writing were the perfect combination for her. Astrid Leitner lives with daughter, dog and cat in Vienna and Upper Austria.
More about the experts All content is checked by medical journalists.Immune thrombocytopenia (ITP) is a rare blood disorder in which there is a lack of blood platelets (thrombocytes) due to a malfunction of the immune system. Affected people have, among other things, an increased risk of bleeding. Read here how the disease is progressing and how it is treated!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. D69

Brief overview
- What is the ITP? Acquired blood disorder in which there is a lack of platelets due to a malfunction of the immune system
- Course and prognosis: Individual course, prediction not possible, spontaneous healing possible (especially in children). ITP patients being treated have a normal life expectancy.
- Treatment: waiting and regular medical check-ups (watch and wait), corticosteroids, immunotherapy, thrombopoietin receptor agonists, spleen tyrosine kinase inhibitors, removal of the spleen
- Symptoms: Increased bleeding tendency (bruises, bleeding in the case of minor injuries), bleeding of the skin and mucous membranes the size of a pinhead is typical, tiredness, some of the patients show no symptoms
- Causes: Autoimmune disease (immune system makes antibodies against blood platelets), trigger mostly unknown
- Risk factors: In 20 percent of cases, ITP is the result of another disease such as arthritis, lymphoma, cancer, HIV or herpes infection.
- Diagnostics: Typical symptoms, blood test, blood smear, coagulation test, ultrasound, bone marrow aspiration
- Prevention: No specific preventive measures possible
What is idiopathic thrombocytopenic purpura?
Immune thrombocytopenia (ITP, autoimmune thrombocytopenia, immune thrombocytopenia) is a rare blood disease in which there are not enough blood platelets (thrombocytes) due to a malfunction of the immune system. People are prone to bruising and bleeding.
Normally, the platelets ensure that an injured vessel is sealed quickly and the bleeding stops.If there are too few platelets due to ITP, blood clotting does not work as it should. Affected people tend to bruise even from slight bumps, and minor injuries such as cuts bleed longer than normal.
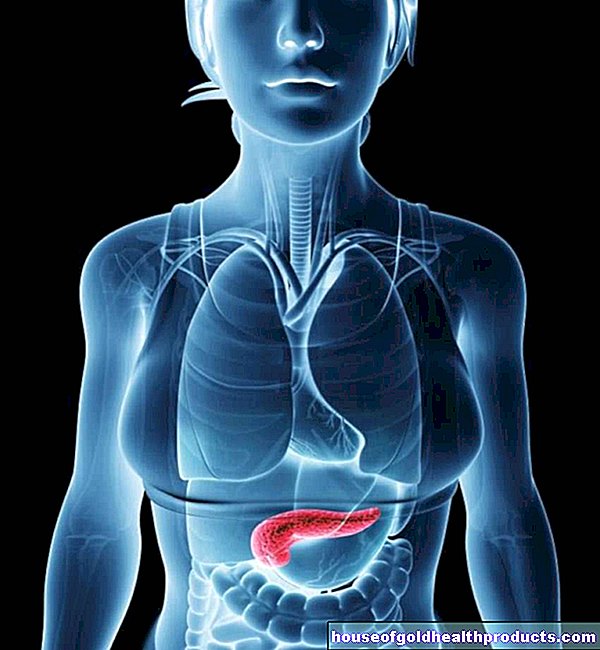
The cause of the disease is a malfunction of the immune system: it incorrectly produces defensive bodies (antibodies) against the blood platelets and their precursor cells in the bone marrow. These antibodies cause the platelets to be broken down in the spleen in a short time and their formation in the bone marrow is inhibited. The result is that there are too few platelets overall.
Healthy people typically have at least 150,000 to 350,000 platelets / µL of blood. In patients with ITP, the number of platelets drops repeatedly or permanently below 100,000 / µl blood.
ITP is not congenital and is not inherited. The disease develops spontaneously over the course of life. How this happens is largely unknown. In around 80 percent of the cases, no cause can be determined; doctors speak of “primary or idiopathic thrombocytopenia”. In 20 percent of all those affected, ITP occurs as part of another illness, doctors then refer to it as "secondary".
Other names
Doctors also refer to ITP as Werlhof's disease or Werlhof's disease. The name goes back to the German doctor Paul Gottlieb Werlhof, who first described the disease in 1735.
