Gut flora - motor for MS
Christiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
More posts by Christiane Fux All content is checked by medical journalists.The predisposition to multiple sclerosis (MS) is genetically programmed. The nervous disease only rarely breaks out - how and how, that remained a mystery. Now there are increasing indications that the initial spark for this could take place in the intestine.
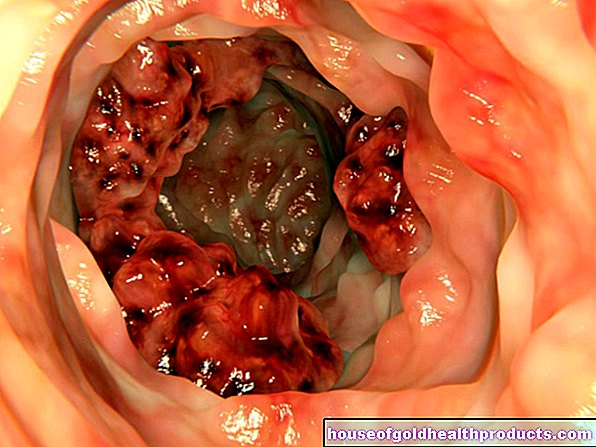
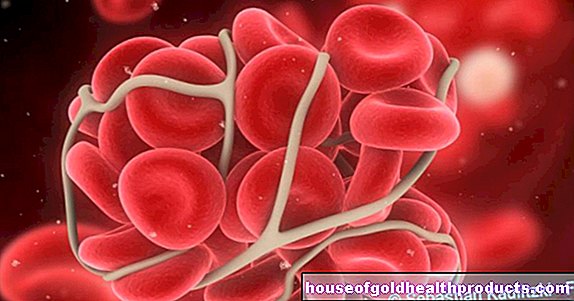
There is turmoil in the human intestine. Around 100 trillion bacteria live here - 100 times as many cells as the body has. The small lodgers are important, they help with digestion. And they have a massive influence on the immune system: like sparring partners, they train the immune cells and make them fit for the fight against pathogens.
Immune cells on the wrong track
If something goes wrong, however, the consequences could be devastating: improperly controlled immune cells may then attack the body's own cells, scientists now suspect. Probably the same in the case of multiple sclerosis. In this disease of the nervous system, the immune cells destroy the insulating myelin layer that envelops the nerve fibers and enables electrical information to be transmitted in the first place. The consequences: paralysis and dysfunction of muscles and organs.
"It seems that intestinal bacteria are an important trigger factor for MS," says Prof. Hartmut Wekerle from the Max Plank Institute in Munich in an interview with They may trigger an initial spark that sets the disease process in motion. Wekerle himself investigated this connection in mice that are genetically programmed to develop an MS-like disease. Animals that were kept aseptic and whose intestines were consequently not colonized by bacteria remained healthy. Their genetically identical conspecifics who had an intestinal flora, however, fell ill.
Twins bring light into the dark
A study that is currently being carried out at the Großhadern Clinic in Munich under the direction of Prof. Reinhard Hohlfeld shows the connection even more impressively. The team analyzes the intestinal flora - also known as the microbiome - of identical twins, only one of whom has MS at a time. “In this way, genetic differences are largely eliminated, and we can really concentrate on the disease,” explains his colleague Wekerle. Identical twins may have the same genetic make-up, but only in 30 percent of cases do both twins suffer from MS.
Initial studies did not reveal any dramatic differences between stool samples from MS subjects and their healthy twins. But when the researchers transferred the bacteria to MS-susceptible mice, the consequences were very different: animals in whose intestines the microbiome of MS sufferers had settled developed the disease much more frequently.
Badly programmed immune system
It is likely that bacteria in the intestinal flora of people with a genetic predisposition to MS program the immune cells incorrectly. With a different intestinal flora, the same person may not get MS. “But that's all still a pure hypothesis,” says the neurobiologist Wekerle.
Nevertheless, the possible connection between the microbiome and MS arouses a seductive thought: Should the intestinal flora really be a trigger for MS - can the disease then perhaps be treated by manipulating the intestinal flora? "There is a lot to be said for it, but whether this will actually work is still completely open," warns the researcher, who does not want to arouse false hopes in sick people. It is possible that the intestinal flora trigger a disease process that cannot be stopped easily.
Eliminated culprits
Should it work, however, antibiotics would be an option that would turn off the MS-promoting intestinal dwellers. However, this is a double-edged sword, because the active ingredients could cause collateral damage. Another possibility would be to attach special viruses to the pathogenic bacteria that only kill them. “Phage therapy” is what doctors call such an approach.
For both lines of therapy, it would be necessary to find out beforehand which bacteria are actually responsible for the outbreak of MS. "And that is a huge effort," says Wekerle. Millions of different genes were already in a single stool sample, an analysis that can only be mastered with the latest technology. And in the case of multiple sclerosis, a large number of samples would have to be compared in order to obtain reliable results. Because: MS occurs in many different variants. These differences could also be reflected in the patient's microbiome.
Healthy chair donation
One method that would be able to do without precise knowledge of the causing microbial profiles is the so-called fecal transplantation. To do this, a patient's intestinal flora is first completely eliminated with the help of antibiotics. The intestines are then repopulated with bacteria from the stool of healthy people. In the case of severe inflammatory bowel diseases, the procedure is already being practiced in isolated cases. Whether it can also help people with MS needs to be investigated in clinical experiments.
And there is also a more appetizing option for influencing the intestinal flora: diet. Because which bacteria settle in the intestines is also influenced by the food that a person consumes.
The intestine eats with you
Using this to treat MS is not new - people with MS have long tried to improve their condition through a special diet. "There are definitely 100 different diets that are reported to help," says Wekerle. Given the latest study results, it is not unlikely that some of them could actually work.
The example of Japan speaks for the fact that diet and MS could really be related. "Thirty years ago, multiple sclerosis was an exotic disease there that only occurred very sporadically," reports Wekerle. But that has changed in the meantime: The number of cases in the land of Nippon has risen rapidly in parallel with the increasing westernization of the country.
In fact, the Japanese now often take a bad example from the eating habits of the western world: "McDonaldification" is what Wekerle calls the phenomenon. Fast food instead of sushi. However, this is not yet proof of the presumed connection. Other environmental factors that have changed at the same time may be behind the increase in the disease.
The fact is: the need for research is still immense, the function of the microbiome and its interaction with the immune system and the functions of the body are only just beginning to be understood. But there is movement in research: asthma and allergies, obesity, autism and depression - all diseases that have recently been suspected of being related to the microbiome. Wekerle says: "The molecular study of the intestinal flora has become a train that everyone is now jumping on."
Tags: sleep organ systems Menstruation