Blood transfusion
Valeria Dahm is a freelance writer in the medical department. She studied medicine at the Technical University of Munich. It is particularly important to her to give the curious reader an insight into the exciting subject area of medicine and at the same time to maintain the content.
More about the experts All content is checked by medical journalists.In blood transfusion (blood transfer), whole blood or parts of the blood are injected into the vein. In this way, a lack of blood, such as that caused by high blood loss, can be compensated for. Read everything about blood transfusion, how it works and the risks it can pose.
![]()
What is a blood transfusion?
A blood transfusion is used to compensate for a lack of blood or blood components or to exchange the blood in the body. The blood reserves - plastic bags filled with blood - are given through a venous access. If the blood comes from a foreign donor, the blood reserve is referred to as a foreign blood donation. If you receive your own blood that was previously drawn and stored, it is called autologous blood donation or autotransfusion. Whilst in the past whole blood transfusions were carried out with all of its components, nowadays blood is separated into its individual components. This gives you:
- Red blood cell concentrate (erythrocytes)
- Granulocyte concentrate from white blood cells (granulocytes)
- Platelet concentrate from blood platelets (thrombocytes)
- Blood plasma
When to do a blood transfusion
Blood transfusions are always carried out when a deficiency in the body caused by blood loss needs to be corrected. Red blood cell concentrates are mostly used in acute blood loss to replace the lost red blood cells.
Platelet concentrates are also given in the event of high blood loss. In addition, this type of blood transfusion is administered to prevent blood platelet formation and to prevent bleeding before operations.
Since the blood plasma contains coagulation factors that are important for blood clotting, it is also transfused as a preventive measure if a tendency to bleeding is suspected.
Granulocyte concentrate can be given as part of a blood transfusion for cancer. The white blood cells it contains are said to strengthen the weakened immune system.
What do you do with a blood transfusion?
Before the actual blood transfusion, the doctor will discuss possible risks and side effects with you and determine your blood type. You must also sign a declaration of consent.
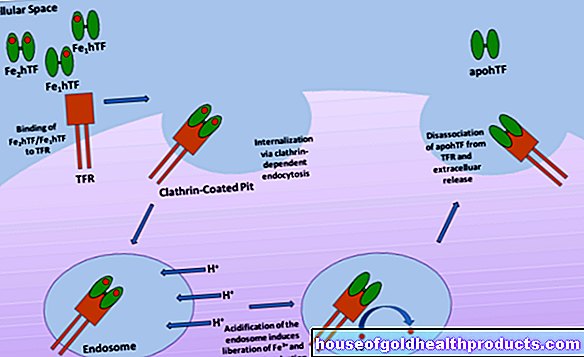
With the help of the so-called bedside test and the cross match, it is ensured that the blood transfusion does not cause any dangerous defensive reactions in the immune system. This incompatibility is caused by various proteins on the blood components and in the blood plasma, which also serve to subdivide into blood group systems. The most important is the AB0 blood group system.
AB0 blood group system
Protein structures called antigens are found on red blood cells. Antigens are proteins that trigger an immune response in the body. Carriers with antigens of type A have blood group A, those of type B correspond to blood group B. If a person has both types of antigens, he has blood group AB. If there are no antigens, it is called blood group 0.
The antibodies in the blood plasma contain further components of the immune system, which in turn are directed against antigens. So that the immune system does not attack their own body, a person with blood group A, for example, does not have antibodies against type A antigens.
Rhesus blood group system
In the rhesus blood group system, a distinction is made as to whether the blood cells carry a certain protein (rhesus-positive) or not (rhesus-negative). About 85 percent of the people in Europe are rhesus positive, 15 percent rhesus negative.
Bedside test
There are three fields on pre-made test cards. These contain substances that react with antigens of type A, type B and with the rhesus factor. To do this, the doctor drips blood onto the individual test fields and mixes them up. The blood group can be deduced from the clumping (agglutination) that results. If the blood agglutinates, for example, on the type A field and the rhesus factor field (anti-D field), but not on the type B field, the patient has blood group A rhesus-positive.
The bedside test is carried out both with the recipient's blood and with the actual blood supply.
Cross match
In the cross match, the red blood cells of the blood reserve are mixed with the plasma of the recipient (major test) and the red blood cells of the recipient are mixed with the plasma of the blood reserve (minor test). Agglutinations must not occur here either.
Before the blood transfusion, the patient data is checked again to avoid mix-ups. The doctor will create a port in the vein that will allow the blood transfusion into the recipient's body. You will be monitored both during the blood transfusion and for at least half an hour afterwards. This also includes regular monitoring of blood pressure and heart rate. If you feel unwell, please inform your doctor immediately.
Further information: blood donation
If you would like to find out what you have to consider when donating blood and how it is carried out, read the article on blood donation.
Further information: Donate plasma
If you would like to find out what you have to consider when donating plasma and how it is carried out, read the article Donating plasma.
What are the risks of a blood transfusion?
Blood transfusion risks are rare, but mostly serious. In the so-called transfusion reaction, the donor's blood reacts with the recipient's blood due to an incompatibility of the blood groups. The immune system destroys the donor blood, which can lead to fever, anemia, jaundice, circulatory problems and kidney failure. The transfusion reaction can occur directly during the transfusion itself or it can be delayed.
In addition, allergic reactions can occur, which manifest themselves in fever, nausea, shortness of breath, drop in blood pressure, redness, itching and, in rare cases, shock. Although all blood products are carefully examined in accordance with the strict regulations of the Transfusion Act, there is still a certain risk of contracting HIV or hepatitis, for example.
If a patient receives a lot of red blood cell concentrates, the iron in the red blood cells can be deposited in the organs and cause cell and organ damage. The liver, heart, bone marrow and hormone-producing organs are particularly badly affected.
What should I watch out for after a blood transfusion?
After an outpatient blood transfusion, you are usually allowed to go home. If you notice symptoms such as nausea or circulatory problems, you should inform your doctor immediately. The success of the therapy is monitored with regular blood transfusions. It is particularly important to measure hemoglobin (red blood pigment) and iron with regard to iron overload caused by the blood transfusion. Side effects only occur when the organs are impaired in their function by the overload.
Tags: anatomy unfulfilled wish to have children menopause