Older terms such as idiopathic thrombocytopenic purpura, hemorrhagic purpura, idiopathic thrombocytopenia or idiopathic immune thrombocytopenic purpura are no longer used in specialist circles because the term “idiopathic” (without a tangible cause) is no longer applicable due to new findings. The same applies to the term “purpura” (inflammation of the smallest vessels under the skin), which does not occur in every case of immune thrombocytopenia.
frequency
Immune thrombocytopenia is rare: in Germany, two to seven out of 100,000 children and two to four out of 100,000 adults develop it every year. The mean age of onset in adults is around 60 years. Men are three times more likely to be affected than women. In younger adulthood, more women develop ITP. In children, more boys are affected than girls.
Is ITP curable? Is it fatal?
How the ITP will progress in the respective patient cannot be foreseen. Children up to ten years of age have the best chance of recovery: with them - but also with some adults - the disease heals on its own in many cases. Doctors speak of "spontaneous remission".
The younger the patient, the better the chances of recovery. And: the more acute the disease begins (for example in children after an infection), the better the chance that it will disappear again. If ITP is insidious, the likelihood of spontaneous healing is less. With successful treatment, ITP patients have a normal life expectancy.
Stages of the disease
Depending on the time that has passed since diagnosis, doctors distinguish three stages:
- Newly diagnosed (time of diagnosis up to three months later): ITP may resolve without treatment.
- Persistent ITP (three to twelve months after diagnosis): Spontaneous regression is still possible.
- Chronic ITP (ITP lasts more than twelve months): Spontaneous resolution is unlikely. The disease lasts for years, sometimes even for life. Around 60 percent of all affected adults and 20 to 30 percent of all children develop a chronic course.
Risk of fatal outcome
The risk of developing life-threatening bleeding in children is virtually zero. In adults, the risk is between zero and seven percent.
treatment
The aim of treatment is to cure the ITP and stop any bleeding. How the doctor treats the disease depends on the individual course and stage of the disease.
Immune thrombocytopenia does not need to be treated in every case. In the case of newly diagnosed ITP in children and adolescents, it is possible to wait and see and avoid drug therapy. Children under ten are particularly likely to heal on their own. Even in adult ITP patients without symptoms, the doctor usually waits and checks the blood values regularly.
First-line therapy
If the first symptoms such as bleeding appear, the so-called "first-line therapy" is used.
Cortisone: The patient first receives high doses of corticosteroids. They inhibit the formation of platelet antibodies. After a few days there is an increase in blood platelets, but this does not last long. The dose is reduced after two to three weeks and slowly stopped after three to six weeks.
Immunotherapy: If heavy bleeding occurs or the blood platelet count needs to be increased quickly (for example, during an upcoming operation), the patient receives special antibodies in addition to cortisone, which are administered via a vein. They prevent the premature breakdown of blood cells. Doctors speak of "immunotherapy".
Second line therapy
If the first-line therapy is unsuccessful or unsuccessful, the doctor switches the treatment to the second-line therapy. Different active ingredients are used individually or combined with one another, depending on the bleeding tendency and the response to the treatment.
Thrombopoietin receptor agonists: Thrombopoietin receptor agonists (TPO-RA) stimulate the formation of blood platelets in the bone marrow. Therapy in the form of tablets or syringes is usually continued for life.
Spleen Tyrosine Kinase Inhibitors: The spleen tyrosine kinase enzyme plays a role in breaking down platelets in the spleen. So-called spleen tyrosine kinase inhibitors block the enzyme and thus prevent the early breakdown of platelets. The active ingredient fostamatinib is used.
Removal of the spleen
Since ITP heals spontaneously in some cases even years after the onset of the disease, the splenectomy (splenectomy) should not be performed too early. Doctors usually only recommend removing the spleen when all medication has been exhausted or life-threatening bleeding is expected. Since the spleen is involved in the immune system, patients are usually more susceptible to infections after the operation.
Tips for everyday life with ITP
Diet: There is no special diet that has a positive effect on the course of immune thrombocytopenia. In any case, make sure you have a healthy and balanced diet!
Exercise: Try to be physically active as regularly as possible. This not only strengthens physical well-being, but also has a positive effect on the often occurring states of fatigue!
Avoid sports with an increased risk of injury such as soccer, martial arts and contact sports, mountain biking, horse riding, skiing or ice hockey. For example, swimming, hiking, jogging, tennis, golf or dancing are more suitable. Minimize your risk of injury by wearing a helmet, joint protectors and other protectors whenever possible!
Medication: Discuss any use of medication (including those not requiring a prescription) with your doctor! For example, some painkillers inhibit blood clotting and increase your risk of bleeding!
Dental interventions: tell your dentist about your condition. Root canal treatment or tooth extraction may have to be postponed until a certain platelet count is reached. Simple dental procedures are usually less critical.
Symptoms
Ten percent of all children and 20 to 30 percent of all adults have no bleeding symptoms at the time of diagnosis of immune thrombocytopenia. In the case of chronic ITP, as many as 30 to 40 percent show no symptoms.
It is not possible to predict which and in which form the symptoms will occur. The course varies individually.
If symptoms occur, the most common symptoms are:
- Punctiform, pinhead-sized bleeding (petechiae) on the legs, oral mucosa and nose, less often on the arms and trunk
- Bleeding gums, nosebleeds
- Minor injuries such as small cuts bleed for an unusually long time.
- Longer and heavier menstrual bleeding
- Tendency to bruises (hematomas) even with only minor bumps
- Blood in the urine
- Severe tiredness and exhaustion (fatigue), decreased performance
- Loss of appetite
- Too little iron in the blood (iron deficiency anemia)
- Pallor, shortness of breath
- Hair loss
- Very rare (in two to three percent of patients): life-threatening bleeding in internal organs such as the spleen, liver, kidneys or lungs. Cerebral hemorrhage occurs in less than one percent of all patients.
Cause and risk factors
The cause of immune thrombocytopenia is an autoimmune reaction: the immune system mistakenly recognizes structures on the blood platelets (thrombocytes) and their precursor cells (megakaryocytes) in the bone marrow as foreign and forms defensive bodies (antibodies) against them. These antibodies accelerate the breakdown of blood platelets and also impair their formation. This reduces the overall proportion of red blood cells in the organism. The risk of bleeding increases.
ITP is a disease that is not inherited, but rather develops spontaneously in the course of life.
Triggers immune thrombocytopenia
In most cases (primary immune thrombocytopenia) the trigger is unknown; in a small proportion of patients, ITP develops as part of another disease (secondary immune thrombocytopenia). In children, the disease is usually triggered by a banal infection.
Primary ITP: In 80 percent of the cases, there is no specific trigger for the autoimmune reaction.
Secondary ITP: 20 percent of the time, the trigger is another disease. These include, for example, other autoimmune diseases such as arthritis, lymphomas and other cancers, infections with HIV or hepatitis viruses. Secondary ITP very rarely occurs after taking certain medications.
Investigation and diagnosis
In symptom-free patients, the doctor usually discovers the signs of ITP by chance during routine blood tests - for example during a preventive medical check-up.
In other cases, frequent nosebleeds and bruising or abnormally long bleeding (after injuries or menstrual bleeding) prompt a doctor's visit. The first point of contact is usually the family doctor or the pediatrician.
Important: There is no specific test that proves an ITP. The doctor therefore conducts a series of examinations. Only when other diseases, which also cause platelet deficiency, have been ruled out, is it possible to diagnose the disease. Doctors speak of a "diagnosis of exclusion".
anamnese
In the initial consultation, the doctor asks about the current symptoms and how long they have existed. It is important for him to know whether you are taking medication (especially anticoagulants), are pregnant, drink alcohol, have viral infections or have other illnesses. He will also ask whether bleeding or blood clots (thrombosis) have occurred.
Physical examination
The doctor will then examine the patient for physical signs of platelet deficiency. He pays particular attention to signs of bleeding and whether lymph nodes are enlarged, and scans the spleen and liver via the abdomen.
Blood test
The most important step in diagnosing thrombocytopenia is to do a blood test. The most noticeable change is a low platelet count. The doctor then examines the individual blood cells for changes (blood smear). To do this, he spreads a drop of blood on a glass slide and looks at the blood cells under the microscope. To check how well the blood is clotting, he arranges for clotting tests.
If the platelet count is several times below 100,000 / µl blood and all other blood values are normal, the diagnosis is ITP.
Bone marrow aspiration
In unclear cases - for example, when another disease such as leukemia cannot be ruled out - the doctor will perform a bone marrow puncture and examine the blood-forming cells in the bone marrow.
To do this, the doctor takes a few milliliters of bone marrow from the patient's pelvic bone under local anesthesia. The bone marrow cells obtained are then examined under a microscope in the laboratory.
The procedure is usually carried out on an outpatient basis and takes around 15 minutes. Most patients only feel a slight feeling of pressure at the puncture site and a brief, sharp pain as soon as the doctor draws the bone marrow into the syringe.
Ultrasound examination
Some ITP patients have an enlarged spleen and liver. An enlargement of these organs can be determined by means of an ultrasound examination.
Prevent
In most cases (80 percent), ITP develops spontaneously with no apparent cause. In these cases, prevention is not possible.
In every fifth ITP patient, other diseases such as arthritis, lymphoma, other cancers, HIV or herpes infections are the cause of ITP. In these cases, it is only possible to prevent it to a limited extent, for example through general protection against infections.
Tags: medicinal herbal home remedies pregnancy laboratory values









.jpg)